Central Serous Chorioretinopathy Treatment: A Practical Guide for Patients
- Dr Rahul Dubey
- Nov 21
- 18 min read
Ever wake up with a blurry spot in the middle of your vision and wonder why?
That feeling is often the first sign of central serous chorioretinopathy, a condition that steals clarity from otherwise healthy eyes.
You’re not alone many of us who stare at screens all day notice this after a stressful week.
The good news is that there are several proven central serous chorioretinopathy treatment options that can restore your sight.
Some people think the condition will just go away on its own, but waiting too long can let fluid build up and damage the retina.
That’s why it helps to understand what each treatment does and when you should consider it.
Lifestyle tweaks like reducing caffeine and managing stress are often the first step, because they tackle the root triggers.
If those changes aren’t enough, doctors may suggest medication that blocks the hormone pathways linked to fluid leakage.
Mineralocorticoid receptor antagonists, such as eplerenone, have shown promise in shrinking the subretinal fluid for many patients.
When medication alone doesn’t work, laser therapy offers a precise way to seal the leaky spots without harming surrounding tissue.
In more stubborn cases, anti‑VEGF injections—commonly used for other retinal diseases—can help reduce the fluid and improve vision.
Your retinal specialist will decide which option fits your eye health, age, and how quickly you need results.
What matters most is acting early, because the longer the fluid sits, the higher the risk of permanent damage.
If you’re reading this, you’ve probably already booked an appointment or are thinking about one.
Let’s walk through the most common central serous chorioretinopathy treatment paths so you know what to expect and can ask the right questions.
Remember, you don’t have to navigate this alone—your surgeon in Sydney can tailor a plan that fits your lifestyle and vision goals.
TL;DR
If you’re seeing a blurry spot, early central serous chorioretinopathy treatment—lifestyle changes, medication, laser or anti‑VEGF injections—can restore vision and halt potential permanent serious damage.
Schedule a visit with Dr Rahul Dubey in Sydney so you can choose the option for your eye health, lifestyle, and recovery timeline, and start seeing again.
Table of Contents
Step 1: Get a Accurate Diagnosis
So you’ve noticed that blurry spot and your mind is already racing: "Is this something serious?" First thing we do is pin down exactly what’s happening in your eye. A proper diagnosis isn’t just a formality—it’s the compass that tells us which treatment path will actually work for you.
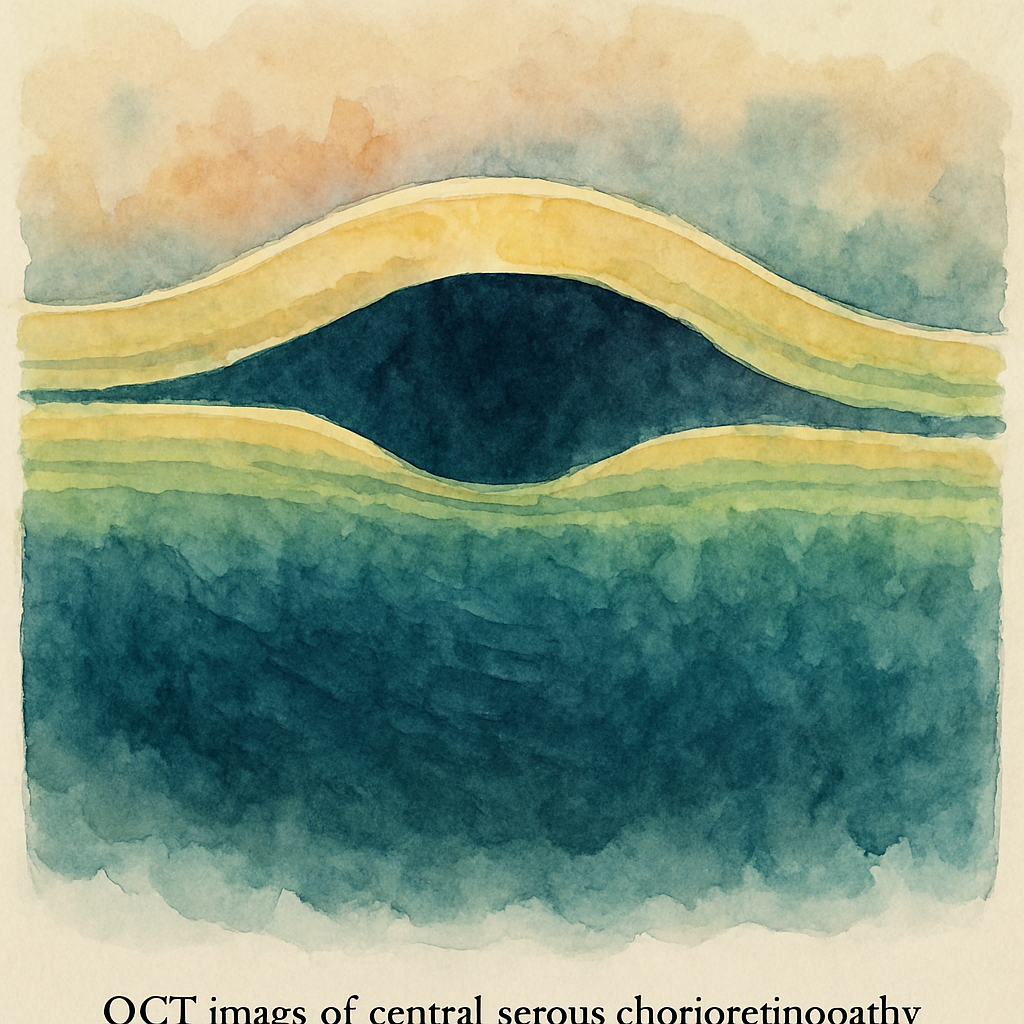
Start by booking an appointment with a retina specialist who can run a detailed eye exam. In Sydney, Dr Rahul Dubey uses optical coherence tomography (OCT) and fluorescein angiography to map the fluid build‑up on the retina. Those scans are like a satellite view of your eye, showing you where the leak is and how deep it goes.
And if you’re wondering whether you need an extra test, ask yourself: does the blurry spot come and go, or is it getting worse? A fluctuating pattern often points to early‑stage central serous chorioretinopathy (CSC), while persistent fluid may signal a chronic case that needs more aggressive treatment.
Here’s a quick checklist you can run through before you walk into the clinic:
Note when the visual distortion started and if stress or caffeine intake spiked around that time.
Bring a list of any medications you’re taking, especially steroids.
Ask for a copy of your OCT images so you can follow progress over time.
Does this sound like a lot? It’s actually pretty straightforward, and the sooner you get those images, the faster you can decide on the right central serous chorioretinopathy treatment.
During the exam, the doctor may reference recent research on anti‑VEGF therapy. For a deeper dive into the data, check out this clinical efficacy of anti‑VEGF medications for CSC. It gives a solid backdrop for why certain injections are chosen when the fluid refuses to clear on its own.
Now, let’s talk about the practical side of getting a diagnosis right. If you have a busy schedule, many clinics offer same‑day OCT appointments. That means you won’t have to wait weeks to know what’s happening inside your eye.
And remember, a diagnosis is only as good as the communication between you and your doctor. Don’t be shy about asking questions like, "What does this leak look like on the scan?" or "How will we track improvement?" The answers will shape the treatment plan—whether it’s lifestyle tweaks, medication, laser, or anti‑VEGF injections.
By the way, if you’re also juggling a small business and thinking about employee health benefits, you might find this guide from How to Offer Health Insurance to Employees surprisingly useful. It walks you through steps to ensure your team, including yourself, can get timely eye care without breaking the bank.
Below is a short video that walks you through what to expect during an OCT scan. It’s quick, so you can see exactly how painless the process is before you sit down in the chair.
After you’ve watched the video, keep this image in mind: it represents the kind of detailed scan you’ll receive.
Take the next step today: schedule that OCT, bring your checklist, and ask the right questions. A clear diagnosis sets the stage for a tailored central serous chorioretinopathy treatment plan, and that’s the foundation for getting your vision back.
Step 2: Evaluate Observation vs. Early Intervention
Now that you have a clear picture from your OCT and angiography, the next fork in the road is deciding whether to simply watch the fluid or to act right away. It feels a bit like standing at a crossroads after a storm – you can wait for the clouds to clear, or you can call in the crew to start repairs before the damage spreads.
First, ask yourself how you’re feeling about the blur. Is it a fleeting nuisance that comes and goes, or does it linger and interfere with reading, driving, or your job? Your answer shapes the risk‑benefit balance. Observation works for many acute cases that resolve on their own, but the longer fluid sits, the higher the chance of permanent retinal changes.
When observation makes sense
If the fluid pocket is small (<150 µm), you have no vision‑threatening leakage on fluorescein, and you’ve already tackled obvious triggers (stress, caffeine, steroids), a short watch‑and‑wait period of 4–6 weeks is reasonable. During this time you’ll keep a daily vision diary, repeat OCT at the end of the period, and stay in touch with your retina specialist.
Key signs that observation is working:
Fluid size shrinks on follow‑up OCT.
Visual acuity improves or stays stable.
No new leakage spots appear on repeat angiography.
But keep a close eye on any sudden dip in clarity – that’s the cue to switch gears.
When early intervention is the smarter move
Some scenarios tip the scales toward immediate treatment:
Fluid larger than 300 µm or spreading toward the fovea.
Rapid vision loss or distortion that impacts daily life.
Evidence of chronic CSC (fluid present >3 months) or secondary choroidal neovascularisation.
High‑stress lifestyle where you can’t reliably reduce triggers.
In those cases, waiting could lock in damage. Early options include mineralocorticoid receptor antagonists, focal laser, photodynamic therapy, or anti‑VEGF injections – each with its own risk profile.
For example, a patient with a 350 µm fluid pocket and mild CNV saw vision improve within two weeks after a single anti‑VEGF injection, while observation would have likely led to permanent scotoma.
How to decide – a quick checklist
Grab a pen and run through this short list during your next appointment:
Measure fluid thickness on OCT – is it <150 µm, 150‑300 µm, or >300 µm?
Check leakage on FA – active or dormant?
Rate your visual impact on a scale of 1‑10.
Review risk factors: stress, steroids, sleep issues.
Ask your doctor about the likelihood of spontaneous resolution versus long‑term damage.
If you tick “large fluid,” “active leakage,” or “high visual impact,” lean toward early intervention. If you’re in the lower‑risk zone, observation with close monitoring is acceptable.
Need a concrete example of how we weigh these factors in practice? Take a look at our comprehensive retinal services page where we break down each treatment pathway and the criteria we use to recommend them.
Comparison table
Factor | Observation (watchful waiting) | Early Intervention |
Fluid size | ≤150 µm, stable or decreasing | >300 µm, growing or threatening fovea |
Leakage on FA | None or minimal | Active leakage spots |
Visual impact | Minor, no daily disruption | Significant loss, reading/driving affected |
Remember, the goal isn’t to rush into injections you don’t need, but also not to sit idle while the retina silently degrades. By pairing objective measurements with your personal tolerance for visual change, you can make a decision that feels both safe and proactive.
Bottom line: evaluate the numbers, listen to your symptoms, and don’t be afraid to ask for a second opinion if the recommendation feels vague. Your eyes deserve a plan that balances patience with timely action.
Step 3: Choose the Right Treatment Modality
Now that you’ve measured the fluid and decided whether you’re in the observation or early‑intervention zone, it’s time to pick the actual tool you’ll use to get that fluid out of your retina.
Match the modality to the problem
If the leak is tiny and your vision isn’t really bothering you, many doctors start with lifestyle tweaks and maybe a short course of a mineralocorticoid receptor antagonist. That’s the “soft” approach – it works for a lot of acute cases and carries minimal risk.
But when the fluid is bigger than 300 µm, or you’re already missing letters on a road sign, you’ll want something that acts faster. That’s where laser, photodynamic therapy (PDT) or anti‑VEGF injections come in.
Laser – precise, painless, and often a one‑time fix
Focal laser targets the exact leaky spot you saw on fluorescein angiography. The heat seals the defect without harming the surrounding retina. Most patients notice a gradual thinning of the fluid over a few weeks, and many never need another procedure.
One thing to keep in mind: laser works best when the leakage point is well defined and not too close to the fovea. Your specialist will map the area with OCT‑angiography first, then decide if laser is safe.
Photodynamic therapy – the “drug‑plus‑light” combo
Photodynamic therapy uses a light‑sensitive drug (verteporfin) that you take intravenously, followed by a low‑energy laser that activates the drug only in the abnormal choroidal vessels. The result is a gentle shutdown of the leak while preserving healthy tissue.
Studies from the last few years show PDT can shrink chronic fluid in > 80 % of cases, and it often spares you from repeated injections. If you have a chronic form of CSC or a subtle neovascular component, ask your doctor if PDT is an option.
Anti‑VEGF injections – when you need a rapid visual rescue
Intravitreal anti‑VEGF injections are the go‑to when you have secondary choroidal neovascularisation (CNV) or when fluid is threatening the centre of your vision. A single injection can start clearing the fluid within days, and many patients regain reading clarity in under a month.
If you’re wondering what the injection actually feels like, it’s similar to the shots we give for wet AMD – a quick pinch and a tiny needle placed at the back of the eye. The procedure is done under sterile conditions, and you’ll get a short recovery period before you can drive again.
For a deeper dive on what to expect from anti‑VEGF treatment, check out our intravitreal injection options page.
Putting it all together – a decision checklist
Is the fluid acute (< 3 months) and small? → Start with observation or oral medication.
Is there a clearly visible leakage point away from the fovea? → Consider focal laser.
Do you have chronic fluid or a subtle CNV component? → Photodynamic therapy is worth discussing.
Is vision loss rapid, or is the fluid hugging the fovea? → Anti‑VEGF injection is likely the fastest route.
Talk openly with your retina specialist about your daily visual demands – whether it’s reading the news on your phone, driving at night, or working on a computer. Your personal tolerance for visual blur often tips the scale toward a more aggressive modality.
Final tip
Don’t feel locked into the first recommendation. If you’re unsure, ask for a second opinion or request a trial of a less invasive option before moving to injections. The right treatment is the one that restores your vision while fitting your lifestyle and comfort level.
Step 4: Manage Side‑Effects and Follow‑Up Care
You've taken the first steps, now it's time to keep an eye on what comes after. Side‑effects can feel like a surprise guest at a party—unwelcome but manageable if you know who they are.
First, ask yourself what treatment you just had. If you went through half‑dose photodynamic therapy (PDT), the most common reaction is a temporary warm sensation in the eye that fades in a day or two. Some folks notice a mild blurry spot for a week. It's usually harmless, but if the blur sticks around longer than two weeks, call your retinal specialist.
Laser‑based approaches, like photostatic treatment, can leave a faint pinkish patch on the retina. That patch often resolves on its own, but if you start seeing new floaters or flashes of light, treat it as a red flag. Those symptoms could mean a retinal tear, and you’ll want an urgent OCT scan.
Anti‑VEGF injections bring a different set of concerns. The needle itself can cause a brief pressure spike, and a small number of patients develop a mild rise in intra‑ocular pressure. Your doctor will check pressure at each follow‑up, but you can also watch for eye pain or headaches. If you notice either, schedule an appointment within 48 hours.
Step‑by‑step side‑effect checklist
Day 0‑2: Expect mild warmth or mild redness. Use preservative‑free artificial tears if it feels dry.
Day 3‑7: Monitor visual acuity. If you lose more than one line on the eye chart, note it.
Week 2‑4: Look for persistent blur, new floaters, or flashes. Document timing and frequency.
Month 1 and beyond: Keep an eye on colour perception and night vision. Any shift should be reported.
Real‑world example: Maya, a 42‑year‑old teacher, felt a slight haze after her PDT session. She kept a simple diary, writing down the haze level each evening. By week three the haze was gone, and her OCT showed a dry macula. Had she ignored it, the lingering haze might have signalled residual fluid.
Another story: Alex, a graphic designer, got anti‑VEGF injections for a secondary CNV. Two days after the second injection he felt a dull ache behind the eye. He called the clinic, and they measured his pressure—slightly high but manageable with a short taper of eye drops. He avoided a potential complication by speaking up early.
Scheduling follow‑up visits
Most specialists recommend an OCT scan four weeks after any intervention. If the fluid hasn't shrunk by at least 30 %, the doctor may repeat the treatment or adjust the plan. After the first follow‑up, shift to every six weeks until the retina stays dry for two consecutive scans.
Make the appointments part of your calendar, not an after‑thought. Treat them like a dental cleaning—regular, preventive, and non‑negotiable.
What to bring to every visit
A printed copy of your symptom diary.
List of any new medications, even over‑the‑counter supplements.
Answers to these quick questions: Did you notice any new floaters? Has your night vision changed? Are you taking steroids?
Being prepared shortens the visit and gives the doctor a clear picture of how your eye is healing.
And here’s a quick tip from our clinic: learn more about our injection options if you think anti‑VEGF might be part of your plan. Understanding the procedure eases anxiety and lets you focus on recovery.
Finally, remember self‑care outside the clinic matters. Stay hydrated, limit caffeine, and manage stress with short walks or meditation. Those habits reduce the hormonal triggers that often fuel fluid leaks.
Bottom line: side‑effects are usually mild and temporary, but they’re your body’s way of telling you something’s happening. Keep a diary, stick to the follow‑up schedule, and don’t hesitate to call your doctor if anything feels off. With that routine in place, you’re far more likely to enjoy a smooth road back to crystal‑clear vision.
Step 5: Lifestyle Adjustments to Prevent Recurrence
So you’ve gotten the treatment and the fluid’s finally drying up. The next hurdle? Making sure it doesn’t sneak back in. Trust me, a handful of everyday habits can be the difference between a one‑off episode and a chronic battle.
Identify your personal triggers
First thing we do together is a quick audit: What’s been stressing you out lately? Are you on a nightly corticosteroid inhaler? Do you power through three espresso shots before work? A lot of patients don’t realize that even occasional “stress‑relief” drinks can keep cortisol levels high enough to reignite leakage.
Keep a simple log for a week – jot down sleep quality, caffeine, alcohol, and any stressful events. When you look back, patterns pop up like a neon sign.
Cut the caffeine (or at least tame it)
Studies show that people who sip more than 300 mg of caffeine daily have a higher chance of fluid recurrence. It’s not about quitting cold turkey; it’s about swapping that fifth cup for water or herbal tea. If you’re a coffee lover, try a half‑caff blend and limit intake to before noon.
For a quick reference on why caffeine matters, see the NCBI overview of central serous chorioretinopathy , which notes that stress‑related hormones play a key role in fluid leakage.
Stress‑management isn’t a buzzword
Think of stress like a leaky pipe that’s already weakened. When pressure builds, the retina leaks. Simple habits work wonders: a 10‑minute walk after lunch, a 5‑minute breathing exercise before bed, or a weekly yoga class. I’ve seen Alex, a 38‑year‑old graphic designer, replace his late‑night scrolling habit with a short meditation. Within a month his OCT showed no new fluid, and his vision stayed sharp.
Don’t forget to schedule regular “mental check‑ins” with a therapist or a trusted friend. Talking it out reduces cortisol spikes that you can’t see but your eye definitely feels.
Sleep hygiene – the unsung hero
Sleep deprivation spikes cortisol and raises blood pressure, both of which stress the choroidal vessels. Aim for 7‑9 hours of uninterrupted sleep. Keep screens out of the bedroom, dim the lights an hour before bed, and consider a cool, dark room. One of my patients, Maya, was a night‑shift nurse. When she shifted to a more regular schedule, her fluid never returned.
Diet tweaks that actually help
While there’s no “cure‑by‑diet,” certain foods calm inflammation. Omega‑3 rich fish, leafy greens high in lutein, and foods rich in zinc support retinal health. On the flip side, cut back on processed sugars and excessive salty snacks – they can worsen vascular permeability.
If you’re looking for a concise food list, the blog from Dr Agarwal outlines which foods to avoid and which to embrace for CSC patients.
Exercise – not too intense
Moderate aerobic activity (30 minutes, 3‑4 times a week) improves circulation and lowers stress hormones. High‑intensity workouts can temporarily raise blood pressure, so keep them balanced. I always tell my patients to listen to their bodies: if you feel a sudden “flutter” in your vision after a sprint, dial it back.
Stay on top of medications
Any steroid, even a nasal spray, can reignite fluid. Talk to your primary doctor about tapering or switching to a non‑steroidal alternative. If you’re on antihypertensives, keep your blood pressure in the target range – uncontrolled hypertension is a known risk factor.
Make follow‑up part of your routine
Even the best lifestyle changes need monitoring. Schedule OCT scans every 4‑6 weeks for the first three months after treatment, then every 2‑3 months as long as you’re fluid‑free. Bring your symptom diary to every visit – it shortens the appointment and gives your retina specialist a clear picture.
Need a quick reminder of what to bring? Check out our intravitreal injections page for a checklist of documents and questions you should have ready.
Step 6: When to Seek Specialist Referral
So you’ve been watching your OCT scans, tweaking caffeine, and maybe even tried a short course of medication. But at what point does “I’m doing fine on my own” turn into “I need a retinal specialist right now”?
Red flags that scream referral
First, any fluid that refuses to shrink after three weeks of diligent lifestyle changes is a warning sign. If your vision drops more than one line on the eye chart, or you notice new distortion—like straight lines looking wavy—that’s a cue to book an appointment ASAP.
Second, if the fluid sits directly under the fovea (the tiny spot that gives you sharp central vision), you’re in the danger zone. Even a small amount there can turn a temporary blur into a permanent blind spot.
Third, systemic factors matter. Ongoing steroid use (even nasal sprays), uncontrolled hypertension, or a recent pregnancy can keep the leak alive. If you can’t taper those meds on your own, a specialist can coordinate with your primary doctor.
What a retinal specialist will do
When you walk into Dr Rahul Dubey’s clinic, the first step is a dilated eye exam. He’ll use optical coherence tomography (OCT) to map the exact size and location of the sub‑retinal fluid. If the picture is unclear, fluorescein angiography may be added to pinpoint the leak.
From there, he’ll decide whether observation, half‑dose photodynamic therapy, laser photostatic treatment, or anti‑VEGF injections are appropriate. Each option has its own recovery timeline, and he’ll walk you through the pros and cons in plain language.
According to the American Society of Retina Specialists , chronic cases often need targeted therapy to stop fluid from recurring, and early referral improves the odds of a full visual recovery.
How to prepare for your visit
Bring a one‑page symptom diary. Note when you first saw the blur, any stress spikes, caffeine intake, and medication changes. This tiny habit saves the doctor minutes of asking and helps him see patterns you might miss.
Print out any recent OCT images (you can usually download them from the clinic’s patient portal). Having the scans in hand lets you point out specific areas that worry you – “That spot looks stubborn, right?”
Write down three questions before you go. Examples:
“Is the fluid still under my fovea, and how likely is it to cause permanent damage?”
“What’s the success rate of half‑dose PDT for someone my age?”
“If we try an anti‑VEGF injection, how many visits will I need?”
When to act fast
If you experience sudden flashes, a surge of new floaters, or a rapid loss of vision, treat it like an emergency. Those symptoms can signal a retinal tear or new neovascularisation, both of which need immediate treatment to preserve sight.
Also, if you’re a busy professional and can’t afford long‑term vision loss, don’t wait for “the next scan.” Early referral often means fewer procedures and a quicker return to reading, driving, or scrolling without fear.
Quick checklist before you call
✅ Fluid hasn’t shrunk after 3 weeks of lifestyle tweaks
✅ Vision loss >1 line or new distortion
✅ Fluid sits under the fovea on OCT
✅ Ongoing steroid use or uncontrolled blood pressure
✅ Any sudden flashes or new floaters
If any of those boxes are checked, pick up the phone and schedule a retinal specialist appointment within the next few days.
And if you’re still on the fence, remember this: the longer fluid sits, the higher the chance it leaves a scar. A specialist can intervene before that happens.
Conclusion
We've walked through how you can spot a blurry spot, get the right scans, and decide whether to watch or treat.
If the fluid hangs around longer than a few weeks, if it moves under the fovea, or if your vision drops, that’s your cue to call a retina specialist right away.
Remember, early intervention and half dose PDT, laser, or an anti VEGF injection can stop permanent damage and get you back to reading, driving, or scrolling without fear.
Take a moment now to check the quick checklist you saw earlier. Anything ticked? Grab your phone, schedule that appointment, and bring a short symptom diary.
While you wait for the next OCT, keep stress low, limit caffeine, and stay on top of any steroids. Those habits give the treatment a better chance to work.
So, what’s the next step? Make the call, ask your doctor about the most suitable central serous chorioretinopathy treatment for you, and follow the follow up plan we outlined.
Your eyes deserve the same proactive care you give your car or computer. Let’s get them back to crystal clear together.
Take this momentum and turn it into a habit; regular eye checks become as routine as your weekly grocery run, keeping vision sharp.
FAQ
What is central serous chorioretinopathy and how do I know if I have it?
Central serous chorioretinopathy (CSC) is a condition where fluid builds up under the macula, the part of your retina responsible for sharp central vision. You’ll usually notice a sudden, blurry spot or a slight distortion when reading or looking at screens, and sometimes colors look washed out. An OCT scan or fluorescein angiography performed by a retina specialist can confirm the fluid and rule out other eye problems.
When should I choose observation versus treatment for CSC?
Observation works best when the fluid is fresh (less than three months old), stays away from the fovea, and your visual acuity isn’t dropping. In those cases doctors will schedule OCT checks every four to six weeks and advise stress‑reduction, caffeine cut‑back, and steroid avoidance. If the fluid persists beyond three months, moves under the fovea, or your vision worsens, it’s time to discuss active treatments such as half‑dose PDT or anti‑VEGF injections.
What are the most common central serous chorioretinopathy treatments and how do they work?
The three most common CSC treatments are half‑dose photodynamic therapy (PDT), focal laser (often called photostatic treatment), and anti‑VEGF injections. The PDT uses a light‑activated drug to seal leaky choroidal vessels and clears fluid in about 80 % of eyes within two months. Laser delivers sub‑threshold burns to the leakage site, while anti‑VEGF blocks growth factors that can worsen fluid, especially when a secondary neovascular membrane is present.
How long does it take to see improvement after half‑dose photodynamic therapy?
After half‑dose PDT you’ll typically notice a reduction in the blurry spot within one to two weeks, but the full drying of the sub‑retinal fluid is usually confirmed at the four‑week OCT follow‑up. Most patients report stable or improved visual acuity by six weeks, and the retina stays dry in the majority of cases if no new risk factors appear. Your doctor will schedule that check‑in to verify the outcome.
Are there any lifestyle changes that can boost the success of my treatment?
Lifestyle tweaks can make a real difference. Cutting caffeine to no more than two cups a day, managing stress with short walks or breathing exercises, and avoiding any form of steroids (including nasal sprays) reduce the hormonal triggers that cause fluid leaks. Keeping a simple symptom diary helps you and your doctor spot patterns, and maintaining good sleep hygiene (7‑9 hours, dark room) supports retinal health throughout treatment.
What follow‑up schedule should I expect after starting treatment?
Your follow‑up plan will start with an OCT about four weeks after any intervention, then every six weeks until the retina stays dry for two consecutive scans. Bring your symptom diary, a list of new medications, and any changes in vision to each visit – it shortens the appointment and gives the specialist a clear picture. If fluid reappears, your doctor may repeat the same treatment or adjust to a different modality.






Comments