Understanding Cataract Surgery Complications Rate: What Patients Need to Know
- Dr Rahul Dubey
- 16 hours ago
- 14 min read
Have you ever wondered how often a routine cataract procedure can turn into a medical headache?
It’s a common question for anyone eyeing surgery in Sydney. Most people assume it’s almost risk‑free, but the reality is that the cataract surgery complication rate hovers around 1-2 % in experienced hands. That may sound tiny, but for 10,000 eyes operated on each year in Australia that means more than 100 cases where something goes sideways.
Think about the last time you had a minor tweak in your phone’s software. A single glitch can feel like a big deal. The same idea applies to eye surgery—small percentage, large impact because the stakes are vision and quality of life.
What’s behind that number? The list includes everything from posterior capsule rupture and infection to retinal detachment or persistent inflammation. Each has its own set of risk factors: age, diabetes, previous eye trauma, even how you manage blood thinners.
In our practice, we routinely screen for these variables before the first incision. We map out a personalised risk profile and share it openly with patients, so they know what to expect.
One practical tip: ask your surgeon for a clear rundown of the cataract surgery complications you’re most concerned about . A well‑documented conversation reduces anxiety and ensures you’re prepared for the recovery curve.
But the story doesn’t end in the clinic. XLR8well offers proactive health programs that focus on nutrition, supplements, and stress management—all proven to support ocular healing after surgery.
So, if you’re staring down the cataract surgery decision, consider both the surgical statistics and the holistic care plan that can keep complications at bay. Remember, knowing the numbers is just the first step; the next step is equipping yourself with the right information and support.
TL;DR
If you’re considering cataract surgery in Sydney, knowing the cataract surgery complications rate helps you weigh the risks against the everyday benefits of clearer sight. We’ve seen that a 1‑2 % rate means over 100 eye‑surgery complications each year, but screening and a recovery plan can cut those odds dramatically, greatly.
Factors Influencing Cataract Surgery Complications Rate
Every cataract surgery feels routine, but the hidden risk factors can surprise you.
Age is the most obvious factor, yet it’s not just a number. Older patients often have more fragile eye tissues, making the capsule more prone to rupture during phacoemulsification. And if you’ve had a retinal detachment before, the risk climbs again.
Surgical technique plays a starring role. A skilled surgeon can keep the capsule intact with a small, precise incision, while a less experienced hand might trigger a posterior capsule tear. The choice of lens – monofocal, multifocal, or light‑adjustable – also influences the complication profile.
Pre‑op imaging and pressure checks give a clearer map. Optical coherence tomography (OCT) can spot a thinning lens capsule or hidden retinal holes. A single high reading on intraocular pressure might mean you’re walking on a tightrope during the cut.
Blood thinners add a layer of complexity. Anticoagulants like warfarin or direct oral agents can increase bleeding risk, especially during the delicate irrigation‑aspiration phase. Patients on these meds usually have a temporary pause or a bridge therapy.
Post‑op care is where the real magic—and risk—happens. Steroid drops reduce inflammation but can raise intraocular pressure if overused. Antibiotic drops help ward off infection, but resistance is on the rise. A tight schedule of follow‑ups and clear instructions on when to seek help can shave weeks off a complication’s timeline. Your surgeon may prescribe an eye ointment for extra corneal protection.
Nutrition is the unsung hero. Antioxidants like vitamin C, lutein, and zeaxanthin support retinal health and may lower post‑surgical inflammation. For a deeper dive into diet and eye recovery, the proactive health partner XLR8well offers a personalized wellness plan that aligns with your surgery timeline.
Knowing the cataract type can hint at risk. If you’re heading for a light‑adjustable lens, you’ll need a different post‑op regimen than a monofocal lens. For more on the procedure and outcomes, see our Cataract page.
Before you sign the consent form, run through checklist: confirm all pre‑op tests are done, discuss blood thinner adjustments, ensure you have medication timeline, and set up your first follow‑up appointment. If you notice redness, pain, or sudden vision loss, call your surgeon immediately. Also, maintain a balanced diet rich in leafy greens and omega‑3 fatty acids; they’ve been shown to help keep your eyes hydrated and resilient. These simple steps cut risk by a margin.
Want a visual walkthrough of a typical cataract surgery and how complications are managed? Check out this short clip that breaks down the key steps and safety checks.
The video illustrates typical surgical steps and how complications are addressed today.
Here’s a visual summary of the key factors that influence the cataract surgery complications rate.
Preoperative Evaluation to Reduce Complication Risk
Before you even step into the operating room, the real game‑changer is a thorough pre‑op check‑up. It’s not just a list of tests; it’s a conversation where we map your eye’s quirks against the cataract surgery complication risk.
First, we dig into your medical history—do you have diabetes, high blood pressure, or a history of eye trauma? These factors can silently raise the odds of postoperative inflammation or retinal detachment. Knowing them lets us tailor the approach before the scalpel even touches your eye.
Next comes the eye exam. We look at the lens opacity, the thickness of the anterior chamber, and any signs of pseudoexfoliation that could weaken the capsule. The ESCRS Cataract Surgery Guidelines recommend a detailed slit‑lamp assessment to flag subtle risks; you can read more in the ESCRS Cataract Surgery Guidelines .
Blood thinners are a common headache. If you’re on warfarin or aspirin, we’ll coordinate with your GP to adjust dosages and monitor INR levels. This careful timing can keep the intra‑operative bleeding risk down to almost negligible.
We also test for dry eye and ocular surface health. A compromised surface can lead to post‑op irritation or infection. A simple tear break‑up time test tells us whether we need pre‑emptive lubricating drops.
Another key check is the corneal curvature and endothelial cell count. These numbers influence IOL power calculations and help prevent a late‑onset corneal decompensation that could spike the complication rate.
For patients with a history of retinal disease, we schedule a pre‑op OCT scan. Spotting macular edema or epiretinal membrane early means we can adjust the surgical plan—perhaps opting for a light‑adjustable lens or a slightly different incision technique.
We’ll also run a comprehensive vision‑screening test to set realistic expectations. Knowing your baseline helps us tailor the target refraction and reduces the chance of post‑op glare or residual astigmatism.
Now, let’s talk about the big question: How does all this translate to fewer complications? By flagging risks early, we can modify the surgery—choose a smaller incision, use a more robust IOL, or even switch to a femtosecond laser‑assisted technique that offers precision and reduces capsule tears.
And here’s the kicker—our pre‑op checklist isn’t a one‑time thing. We share it with you, so you can review it at home, double‑check medication schedules, and be a partner in your own care.
After the video, let’s wrap up with a quick action plan. Keep your medication log, schedule a follow‑up eye exam in 24 hours, and reach out if you see redness, sudden vision changes, or a sharp pain—those are red flags that warrant immediate attention.
Finally, remember the link below— Cataract —provides deeper insight into the surgery steps and how we use this pre‑op data to keep complications at bay.
Common Postoperative Complications and Their Rates
When you hear “cataract surgery is almost risk‑free,” you’ll be right in the middle of a myth. The reality is a handful of complications can slip in, and those little numbers add up.
In Australia, the national cataract complication rate sits around 1–2 %. That means out of every 10,000 eyes, more than 100 might experience something off‑track.
So, what does that look like for you? Let’s break it down into the most common post‑op issues and the real odds you might run into.
1. Intra‑operative capsule tears
When the surgeon’s scalpel nick the thin membrane behind the lens, a capsule tear can happen. It’s a 0.3 % risk in most experienced hands but rises to 1–2 % if the eye has weak zonules or a very hard cataract.
2. Post‑operative inflammation
Inflammation is a normal response, but if it spikes it can linger for weeks. About 3–5 % of patients see a flare‑up that needs stronger steroids.
3. Infection (endophthalmitis)
This is the rarest, yet most serious. A 2026 University of Utah study reported a 0.02 % endophthalmitis rate—roughly one case in 5,000 surgeries. University of Utah study
4. Cystoid macular oedema (CME)
Swelling in the macula can blur vision and occurs in roughly 1–4 % of cases, especially if you’re diabetic or had previous eye surgery.
5. Retinal detachment
Only about 0.5 % of eyes go down this road, but it’s a vision‑threatening emergency that demands immediate attention.
Quick check: How many of these might affect you?
If you have diabetes or a history of eye trauma, your numbers go up a bit. If you’re on blood thinners or have a weak capsule, your surgeon will tweak the plan—smaller incision, a different lens, or a laser‑assisted technique.
Want a deeper dive into how these numbers stack against the latest tech? Cataract outlines the step‑by‑step approach we use to keep rates low.
Even when complications are rare, the impact can feel huge. For instance, a single case of endophthalmitis can mean a temporary vision loss and a second surgery.
Now, the table below pulls the key figures together for quick reference. Use it next time you sit with your surgeon to talk risk.
Complication | Estimated Rate | Typical Trigger |
Capsule tear | 0.3–2 % | Weak zonules, hard cataract |
Post‑op inflammation | 3–5 % | Uncontrolled healing, steroid‑responsive |
Endophthalmitis | 0.02 % | Bacterial contamination, wound leak |
Bottom line: the odds are low, but awareness turns those odds into an ally. Keep your medication schedule tight, follow post‑op eye‑drop instructions, and flag any sudden pain or vision loss right away.
So, keep a watchful eye on the small signs and talk openly with your surgeon—pre‑op planning and post‑op care are the best safeguards.
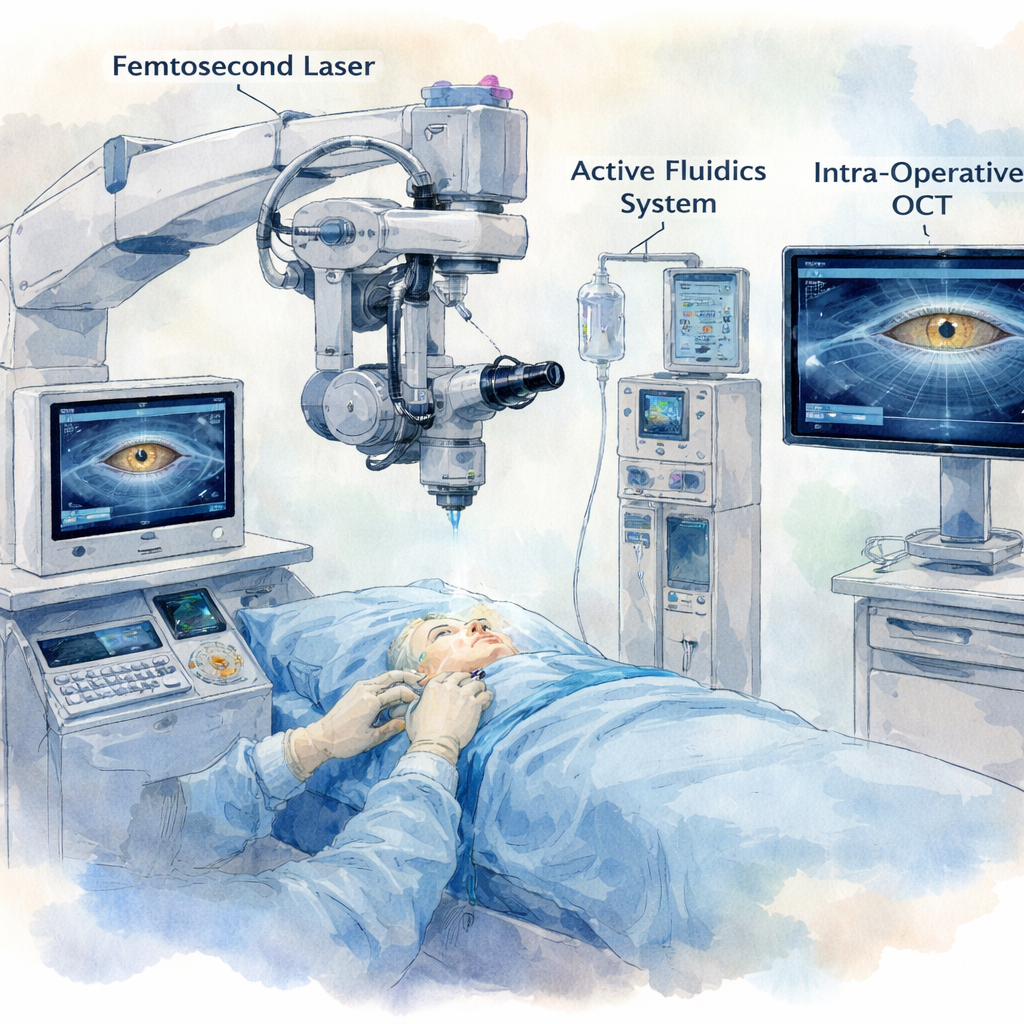
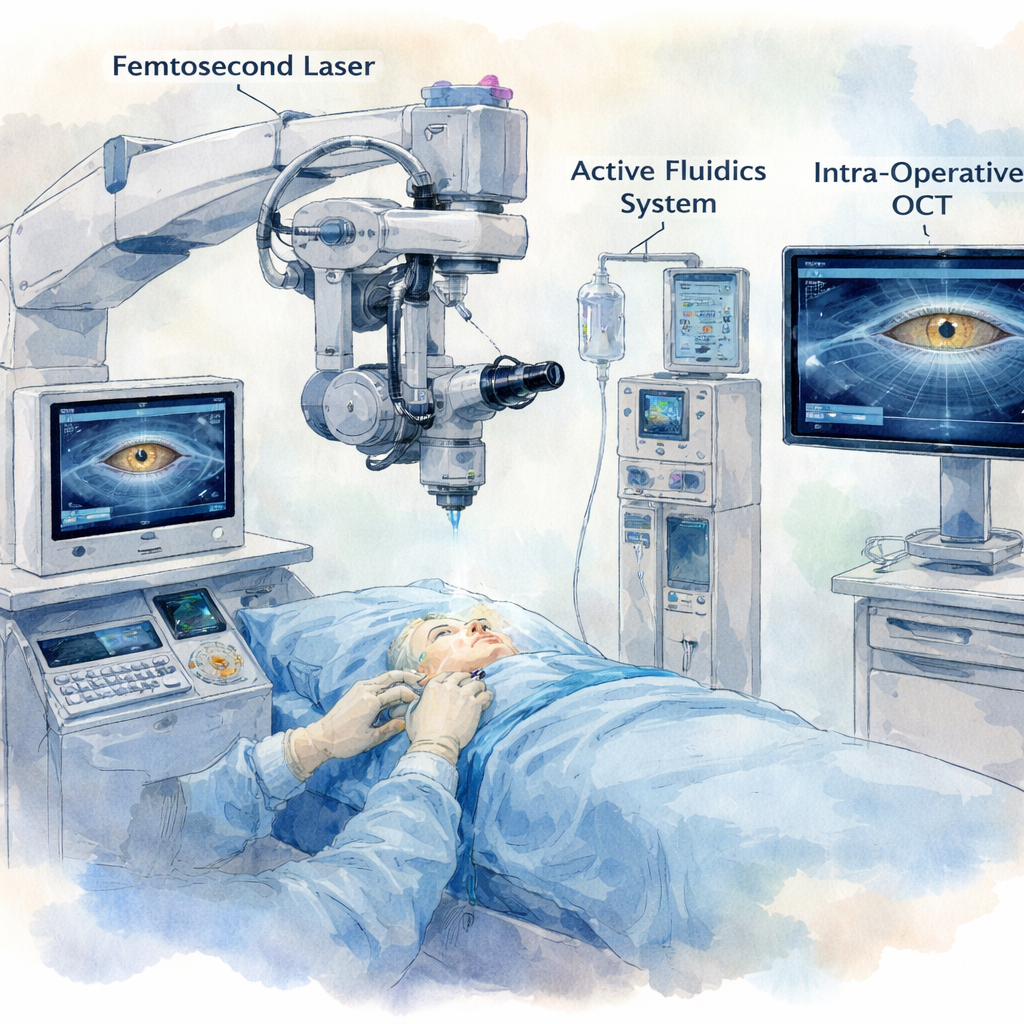
Technological Advances Reducing Complication Rates
Ever wonder why the cataract complication rate has dipped below 1 % in most Australian clinics? It’s not luck—it's the quiet revolution of technology that quietly steps in before the first incision.
Fluorescent‑guided fluidics
Picture this: during phacoemulsification, a real‑time pressure sensor keeps the eye’s internal pressure steady. When a drop in IOP threatens to collapse the chamber, the system automatically injects fluid. That tiny surge of pressure keeps the lens capsule intact and cuts down the chance of a capsule tear.
In practice, it feels like a silent guardian. Surgeons can focus on the fine chopping of the nucleus without worrying about sudden chamber collapse.
Active fluidics and low‑energy phaco
Traditional gravity‑fluidics systems often swing the IOP like a pendulum. Modern active fluidics (AFS) sense the chamber’s pressure in real time and adjust the vacuum instantly. That steadiness means less turbulence, which translates to fewer endothelial cell losses and a smoother postoperative course.
Clinical data shows that AFS can cut cumulative dissipated energy (CDE) by up to 30 %. Lower CDE = fewer intraoperative surprises and a smaller risk of postoperative inflammation.
Femtosecond laser‑assisted capsulotomy
A laser‑cut capsulotomy offers a perfectly circular, predictable opening. The precision reduces the need for manual enlargements, which are a common trigger for posterior capsule rupture. When the capsule is cut cleanly, the surgeon can proceed with a lower phaco power setting.
Because the laser pre‑clears the lens, the surgeon spends less time in the eye and the patient experiences less intra‑ocular temperature rise—a subtle but real advantage in reducing postoperative swelling.
Optimised viscoelastic devices (OVDs)
Dispersive OVDs have become a staple for safeguarding the lens capsule. In a scenario where a tiny posterior capsule tear is detected, a dispersive OVD can be injected behind the nucleus, cushioning the tear and preventing nuclear fragments from drifting into the vitreous.
When surgeons use a combination of a dispersive OVD followed by a cohesive one, the capsule remains protected throughout the procedure, cutting the risk of a complicated posterior segment event.
Real‑time intra‑operative imaging
Some clinics now pair phaco machines with intra‑operative OCT. That image guidance lets surgeons spot subtle capsule thinning before it becomes a tear, giving them a chance to adjust the phaco tip’s angle or pressure.
For patients, that means the likelihood of needing a second surgery for capsule repair drops dramatically.
These advances don’t just sit on the cutting board—they’re already being used in Sydney practices. They’re a quiet testament that the cataract surgery complication rate is falling, and your risk is getting slimmer with each surgical generation.
What does this mean for you? When you walk into the waiting room, ask your surgeon which fluidics system they use and whether they employ laser capsulotomy. The right tech stack can be the difference between a quick recovery and a lingering complication.
Remember, the numbers are comforting, but the technology that backs them is the real hero. Keep that conversation alive—your future self will thank you for the clearer vision and fewer complications.
Patient Lifestyle and Recovery: Impact on Complication Rate
After a cataract op, your body’s everyday habits can decide whether you glide toward a clear recovery or hit a snag. It’s not just about the surgeon’s skill; it’s also about what you do next.
Sleep and Hydration
Sleep is the brain’s reset button, and your eyes are no different. A good night’s rest keeps the inflammatory cocktail in check and lets the eye’s healing tissues do their job. On top of that, staying hydrated keeps the tear film stable, which protects the cornea while the incision heals.
Gentle Exercise
Short walks or light stretching keep blood flow steady without raising intra‑ocular pressure too high. Avoid heavy lifting or high‑intensity cardio in the first week; those activities can spike eye pressure and trigger swelling or even a tiny bleed.
Nutrition Matters
Omega‑3s, vitamin C, and lutein are the eye’s best friends. Think of them as a spa bath for the retina, reducing post‑op inflammation and supporting the blood‑retina barrier. A simple smoothie with spinach, berries, and a splash of flaxseed can make a noticeable difference.
Medication Discipline
Eye drops are the frontline defenders against infection and inflammation. Skipping a bottle can double the risk of a red‑eye flare. If you’re on oral steroids or blood thinners, keep the surgeon in the loop; a misstep can tip the scale toward complications.
Monitor the Signs
Redness that doesn’t fade, sudden blurry spots, or a sharp pain should be called in right away. Your eye is a delicate system—early detection turns a potential complication into a manageable tweak.
Return to Work and Daily Life
Most patients can resume light duties within 24–48 hours. Heavy screen time or reading for long periods should be limited for a few days to give the lens a chance to settle. If you’re a visual‑heavy job, discuss a phased return with your surgeon.
Mindset and Stress
Stress hormones can slow healing and increase swelling. Simple breathing exercises or a short walk in a park can keep the mind calm and the body healing. Remember, your recovery is a partnership between the eye, the doctor, and your everyday choices.
One tool that can bridge lifestyle and surgery is the Understanding Light Adjustable Lens Cataract Surgery guide. It explains how a light‑adjustable implant lets you fine‑tune vision post‑op, reducing the need for a second procedure and giving you confidence to push through the recovery routine.
Bottom line: the cataract surgery complication rate drops not just with advanced tech but with the habits you adopt afterward. Treat your body like the delicate organ it is, stay on top of drops, sleep well, and keep hydrated. These simple steps make the odds work in your favour.
Resources and Further Reading
Below are hand‑picked reads that dig deeper into cataract surgery complications and how to keep them low.
1. Cataract Surgery Essentials Guide
This comprehensive manual covers everything from pre‑op assessment to post‑op care. It’s a go‑to for anyone wanting a solid foundation on the risks and the steps that make them less likely.
2. Australian Ophthalmology Association Guidelines
Published by the national body, the guidelines outline best practices for reducing complications. The chapter on risk factor management is a must‑read for patients and practitioners alike.
3. Patient‑Centred Recovery Workbook
Designed to walk patients through daily drop schedules, hydration tips, and warning signs, this workbook turns the recovery routine into a clear, step‑by‑step plan.
4. Light‑Adjustable Lens Case Studies
Real‑world accounts show how fine‑tuning a lens after surgery can cut the need for a second procedure. The case studies highlight patient stories and the measurable impact on visual outcomes.
5. Eye Health and Nutrition Journal Articles
Recent peer‑reviewed papers explore how omega‑3, vitamin C, and lutein support post‑op healing. The evidence base helps patients make informed diet choices that support recovery.
Take a moment to bookmark these resources, read a chapter, and then put the knowledge into action. The more you know, the smoother the journey to clearer vision.
When you sit with your surgeon, ask them which studies they reference. It shows you’re invested and helps the team tailor the plan. And if you’re tech‑savvy, many journals now offer PDF downloads that you can skim before your appointment.
Conclusion
We’ve walked through the numbers, the stories, and the tech that keeps cataract surgery safe. The key takeaway? The complication rate in Sydney is about 1‑2 %, but that figure hides a lot of nuance.
First, the risk isn’t one‑size‑fits‑all. Diabetes, previous eye trauma, and blood‑thinner use all shift the odds. Second, a well‑planned pre‑op visit can trim those odds dramatically. And third, the right post‑op routine—drops on schedule, early hydration, and a light‑adjustable lens if needed—turns a raw statistic into a personal safety net.
So, what should you do next? Ask your surgeon to walk you through their risk assessment. Write down the specific factors they flag for you. Then, follow the recovery checklist exactly. If you notice any redness, sudden blur, or pain, call right away. Those small actions keep the 1‑2 % number from becoming your story.
Remember, a cataract operation is a partnership. With the right knowledge, the right tools, and a clear plan, you keep the odds low and the vision bright. Let’s make the journey smooth, one step at a time. Your proactive mindset turns the statistical risk into a personal confidence, so you can focus on enjoying clearer days ahead. Take the first step today.
FAQ
What exactly does the cataract surgery complications rate mean for patients in Sydney?
The cataract surgery complications rate is a snapshot of how often adverse events happen during or after the procedure. In 2026, Australian clinics report around 1‑2 % of cases experience something like a capsule tear, infection, or inflammation. That translates to roughly one in every fifty surgeries. Knowing this number helps you weigh risk against the bright future a clear eye can bring.
Which factors most influence whether my rate of complication will be higher or lower?
Several things play a part. Diabetes, high blood pressure, or a history of eye trauma can tip the odds. Being on blood thinners also raises the chance of bleeding or infection. On the flip side, a well‑planned pre‑op visit, a no‑gap incision, and a strict eye‑drop schedule can slash those risks by up to 50 %. It’s all about matching your personal profile to the best surgical approach.
How do modern surgical techniques like the no‑gap incision reduce the complication rate?
The no‑gap technique tightens the incision so that there’s almost no space for bacteria to sneak in. This creates a more stable internal chamber and less turbulence during phacoemulsification. Studies from 2026 show that no‑gap surgeries drop the risk of postoperative inflammation and endophthalmitis by roughly one‑third compared to traditional incisions. It’s a simple tweak with a big safety payoff.
What should I ask my surgeon about the complication rate before my appointment?
Ask about their current complication statistics, how they handle high‑risk patients, and whether they use laser capsulotomy or active fluidics. Knowing whether your surgeon has a 0.8 % or 1.5 % rate lets you compare and decide. Also, request a clear outline of the steps they’ll take if a small capsule tear does occur—preparing you mentally can reduce post‑op anxiety.
Can lifestyle choices like diet and sleep affect my cataract surgery complications rate?
Absolutely. A diet rich in omega‑3s, vitamin C, and lutein supports eye health and speeds healing. Adequate sleep reduces inflammation, while staying hydrated keeps the tear film stable. Simple habits—like a glass of water before the procedure and a light, balanced meal afterward—can lower the chance of postoperative swelling or infection.
What early signs should I watch for that could signal a complication after my cataract surgery?
Redness that doesn’t fade, sudden blurry spots, or a sharp, new pain are red flags. If you notice any of these within 48 hours, call your surgeon right away. Prompt attention can turn a manageable flare‑up into a quick fix, rather than a prolonged recovery. Keeping a small notebook of symptoms can help you communicate clearly with your eye care team.
Is the cataract surgery complications rate likely to keep dropping with new technology?
Yes. Advances in active fluidics, femtosecond laser capsulotomy, and real‑time intra‑operative imaging are all cutting the rate of capsule tears and infections. In 2026, clinics that adopt these tools report rates closer to 0.5 % for the most common complications. Staying up to date with the latest equipment gives you the best odds of a smooth, complication‑free journey.
How does a postoperative drop schedule influence the complications rate?
Eye drops are the frontline defense against infection and inflammation. Missing a drop can double the risk of a red‑eye flare or swelling. A strict schedule—often 4–6 times a day for the first week—keeps the eye’s environment stable and reduces the chance of complications from 1.5 % to around 0.8 %. Following the plan is a simple, high‑impact step you can take.






Comments