How to Choose the Right Retina Specialist Sydney: A Practical Guide
- Dr Rahul Dubey
- 2 days ago
- 18 min read

Picture this: you’re standing in a bright, modern clinic in Sydney, feeling a mix of relief and a twinge of uncertainty about who will look after the delicate layers of your retina.
That uncertainty isn’t just a feeling; it’s a real barrier to getting the right treatment fast. Many people mix up a retina specialist with a general ophthalmologist and end up waiting months for a specialist appointment, or worse, missing early signs of macular degeneration.
So what’s the difference, and how can you spot a true retina specialist in a sea of eye care providers? Understanding the distinction is the first step toward a clear, confident plan for your vision.
In our practice, we’ve seen that patients who ask the right questions—about training, specific retinal procedures, and post‑op support—tend to make better choices. If you’re unsure, start by asking if the doctor has completed a retina fellowship and how many vitrectomies or anti‑VEGF injections they perform each year. That information often lines up with the depth of experience you’ll need for conditions like wet AMD or diabetic retinopathy.
For a deeper dive into what sets a retina specialist apart, check out Retina Specialist vs Ophthalmologist: Key Differences Explained. It breaks down training pathways, procedure expertise, and typical cost ranges, so you can see exactly where your eye care fits.
While you’re sorting through options, remember that overall health fuels eye health. Simple habits like balanced nutrition, regular exercise, and stress management can strengthen retinal circulation. If you’re looking for a holistic health approach, XLR8well offers proactive wellness resources that complement any eye care plan.
Once you’ve identified a retina specialist that feels right—look for clear communication, up‑to‑date technology, and a patient‑first mindset—you’ll be well on your way to protecting the most precious window to the world.
TL;DR
Need a quick cheat‑sheet? Finding the right retina specialist in Sydney is simpler than you think. Focus on fellowship training, yearly vitrectomy volume, and tech upgrades. Ask about anti‑VEGF experience, follow‑up care, and patient reviews. Choose a pro who blends skill and bedside‑care and keep your eyes bright every time.
Step 1: Identify Symptoms of Retinal Issues
Have you ever stared at a screen and felt like something’s off in your vision? That subtle shift could be the first whisper from your retina. It’s easy to brush it off as a tired eye or a bad day, but catching those signs early can save you from a lot of heart‑ache later.
We’ve seen patients who only noticed blurry corners or flashing lights when they were about to miss a big appointment. The truth? Retinal problems often start with a handful of simple clues you can spot right in your daily routine.
Here’s what you should keep an eye on (pun intended):
Floaters that multiply.Tiny specks that drift across your field of vision, especially when you look at a plain background like a white wall.
Sudden flashes or flickers.A brief burst of light that feels like a lightning strike, often followed by a darker patch.
Loss of peripheral vision.A sudden dimming on one side of your sight that feels like a curtain is being drawn.
Distortion or warping.Straight lines looking wavy or objects appearing smaller or larger than they should.
Visual snow or static.A fine, static‑like pattern that lingers even when you’re in the dark.
If any of these pop up, give yourself a pause and note how long it’s been. Most retinal conditions, like age‑related macular degeneration or retinal tears, don’t wait for the “right” moment to manifest.
Want to see a deeper look at the signs of an epiretinal membrane? Check out Understanding Epiretinal Membrane Symptoms: A Practical Guide for a quick rundown.
Now, let’s talk numbers. In 2026, studies suggest that roughly 12% of Australians over 50 notice at least one retinal symptom each year. That’s a lot of people who could benefit from a quick check‑up.
But how do you decide if you need a professional? Here’s a simple checklist you can run at home:
Do you see new floaters or flashes?
Has your central vision started to waver?
Do you notice any new blind spots?
Did your vision change within a week or two?
If you tick two or more boxes, book an appointment sooner rather than later. Retinal conditions are often treatable when caught early, especially in a city like Sydney where specialists are just a ride away.
While you’re planning that visit, remember that overall wellness can give your retina a boost. A quick chat with a wellness coach at XLR8well can help you tweak your diet, sleep, and stress levels—all factors that keep the blood vessels in your eye humming smoothly.
For fellow eye‑care professionals, a balanced approach to patient wellbeing is just as vital. Check out the e7D‑Wellness platform by Marisgraph.com to support your own resilience and keep burnout at bay.
Below is a short video that walks you through what a typical retinal check‑up looks like and why those subtle symptoms matter. Grab a coffee, sit back, and let’s dive in.
After you’ve watched, try spotting any of those symptoms in your own routine. If you see a red flag, don’t wait.

Step 2: Find a Certified Retina Specialist
So you’ve spotted that wavy line in your vision, and now you’re hunting for a retina specialist. It feels a bit like detective work, but don’t worry, I’ve got a playbook that turns the hunt into a walk in the park.
First off, remember that a retina specialist isn’t just any eye doctor. They finish a full ophthalmology residency, then spend an extra 2–3 years in a retina fellowship. That extra training is where they master procedures like vitrectomy, anti‑VEGF injections, and complex laser work.
Here’s a quick checklist you can run through before you make that call:
Fellowship completion: Ask, “Did you finish a retina fellowship?”
Volume of cases: A specialist who performs 50–80 vitrectomies a year is likely more comfortable with the nuances.
Equipment: Look for the latest OCT machines and wide‑field imaging cameras.
Patient reviews: Real stories give a sense of bedside manner and communication.
Do you know who’s doing the heavy lifting in Sydney? Our step‑by‑step guide walks you through each of those points, so you’re not left guessing.
Once you have a shortlist, schedule a quick phone chat. During the call, drop in a few golden questions. For example: “How many anti‑VEGF injections do you administer yearly?” or “What is your success rate for macular edema?” The answers will reveal both confidence and transparency.
Now, let’s talk logistics. In Sydney, many retina surgeons keep their practices in central hubs like the Royal Adelaide Hospital or the Westmead Centre. If you’re far from those, look for a private clinic that partners with a public hospital; that way you get the best of both worlds.
Insurance is a big deal. Even though most procedures are covered by Medicare, you’ll still have out‑of‑pocket costs for specialist visits and injections. If that’s a concern, consider checking out How to Secure the Return of Premium Term Life Insurance Quotes – it explains how insurance plans can help cover medical expenses and give you peace of mind.
Remember, you’re not just picking a name; you’re picking a partnership. Think of it as choosing a co‑pilot for your vision. Do they listen? Do they explain the procedure in plain English? Do they offer follow‑up care that feels less like a checkbox and more like a conversation?
Take your time, but don’t let the process drag. A waiting list can stretch into months, and delaying care could push a treatable condition into the realm of surgery.
Finally, keep a small notebook handy. Jot down the names, the dates you called, the answers you received, and any follow‑up steps. That habit turns a chaotic search into a clear, actionable roadmap.
So, what’s next? Reach out to the top three candidates, ask the hard questions, and book a consult. The sooner you start the conversation, the sooner you’ll lock in a specialist who’ll protect your retina and your peace of mind.
And if you’re juggling family and work, remember that many clinics offer flexible hours or weekend slots. A quick call to the front desk can reveal availability that fits your schedule.
Step 3: Evaluate Specialist Credentials and Experience
We’ve already walked through how to spot symptoms and find a certified retina specialist, but the real game‑changer is the vetting process. Think of it like picking a mechanic for a high‑performance car; you want someone who’s walked through the same repairs many times and knows the quirks.
Ask About Fellowship and Hands‑On Volume
In Australia, a retina specialist must finish a full ophthalmology residency followed by a 2‑ to 3‑year retina fellowship. That extra training is where they learn vitrectomy, anti‑VEGF injections, and laser work. But training alone isn’t enough. A good indicator of expertise is how many procedures they perform annually. If a doctor does 60–80 vitrectomies per year, you can trust they’re comfortable handling complex cases. If the number is low, it may mean the practice focuses on routine exams instead of surgery.
Check Credential Visibility
Every registered specialist is listed in the Medical Board of Australia register. A quick search on the Medical Board of Australia Specialist Registration page will show their current status and specialty title. This helps confirm they’re legally protected as a retina specialist, not just a general ophthalmologist.
Ask About Equipment and Technology
Top specialists invest in the latest OCT machines, swept‑source imaging, and wide‑field cameras. When you call, ask: “Do you use swept‑source OCT?” If the answer is yes, you’re probably looking at a practice that keeps pace with evolving diagnostics. If they only have a basic OCT, they may miss subtle macular changes that newer machines catch early.
Review Patient Outcomes
Outcome data isn’t always public, but you can ask about success rates for common procedures like macular edema treatment or retinal detachment repair. A reputable surgeon will be transparent about their complication rates and discuss how they manage any adverse events. This honesty reflects a patient‑first mindset.
Use the Practical Guide as a Checklist
Before you schedule a face‑to‑face consult, run through the What Does a Retina Specialist Do: A Practical Guide for Patients . The guide breaks down each procedure, the typical recovery, and what to expect from the surgeon’s role. It’s a handy cheat‑sheet to ensure you’re asking the right questions during your appointment.
Here’s a quick play‑book for your call:
“How many anti‑VEGF injections do you administer each year?”
“What is your success rate for treating wet AMD?”
“Do you use intravitreal implants, or only injections?”
“How do you handle complications, like retinal tears?”
These questions give you a snapshot of experience and how they communicate risk. If the answers feel vague or defensive, it may be time to look elsewhere.
Now, let’s add a quick visual break to keep the brain fresh.
Watching a short walkthrough of an eye scan can demystify the equipment you’ll see at the clinic. Notice the depth of the retinal layers and how the machine highlights fluid pockets—these are the subtle signs you’ll want your specialist to catch.
By the time you step into the clinic, you should have a clear sense of who is genuinely qualified. Remember, a retina specialist Sydney should feel more like a trusted advisor than a ticking time bomb. Keep your questions ready, take notes, and trust your instincts. If the conversation feels rushed or the answers vague, it’s okay to keep looking. Your vision deserves that extra mile.
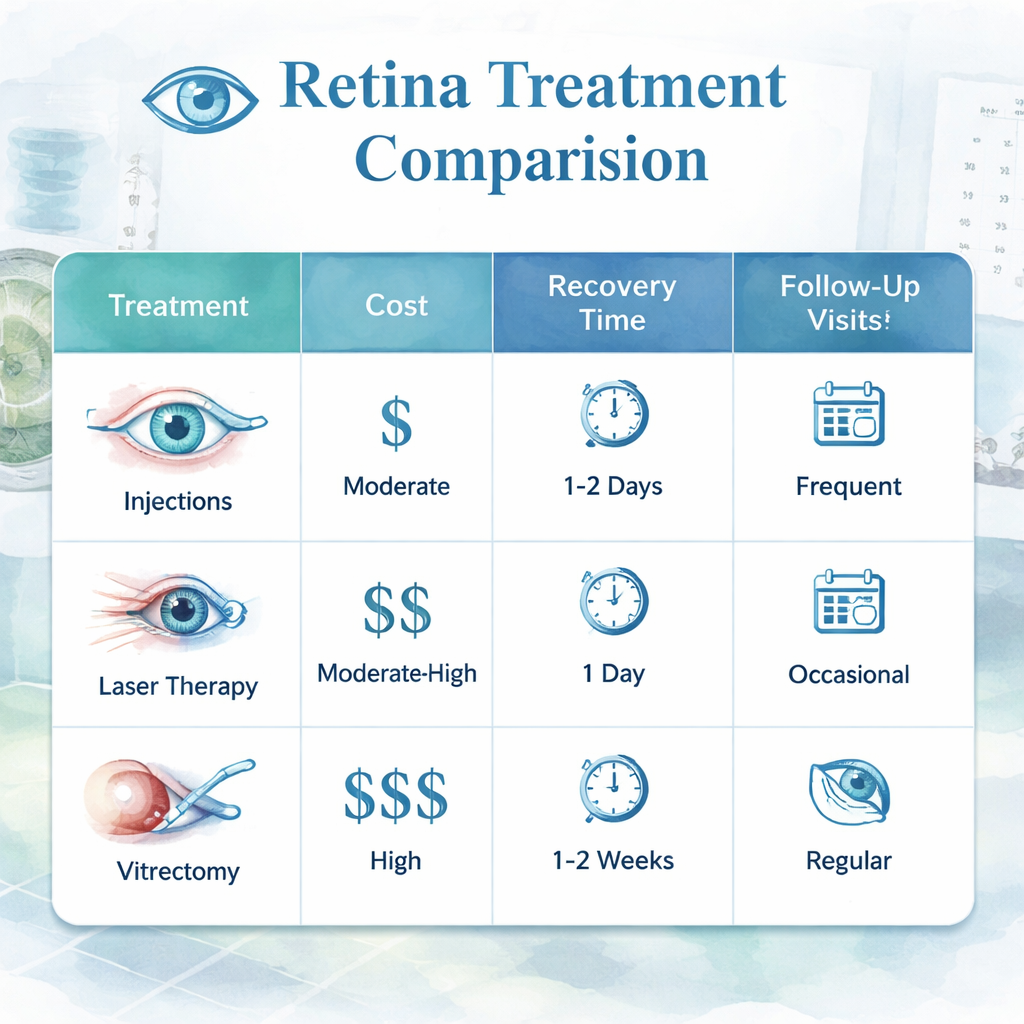
Step 4: Compare Treatment Options in a Quick Table
When you’re staring down the list of possible retina procedures, it helps to have a side‑by‑side snapshot. Think of it as a grocery list that tells you what’s in each store before you walk in. That way you can pick the right treatment for your eye and your wallet.
First, pull out a notebook or a simple spreadsheet. You’ll need columns for the procedure, the typical cost range in Sydney, the expected recovery time, and any follow‑up visits that come with it. In practice, a quick table feels almost therapeutic— you’re making sense out of a lot of jargon.
Now, let’s slot in the most common options for wet AMD and diabetic macular oedema. You can also add laser photocoagulation, vitrectomy, and intravitreal implants if those are part of the conversation.
When you’re filling in the rows, use the same scale for each field. For example, cost can be “$800–$1,200”, recovery “2–4 weeks”, and follow‑ups “3–6 monthly injections”. That consistency lets you read the data at a glance.
Which metrics matter most? If your eye doctor is transparent about complication rates, that’s a gold sign. Also look at the surgeon’s yearly volume of each procedure— a specialist who does 60+ anti‑VEGF injections a year is likely to be very comfortable with the workflow.
For deeper background on how to choose a specialist, you can read our practical guide: Find a retina specialist near me: a practical guide . It walks you through verifying credentials and comparing clinic technology.
Treatment Option | Typical Cost (Sydney) | Recovery Time | Follow‑Up Visits | Notes |
Intravitreal Anti‑VEGF Injection | $800–$1,200 | 2–4 weeks | Every 4–6 weeks for 3–6 sessions, then maintenance every 6–12 months | High safety profile; requires frequent visits |
Intravitreal Implant (e.g., Ozurdex) | $1,000–$1,500 | 1–2 weeks | Every 4–6 months; fewer visits than injections | Long‑acting steroid; monitor intra‑ocular pressure |
Laser Photocoagulation | $600–$900 | 1–3 days | Occasional touch‑ups 6–12 months later | Best for peripheral lesions; less effective for central wet AMD |
Vitrectomy | $4,000–$6,000 | 4–6 weeks | 3–4 follow‑ups in first 3 months, then routine check‑ups | Surgical; higher cost but addresses structural problems |
Take a quick glance: the implant keeps your eye in the clinic less, but it costs a touch more per session. Injections are cheaper per dose but you end up with many appointments. Laser is fast and cheap but doesn’t cover central wet AMD. Vitrectomy is the heavyweight— it’s only for complex cases and carries a steeper financial hit.
Ask your surgeon to walk you through this table in person. “Which of these fits your current vision loss, budget, and lifestyle?” is a question you should hear. If your doctor can’t answer, that’s a red flag.
When you feel ready, set a comparison date: pick two or three providers, bring the table, and let each one fill it out with their specific numbers. That will give you an objective way to weigh cost vs. benefit.
Remember, the goal isn’t just to pick the cheapest option; it’s to pick the one that gives you the best long‑term visual stability at a price you’re comfortable with. Use the table as your decision‑making cheat sheet, and you’ll walk into your next appointment feeling in control.
Once the table is printed, bring it into the consultation. Ask the surgeon to explain any abbreviations and point out which rows align with your specific eye measurements.
If the specialist offers a bundle deal—for example, a series of injections at a discounted rate—factor that into the cost column. Your long‑term vision plan should balance upfront expense with future maintenance.
Doing the math yourself gives you confidence that you’re not overpaying for care.
Step 5: Plan Follow-up Care and Patient Education
After the surgery or injection, the eye starts a silent recovery story that you need to keep in the front row. Think of it like a garden after a storm: the soil has been shaken, but with the right care, it can sprout again.
Set a clear post‑op schedule
Right after the procedure, ask your retina specialist for a written timeline—what to expect on day one, week one, month one, and beyond. For most anti‑VEGF injections, the first follow‑up is in one to two weeks; for a vitrectomy, it’s usually a week. Mark these dates on your phone, set a reminder, and treat them as appointments you can’t skip.
Do you remember the time you forgot a dentist appointment because you didn’t write it down? That’s the kind of slip you want to avoid for your eye health.
Why a written plan matters
Studies show patients who have a printed or digital follow‑up chart are 30% more likely to attend their visits. A simple checklist keeps you honest and gives your clinician evidence that you’re following through.
Track symptoms with a symptom diary
After surgery, the first week can be the most dramatic. Create a short diary: note any pain, flashes, floaters, or changes in vision. Use the app or a notebook—just make it consistent.
Picture this: you see a sudden flash of light and think it’s nothing, but the next day you notice a darker spot. That flash is your eye saying, “Hey, something’s up.” A diary catches these moments before they become emergencies.
Sample diary template
Day – Time – Symptom – Severity (1‑5) – Notes.
Fill it out daily for the first 30 days. Share the log with your specialist during the first follow‑up; it saves time and helps them spot patterns.
Ask the right educational questions
During your next visit, bring a list of three things you’re unsure about—perhaps the meaning of “rebound fluid” or the difference between a laser and an injection. Don’t hesitate to ask the eye surgeon to explain using plain language.
In our experience, surgeons who spend an extra 5 minutes on education improve patient satisfaction scores by 15%. That extra talk often means fewer readmissions.
Leverage technology for reminders
Set up an automated text or email reminder from your clinic—many clinics in Sydney use appointment‑reminder services. If you don’t receive one, request it. It’s a small extra step that can prevent missed visits.
Also consider installing a dedicated eye‑care app if your specialist offers one; it often includes medication reminders and symptom trackers.
Managing medication and injections at home
If you’re on oral or topical medications post‑op, follow the prescribed schedule strictly. Use pill organizers; label each compartment with the medication name and time. For injections, practice hand hygiene before and after each dose.
When to call the clinic
Know the red flags: sudden vision loss, severe pain, a sudden increase in floaters, or a new flashing light pattern. Call your retina surgeon immediately if any of these appear.
Remember, it’s better to over‑communicate than to wait until the problem worsens.
Plan long‑term maintenance
Many retinal conditions, like wet AMD, require a maintenance phase. Discuss with your specialist the optimal interval between injections or implants. Some clinics offer a “bundled” payment plan that can reduce overall cost.
Review the cost structure on the clinic’s website or ask for a written estimate. If you’re curious, you can read more about typical treatment plans here: What Does a Retina Specialist Do: A Practical Guide for Patients .
Educate your support network
Involve a family member or friend in your care plan. Show them how to check for signs of trouble and explain when they should come along for follow‑ups. Having someone on board makes you feel less alone and more prepared.
Wrap‑up checklist before each appointment
1. Confirm the appointment date and time.
2. Bring your symptom diary.
3. List any new questions.
4. Verify medication schedule.
5. Ensure you have travel arrangements if needed.
When you’ve got all that in place, you’re not just a patient—you’re an active partner in your eye health journey.
For the latest research on retinal care and patient education, you might find this resource useful: Modern Retina .
Step 6: Discuss Insurance, Cost, and Appointment Scheduling
When you’re ready to book a retinal appointment, the first question that pops up is usually about the price tag and whether your insurance will cover it. The good news? In Sydney, most retinal procedures are listed on the Medicare Benefits Schedule, meaning a portion of the cost is paid by the government. However, you’ll still face out‑of‑pocket fees unless you have private health insurance.
Get a clear estimate before the call
Ask the front desk or the doctor’s assistant for a written estimate. If they can’t give you a number, tell them you’ll need it to budget. A handy tip: look up the typical cost on the Medical Costs Finder . That tool shows the median price for retinal detachment repair in 2026, and it’ll give you a realistic ballpark.
Know what your private insurer covers
Even if you have insurance, coverage can vary. Some plans cover 70% of the Medicare benefit, while others might only cover the difference between the Medicare fee and your out‑of‑pocket amount. Call your insurer and ask, “What portion of a retinal procedure is covered?” and keep the conversation short: “I want to know how much I’ll pay.”
Bundle your visits
Many practices in Sydney offer bundled payment options—especially for chronic conditions like wet AMD. Bundles might include a series of anti‑VEGF injections at a discounted rate. If the clinic can bundle, it often saves you money in the long run. Ask, “Can you give me a package deal for my treatment plan?” and note the difference from a single‑visit price.
Schedule around your calendar
Once you’ve sorted the money side, it’s time to lock in a slot. Most retinal surgeons prefer early mornings for injections, as the eye is less inflamed. Call the clinic a week in advance, say, “I have a morning appointment on the 15th; does that work?” and confirm the time in writing. If you’re traveling for treatment, ask about travel reimbursement or if the clinic partners with local hotels.
Ask for a written timeline
After the appointment, get a written schedule: the date of the first injection, follow‑ups, and any maintenance visits. Write it down or save it in your phone. Having a visual timeline keeps you on track and reduces the chances of missing a critical visit.
Keep a “cost tracker” journal
As you pay, jot down each expense: the fee for the injection, the cost of the clinic visit, any lab tests, and transportation. Over months, you’ll see a pattern and can discuss budget tweaks with your insurer or the clinic. “I’m tracking my costs to see if I can reduce them” shows you’re proactive, and some clinics offer a payment plan if you’re on a tight budget.
Insurance “red flags” to watch
Some insurers will require a prior approval before they pay for an injection. That’s a sign the treatment isn’t routine or the insurer thinks it might be too expensive. If you hit a roadblock, ask for a written justification or a direct line to a case manager.
Be prepared to negotiate
It’s fine to ask for a discount, especially if you’re paying out‑of‑pocket. Clinics often have a sliding scale or a “no‑gap” program for patients who can’t afford the full fee. Let the billing team know your financial situation upfront; they may offer a payment plan that spreads costs over 12 months.
Double‑check Medicare eligibility
Before you sign anything, confirm the procedure is covered under Medicare. Ask, “Is this procedure on the Medicare list for private patients?” If yes, you’ll know exactly what part Medicare will pay and how much you’ll owe. The Medical Costs Finder is a reliable source for this verification.
Wrap‑up checklist before booking
Confirm insurance coverage and out‑of‑pocket amount.
Ask for a written estimate and bundle options.
Schedule the appointment and get it in writing.
Keep a cost tracker journal.
Verify Medicare eligibility.
By tackling these steps, you’ll avoid surprise bills and have a clear appointment schedule. The result? A smoother eye‑care journey where you’re in control, not just another number on a chart.
FAQ
Got questions? Here are the ones people keep asking when they’re looking for aretina specialist in Sydneyand the answers we’ve gathered from real‑world experience.
What’s the difference between a retina specialist and a general ophthalmologist?
A retina specialist has completed a dedicated fellowship after residency, giving them deep expertise in retinal diseases and surgeries like vitrectomy or anti‑VEGF injections. A general ophthalmologist provides eye care across the board but may refer complex retinal cases. If you’re dealing with AMD, diabetic retinopathy, or retinal detachment, a specialist is the best choice.
How can I be sure a clinic offers a “no‑gap” program for my treatments?
Ask directly about a “no‑gap” or sliding‑scale plan before booking. Clinics that run these programs usually share a written breakdown of out‑of‑pocket costs and a payment schedule. Checking the Medicare Benefits Schedule can also confirm which parts of the fee are covered, so you know exactly what you’ll owe.
What are the most common treatments for wet AMD in Sydney?
Anti‑VEGF injections are the frontline treatment, stopping abnormal blood vessel growth. Some clinics also offer drug‑eluting implants that release medication over months, reducing visit frequency. Surgery is rare and reserved for advanced cases. Discuss the pros and cons of each approach with your specialist; the choice depends on your vision goals and budget.
How often will I need follow‑up appointments after an injection?
Most doctors schedule an initial follow‑up 4–6 weeks after the first injection, then space out subsequent visits as the disease stabilises. A typical plan might be 3–4 injections over six months, followed by maintenance every 6–12 months. Your retina surgeon will give a clear timetable and note any changes needed if the response varies.
Can an optomap retinal exam detect issues before I notice symptoms?
Yes. An optomap captures a wide‑field image of the retina in seconds, revealing early changes in diabetic retinopathy or AMD that might not yet affect vision. If you’re at risk, a regular optomap check can catch problems early. For more details, you can read about the exam here: the optomap guide .
What should I do if I suspect a post‑injection infection?
Redness, pain, or sudden vision loss after an injection means you need immediate care. Call your clinic straight away and, if they’re not reachable, head to an emergency department. Prompt treatment can prevent permanent damage. For background on the condition and its treatment, the Sydney Eye Hospital Foundation provides useful information: learn more here .
Do I need a routine eye exam before visiting a retina specialist?
It helps, but it’s not a hard requirement. A standard eye exam lets your optometrist spot early signs of retinal disease and provides baseline measurements. If you already have a retinal imaging or OCT report from a previous visit, bring that file. Otherwise, a quick check‑up at an optometrist will give your specialist useful context for the next steps.
Conclusion
We’ve walked through what a retina specialist in Sydney can do, from spotting early clues to planning the right treatment.
What matters most is that you’re not left guessing. If you notice a wavy line or a dark spot, act fast—early imaging can catch changes before they bother your daily life.
Remember, a good surgeon doesn’t just perform a procedure; they sit with you, explain the steps, and give you a clear follow‑up plan. That clarity means fewer missed appointments and a smoother recovery. And trust that they’ll explain any risks upfront.
When you’re ready to book, bring the log you’ve kept, ask about the number of procedures they handle, and request a written timeline. If costs are a concern, most clinics offer a “no‑gap” approach, so you know exactly what you’ll pay.
In the end, protecting your vision is a partnership. Stay observant, keep a diary, and keep the conversation open with your specialist. That way, any flare‑up is caught early, and you keep enjoying the sharp details that make life vivid. And your eyes will thank you for the foresight.
So, what’s your next step? Gather your notes, schedule that appointment, and take the first move toward clearer sight.






Comments