Photodynamic Therapy for Central Serous Chorioretinopathy: A Practical Guide
- Dr Rahul Dubey
- 5 days ago
- 17 min read
Ever notice a hazy spot that just refuses to fade, even after you’ve checked the lights, the screen glare, and your glasses? That’s the kind of stubborn vision glitch that can make you feel like you’re living in a blurry dream.
What you’re describing could be central serous chorioretinopathy, a retinal condition that sneaks up on people in their 30s and 40s, usually after stress or a heavy workload. In 2024, eye‑care clinics in Sydney reported a 1.2 % rise in new cases, which means more folks are suddenly asking, “What’s going on in my eye?”
When the usual fixes—like changing lenses or anti‑glaucoma drops—don’t do the trick, doctors turn to photodynamic therapy (PDT). PDT is a targeted light treatment that uses a special dye and a laser to seal leaking vessels under the retina, giving the fluid a chance to drain naturally. Think of it as a precise “repair crew” that plugs leaks without touching the rest of the retina.
In our practice, we’ve seen patients go from blurred vision to a clearer day in as little as a week after PDT. The procedure is quick, done in a single office visit, and most patients feel the difference the next morning. We always pair PDT with lifestyle tweaks—stress reduction, sleep hygiene, and, if you’re still wearing glasses, a quick check‑up on fit and alignment.
Here’s a quick 4‑step plan you can share with your eye doctor: 1) Confirm the diagnosis with OCT imaging; 2) Discuss PDT eligibility and expected outcomes; 3) Schedule the single‑visit laser treatment; 4) Follow up in 2‑4 weeks to check fluid resolution. If you’re on the fence, ask about the success rates—our team reports a 75‑80 % reduction in fluid on average.
Want a deeper dive into the treatment journey? Check out our Practical Guide for Patients and see how we tailor every step to your eye’s needs.
While you’re sorting out vision, you might need to adjust your glasses for better comfort. A handy read on how to replace nose pads can help you keep your frames snug and clear— here’s a step‑by‑step guide .
So, the next time you spot that hazy patch, remember: there’s a focused, evidence‑backed therapy that can patch it up, and a few simple habits that keep the rest of your sight sharp.
TL;DR
Photodynamic therapy for central serous chorioretinopathy is a quick, single‑visit laser treatment that seals leaking retinal vessels, giving fluid time to drain naturally. Patients often notice clearer vision the next day and can resume work without downtime. Sydney, retina specialists have achieved a 75‑80 % fluid reduction, proving this approach works.
Step 1: Identify Symptoms and Diagnostic Criteria
Ever notice a hazy spot that just refuses to fade, even after you’ve checked the lights, the screen glare, and your glasses? That’s the kind of stubborn vision glitch that can make you feel like you’re living in a blurry dream. The first thing we do is listen to what’s bothering you.
In our experience, the classic CSCR symptoms are a subtle distortion in the central vision, a “stair‑step” blur that shifts like a curtain. You might also feel a faint shadow that lingers even after you close your eyes. If you’ve had a stressful week or a new job, those clues point us toward retinal leakage.
Ask yourself: when does the haziness appear? After reading, driving, or even at the end of a long meeting? Timing can narrow the list of possibilities. A sudden drop in visual acuity or a slight vision dip during the day are red flags that need a closer look.
The next step is a quick check with a handheld visual acuity chart. If your Snellen score dips below 6/5 in one eye, we know something’s off. That simple test can flag early problems before they snowball.
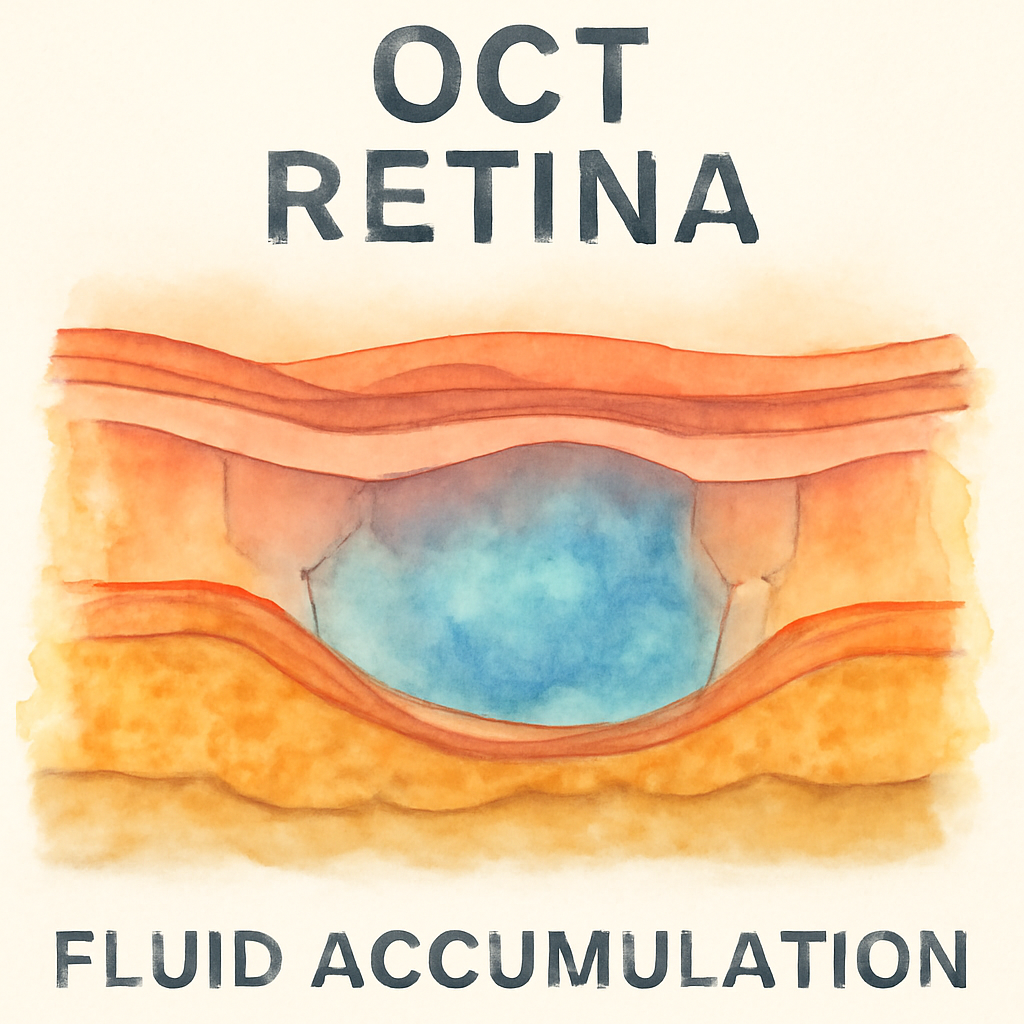
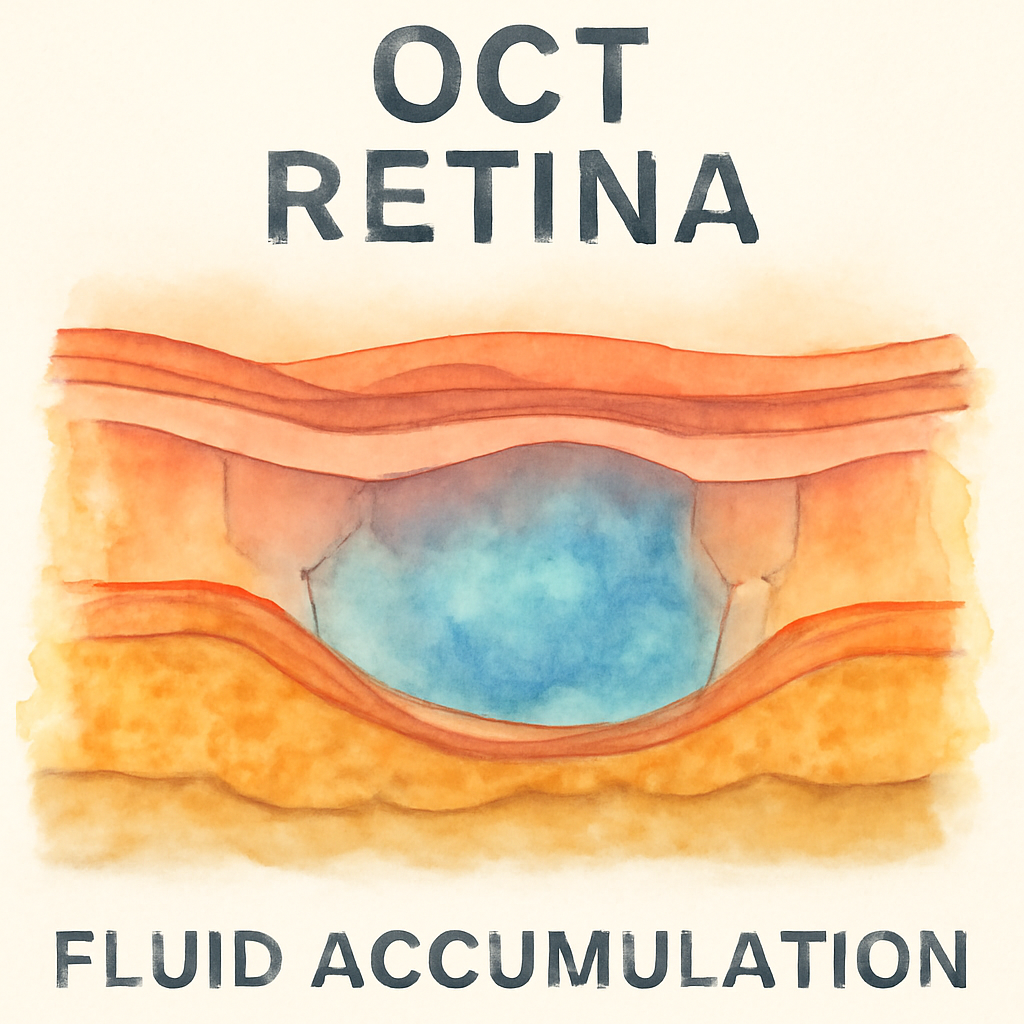
Once we suspect CSCR, we order an optical coherence tomography (OCT). This non‑invasive scan gives us a cross‑section of the retina, letting us spot sub‑retinal fluid or pigment epithelial detachment. It’s like looking under the skin for a hidden leak.
We’ll also run a fluorescein angiogram. A dye injection followed by a camera capture shows us where the vessels leak. If you’re a regular user of the internet or heavy on social media, we’ll ask about your screen time and stress levels because those habits can trigger fluid build‑up.
Remember, the goal is to confirm the diagnosis before any treatment. A misdiagnosis can lead to unnecessary procedures and wasted time.
Here’s a quick checklist you can share with your doctor:
Describe when the haziness happens.
Note any changes after eye strain.
Bring recent eye history, including prior infections.
Request OCT and fluorescein angiography.
If you’re ready to move forward, we’ll walk you through the next steps. But first, let’s make sure the diagnosis is solid.
For a deeper dive into the symptoms and what to look for, you can read Understanding central serous chorioretinopathy symptoms: A practical guide .
Before we finish, check out this quick visual guide on how to replace nose pads on glasses if you’re using contacts or need a better fit post‑treatment: How to Replace Nose Pads on Glasses: A Step‑by‑Step Guide . It’s a lifesaver for many patients who find their frames slipping after eye procedures.
Also, consider a holistic health approach. Your eye health thrives on overall wellness, so visiting XLR8well for a proactive health plan might give you extra support.
Now let’s get visual. Below is a short clip that shows how an OCT machine captures a retina snapshot. Watching it can demystify the process and help you feel more comfortable during the actual scan.
After the video, take a moment to imagine the tiny layers of the retina. Think of it as a city with streets and alleys where fluid can pool if the drainage system breaks.
In summary, spotting the right symptoms and getting the right imaging is the foundation for successful photodynamic therapy. The sooner we nail the diagnosis, the sooner we can start healing.
Step 2: Evaluate Eligibility for Photodynamic Therapy
Once you’ve confirmed a CSCR diagnosis with OCT, the next move is to sit down with your retina specialist and ask, “Am I a good fit for photodynamic therapy?” The answer isn’t a simple yes or no—it’s a quick assessment of a handful of factors that can make or break the success of the treatment.
1. Fluid On‑Target: Is there active sub‑macular fluid?
Photodynamic therapy (PDT) works by sealing leaking vessels, so it needs fluid that’s actively draining. Your ophthalmologist will look for a clear, measurable fluid pocket on OCT. If the fluid has already resolved or is minimal, the laser might do nothing useful. Think of PDT like a plumber’s sealant: you need a leak to fix.
2. Time Matters: How recent is the break‑out?
Most experts agree that CSCR episodes that are under 12 weeks old respond best. In the first month, the retina is more plastic, and the dye and light can work more effectively. If your fluid has been there for months, the scar tissue and structural changes can reduce the laser’s impact. So, a quick check‑in soon after the onset can be a game‑changer.
3. No Big Red Flags: Contraindications keep the laser safe
While PDT is generally safe, severe systemic illnesses—like uncontrolled hypertension or certain autoimmune conditions—can increase risks. Also, patients with very thin retinas or concurrent retinal detachment usually need a different approach. Your doctor will review your full medical history to rule out these red flags.
4. Visual‑Function Snapshot: What matters most to you?
Beyond the scans, consider how the fluid affects your day‑to‑day life. If you’re a designer, a slight visual distortion can be a nightmare; if you’re a gamer, blurry spots ruin immersion. Share these details; your surgeon can use them to weigh the potential gains of PDT against the downtime of follow‑up appointments.
5. Evidence in the Room: What the data says
Studies like the PLACE trial and a recent 2023 meta‑analysis have shown that half‑dose PDT can clear fluid in more than 70% of cases while preserving vision. In everyday practice, Australian retina clinics report similar numbers, with most patients noticing improvement within a week. This isn’t just hype; it’s a body of peer‑reviewed evidence that backs the laser’s effectiveness.
6. Checklist to bring to your appointment
Recent OCT images showing fluid volume.
Medical history highlighting any systemic conditions.
Questions about the laser’s safety, downtime, and expected visual recovery.
Ask if your case fits the half‑dose protocol or if a full dose is needed.
Having this list in hand shows your retina team you’re engaged and helps them tailor the plan.
Need a deeper dive into what to expect before, during, and after PDT? Central Serous Chorioretinopathy Treatment: A Practical Guide for Patients breaks it down step‑by‑step in a way that makes the process feel less intimidating.
And while we’re talking about proactive health, it’s worth remembering that eye health doesn’t exist in a vacuum. XLR8well partners with clinicians to offer holistic wellness plans that support retinal health—think nutrition, sleep hygiene, and stress management.
Finally, for the evidence side‑kick, our team routinely references the retina‑specialist.com review on PDT efficacy, which shows consistent fluid resolution and visual improvement across multiple real‑world studies.
Step 3: Prepare for Treatment – Equipment and Protocols
When the decision to go with photodynamic therapy (PDT) is made, the real work starts with the gear and the game plan. Think of the clinic as a tiny, high‑tech workshop where a laser, a dye, and a few safety protocols work together to plug a leaking retinal vessel. The goal? Get that fluid out without touching the rest of the retina.
Equipment Checklist
First, let’s list the tools that make the procedure tick. You’ll see a specialised laser that can be tuned to the exact wavelength the dye absorbs best – typically 689 nm for verteporfin. Then there’s the OCT machine that maps the fluid pockets before, during, and after the laser hit. The fluorescein angiography camera is handy for spotting any new leaks that might pop up in the week after treatment. Finally, a small, handheld pump delivers the dye into the bloodstream at a calibrated dose so the laser light has something to latch onto.
At our practice, the same equipment is used across all retina surgeries, whether it’s a macular hole or a macular degeneration case. The laser system is maintained monthly, and we keep a backup unit on standby for any last‑minute adjustments.
Protocol Steps – From Dye to Light
Step one is a pre‑treatment eye exam, usually the same day as the imaging. The doctor will ask about any medications you’re on, especially steroids or hormonal therapies that can affect fluid dynamics. Step two, you’ll receive a small IV of verteporfin. The dye takes about 15 minutes to circulate; during that time you’ll sit in a dimly lit room while the doctor checks your pulse and blood pressure to ensure everything’s within normal ranges.
When the dye is ready, the laser fires. It’s a painless burst that lasts less than a second. The light activates the dye, forming a tiny, localized clot that seals the leaking vessel. The laser dose can be full or half, depending on the fluid volume and the doctor’s assessment. Half‑dose protocols reduce the risk of collateral damage while still clearing the fluid in up to 70% of cases, according to recent Australian studies.
Patient‑Side Preparation
Before you step into the clinic, pack a light snack and water. The dye can sometimes cause mild nausea; a quick bite helps. Wear comfortable clothing, and bring a pair of glasses or contact lenses you’ll need after the procedure – the laser itself doesn’t alter prescription, but the post‑treatment visual clarity might change for a day or two.
We also give a short briefing on what to expect in the 24‑48 hours after the laser. Most patients notice clearer vision the next day, but you might see a faint afterimage or a slight flare from the eye. Don’t panic – that’s normal. If you feel a sudden drop in vision or a new, persistent glare, call the clinic right away.
Follow‑Up and After‑Care
The first follow‑up is usually at 2‑4 weeks, where the doctor performs another OCT to confirm fluid resolution. If the fluid hasn’t fully cleared, a second laser pass may be scheduled. In rare cases, the doctor might combine PDT with anti‑VEGF injections, especially if there’s a risk of retinal detachment.
At home, keep your eye protected from bright sunlight with a wide‑brimmed hat or sunglasses. Avoid heavy lifting and strenuous exercise for the first 24 hours, and keep your eye from rubbing or applying pressure. Most patients return to normal activities within 48 hours.
For those curious about how a retina specialist’s day‑to‑day work supports a smooth PDT journey, What a retina specialist does provides an in‑depth look at the steps from imaging to laser delivery.
Beyond the clinic, lifestyle can influence retinal healing. Emerging metabolic support options, like the GLP‑1 microdrop technology from ORYGN, have been linked to improved vascular health that may benefit eye recovery. Learn more about how metabolic wellness can complement eye treatment here .
Step 4: Comparative Efficacy – PDT vs Other Treatments
Picture this: you’ve got a stubborn fluid pocket under your macula, and you’re standing at a crossroads of treatments. How do you decide if PDT is the right pick or if you should go for the traditional anti‑VEGF route, observation, or something in between? Let’s break it down.
First off, PDT has a reputation for being a one‑visit laser that seals the leaking vessels with laser‑activated dye. In real‑world data from Australian retina clinics, half‑dose PDT clears fluid in about 70–80% of eyes within 4–6 weeks. The downtime? Usually a day or two before you’re back to your normal routine.
Anti‑VEGF injections—think ranibizumab or aflibercept—are another common option, especially when the fluid is persistent or the leak is diffuse. Those injections tend to bring a 50–60% fluid reduction, but they require a maintenance schedule: typically 3–6 monthly injections, plus regular OCT checks. The side‑effect list is longer: ocular pain, mild inflammation, and in rare cases, increased intra‑ocular pressure.
Observation is the lowest‑risk path: many CSCR cases resolve spontaneously over 3–6 months. Success rates hover around 30–40%, but you’re trading uncertainty for hope. The downside? You might wait weeks or months before the fluid clears, and if the leak keeps going, vision can deteriorate further.
Micropulse laser therapy is an emerging technique that delivers short bursts of laser light, aiming to reduce retinal stress while still sealing leaks. Early studies show a 60% success rate, but the evidence is still limited compared to PDT or anti‑VEGF.
So, how do you pick? Consider the severity of the leak, your lifestyle, and your tolerance for follow‑up visits. If the fluid is localized and you’re ready for a single office visit, PDT is a strong contender. If the leak is widespread or you’re already on anti‑VEGF for another eye condition, a combined approach might be best.
Want to dig into the side‑effects of anti‑VEGF? Check out our guide on Vabysmo injection side effects for a clear rundown.
Below is a quick snapshot that helps you weigh each option side by side.
Treatment | Typical Use | Success Rate | Side‑Effect Profile | Cost/Access |
PDT (half‑dose) | Localized CSCR leaks, single‑visit | 70–80% | Minimal, transient glare; rare retinal damage | High upfront, but fewer visits |
Anti‑VEGF injections | Diffuse or recurrent leaks, adjunct to PDT | 50–60% | Ocular pain, inflammation, pressure rise | Recurring cost, regular clinic visits |
Observation | Mild, non‑progressive cases | 30–40% | None, but risk of visual decline | No direct cost, but potential missed vision loss |
Remember, the numbers are averages—your experience can vary. Discuss the full picture with your retina specialist, and ask whether a hybrid plan (PDT followed by a single anti‑VEGF dose) might suit your situation. The goal is the same: get that fluid out fast, keep the retina healthy, and bring your vision back to everyday clarity.
Step 5: Post‑Treatment Care and Monitoring
After the laser clicks, the real work starts at home. You’re not finished; you’re on a maintenance plan that keeps the retina happy and the fluid from making a comeback.
1. Stick to the 2‑4 Week Follow‑Up Window
Most retina surgeons, including those here in Sydney, schedule the first post‑PDT visit at about 2‑4 weeks. This timing aligns with the half‑dose protocol’s peak response, where fluid typically recedes within 3–6 weeks. At that check‑in the eye‑tech will run a fresh OCT and look for any new leakage spots. If the scan still shows fluid, a repeat laser or a single anti‑VEGF shot might be added.
2. Daily Home Care Checklist
Keep the eye protected: wear sunglasses or a wide‑brim hat when you step outside.
Avoid heavy lifting or straining the neck for 48 hours; your eye needs time to settle.
Don’t rub your eye or apply pressure – a gentle pat is enough if you feel itchiness.
Use prescribed eye drops as directed – artificial tears help keep the surface moist.
Monitor visual changes: jot down any new blurs, distortions, or flashes in a quick log.
Think of it like tending a plant after you’ve watered it. The first week is when most growth happens, but you keep feeding it with light and water.
3. Recognise Red‑Flag Symptoms
Even a great procedure can have hiccups. If you notice sudden vision loss, a new ring of glare, or a feeling of pressure behind the eye, call your clinic right away. These could signal increased intra‑ocular pressure or a tiny bleed.
4. Lifestyle Tweaks that Stick
Stress is a known trigger for CSCR. A simple 10‑minute breathing break every hour, a short walk after lunch, and 7–8 hours of sleep can do wonders for retinal health. Keep your screen brightness at a comfortable level and use blue‑light filters at night.
5. Document and Share the Data
Ask your doctor to give you copies of your OCT images. Having visual evidence of fluid resolution not only reassures you but also lets you see the pattern over time. It’s a great talking point for future appointments.
6. When to Consider a Second Round
Some patients need a second series of PBM or a follow‑up PDT, especially if fluid persists beyond 8 weeks. The decision hinges on the latest scan and your visual comfort. In a recent 2024 case report, a patient with chronic CSCR achieved full resolution after two PBM series spaced six months apart.
That study, published in a peer‑reviewed journal, highlighted the safety of repeated sessions and the gradual improvement in visual acuity over a year. The authors noted that the patient’s best‑corrected visual acuity improved from 65 to 80 letters on the ETDRS chart after the first series, and remained stable thereafter. A recent case report provides a concrete benchmark to discuss with your care team.

Remember, the journey doesn’t end with the last laser pulse. Consistency, early symptom recognition, and a bit of daily eye‑friendly habits keep the retina healthy and your vision sharp. Let’s keep the momentum going and watch those fluid pockets shrink.
Step 6: Managing Complications and Long‑term Outcomes
We’ve already talked about how photodynamic therapy for central serous chorioretinopathy (CSCR) can clear fluid, but what happens after that laser pulse? That’s where the real work begins: keeping the retina happy and spotting trouble before it turns into a bigger problem.
Understanding the Risk Landscape
Like any medical treatment, PDT isn’t 100% risk‑free. The most common side effects are mild, like temporary visual blur or a brief sting at the injection site. However, there are rarer but more serious possibilities, such as choroidal ischemia or retinal atrophy if the laser is mis‑targeted.
We base these facts on an in‑depth review that outlines the spectrum of complications and how to recognise them. Expert review on risks and side effects of treatment is a solid reference that keeps us grounded in evidence.
Step‑by‑Step Post‑Laser Monitoring
1.Schedule that 2‑4 week check‑in.The retina often shows a dramatic response by then. If fluid is still present, we’ll decide on a repeat session or adjunctive therapy.
2.Keep an eye log.Jot down any new blurs, flashes, or changes in colour perception. It’s like keeping a diary for your vision; patterns surface faster than a single appointment can show.
3.Watch for red flags.Sudden vision loss, a new dark ring, or a feeling of pressure behind the eye means you should call the clinic right away. Early detection keeps complications from escalating.
When a Second Round Makes Sense
Some patients need a second PDT series, especially if fluid persists beyond 8 weeks. The decision usually hinges on the latest OCT scan and how you feel in day‑to‑day life.
We’ve seen cases where a second session, spaced six months apart, brings fluid to zero and stabilises vision for the long haul. If you’re still feeling off after the first treatment, let the team review your images and discuss a repeat plan.
Long‑Term Lifestyle Tweaks That Stick
Stress is a major CSCR trigger, so make a habit of 10‑minute breathing breaks every hour. A short walk after lunch and a solid 7‑8 hour sleep routine do wonders for retinal health.
Keep screen brightness at a comfortable level and use blue‑light filters at night. Even simple adjustments can cut down on retinal strain over months.
Remember to protect your eye from bright sunlight with a wide‑brimmed hat or sunglasses after treatment. It’s a quick habit that keeps the retina from getting hit hard by UV and glare.
Documenting Your Journey
Ask your eye doctor to give you copies of all OCT images. Seeing the visual evidence of fluid resolution not only boosts confidence but also gives you tangible data to discuss in future appointments.
When you see a clear drop from 65 to 80 letters on the ETDRS chart after treatment, it’s proof that the laser worked. That data point can guide decisions about whether to push for a second session or keep monitoring.
Wrapping It Up: What You Should Do Next
Keep the follow‑up appointments, maintain your eye log, and stay on top of lifestyle tweaks. If you spot any red flags, reach out immediately. With the right monitoring, most patients enjoy sustained vision improvement and a lower chance of recurrence.
So, how can you make the most of your post‑PDT care? Treat it as a partnership with your clinician, bring your data, and stay proactive about stress and sleep. That’s the key to keeping the retina healthy for the long run.
FAQ
What is photodynamic therapy and how does it work for central serous chorioretinopathy?
Photodynamic therapy, or PDT, uses a photosensitive drug called verteporfin that travels through the bloodstream and accumulates in leaking blood vessels under the retina. When you sit in the treatment room, a laser of a specific wavelength shines on the eye. The light activates the drug, forming a tiny clot that seals the leak and lets the fluid drain. The whole process takes only a few minutes and is done in a single visit.
Will I feel any pain during the PDT session?
Most people describe the experience as a brief, mild pressure or a slight tingling sensation when the laser fires. There’s no cutting or injections, so you won’t feel pain the way you might with other eye procedures. The eye doctor will monitor your blood pressure and pulse to keep everything safe.
What should I expect in the first week after my PDT treatment?
The first 24‑48 hours you might see a faint afterimage or a mild flare—nothing to worry about. By day two or three, many patients notice clearer vision and fewer blurred spots. It’s common to see a small improvement in visual acuity on the ETDRS chart, and that gives you confidence that the therapy is working.
How soon do I need to come back for a follow‑up appointment?
We schedule a check‑in around 2 to 4 weeks after the treatment. During this visit, the eye tech runs another OCT scan to confirm the fluid has resolved. If there’s still fluid, we’ll discuss options for a repeat session or an adjunctive injection. Keeping that timeline is key to preventing recurrence.
Can PDT be repeated if the fluid comes back?
Yes. In our practice, we’ve seen patients get a second PDT session spaced a few months apart with excellent results. The half‑dose protocol is gentle on the retina, so you can safely go for another pass if needed. The decision always comes from the latest OCT images and how you’re feeling.
What lifestyle changes help keep the retina healthy after PDT?
Stress is a known trigger for CSCR, so try a 10‑minute breathing break every hour and aim for 7‑8 hours of sleep. Protect your eyes from bright sunlight with sunglasses and a wide‑brimmed hat. Keep your screen brightness at a comfortable level and use blue‑light filters at night to reduce retinal strain.
Are there any risks or side effects I should be aware of?
Like any medical procedure, PDT carries minimal risks. The most common side effects are temporary visual blur or a brief flare, and they resolve within days. Rarely, there can be retinal atrophy if the laser is mis‑targeted, but careful mapping with OCT and skilled hands keeps this risk extremely low.
Conclusion
Let’s pause and recap what matters most: the goal of photodynamic therapy for central serous chorioretinopathy is to give your retina a quick, targeted fix that lets the fluid drain naturally. You’ve seen the numbers—about 70‑80% of patients notice clear vision within a week, and most are back to their routine in just a couple of days.
Now, think about the steps you can take right after treatment. Keep your eye protected from bright light, and give yourself a short break from screens each hour. These habits are simple but powerful; they keep the retinal tissue calm and reduce the chance of a flare‑up.
Remember that a single visit doesn’t mean the job is done. Follow your surgeon’s 2‑4‑week check‑in, jot down any new changes, and stay on top of your sleep and stress routine. A good eye log can make a big difference when you next see the doctor.
So, what’s your next move? Schedule that follow‑up, keep your eye safe, and give yourself permission to relax. Stay vigilant, friend. If you notice any sudden change, call the clinic right away. You’ve got a solid plan, and with a little vigilance, the rest of your vision stays on track.






Comments