How Long Does Macular Hole Surgery Take? A Step‑By‑Step Guide
- 13 hours ago
- 20 min read
Ever walked into the clinic, heard the term "macular hole surgery" and wondered how long you'll be in the recovery chair before life feels normal again? You're not alone – that moment of uncertainty is exactly what most patients feel the day they get the call for surgery.
In a typical macular hole procedure, we make a tiny incision in the eye, insert a tiny gas bubble, and use a delicate laser to flatten the hole. The whole operation itself usually takes about 45 to 60 minutes – just enough time to get you settled, prepped, and back in the recovery lounge.
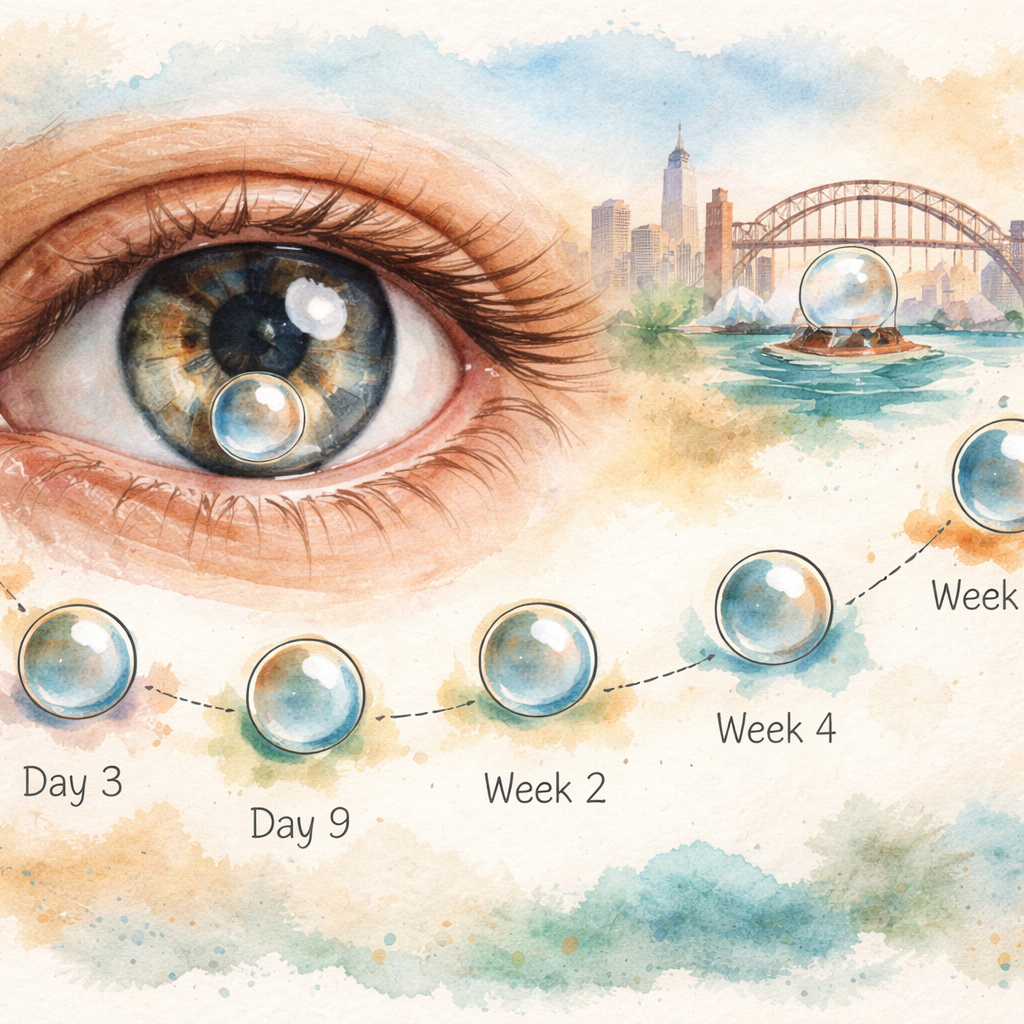
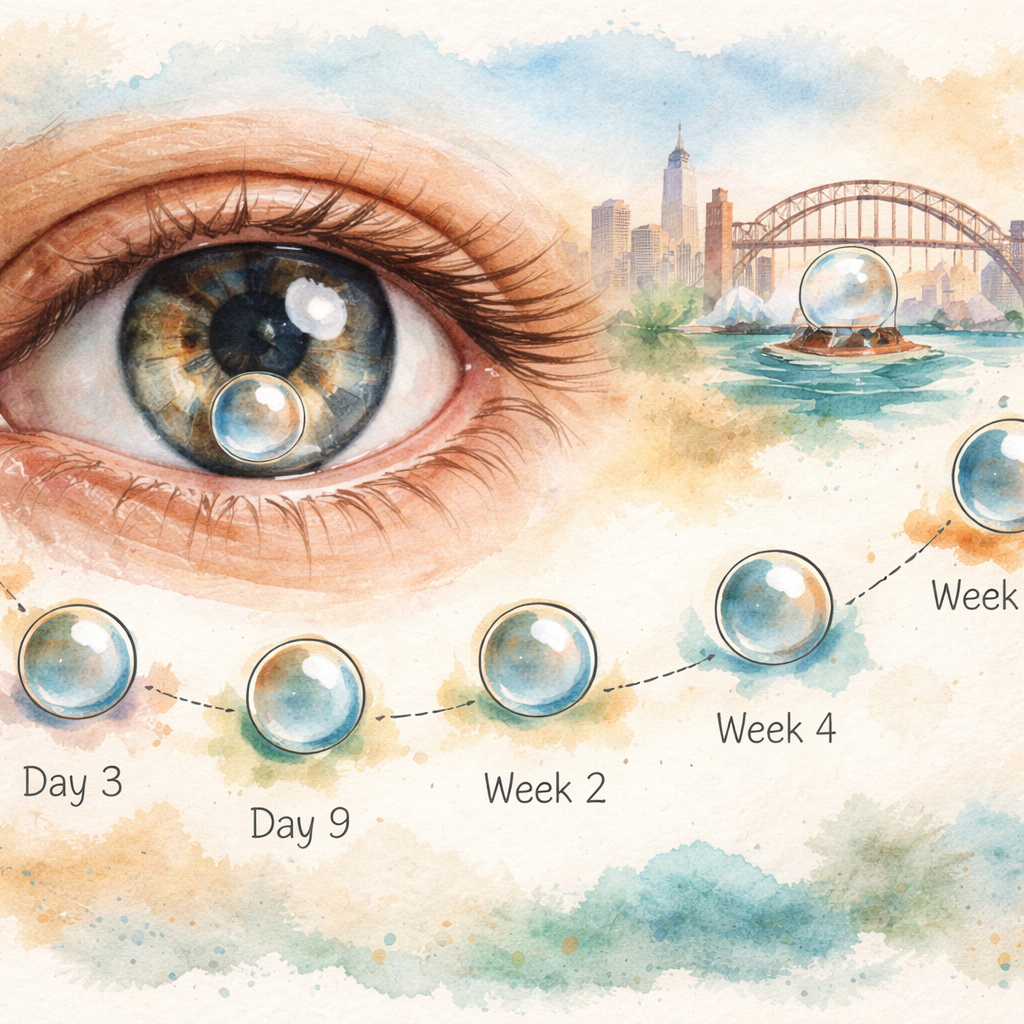
But the real question is the timeline after you leave the theatre. Most of our Sydney patients notice a marked improvement in vision within the first week. By day three, the gas bubble is already doing its job, pushing the retinal edges together. Around day seven, a follow‑up OCT scan often shows the hole closed and the retina re‑attached.
From there, things get a little variable. Younger patients (under 60) typically see their visual acuity stabilise by the end of the second week, while older folks might need three to four weeks for the eye to settle. The gas bubble itself gradually absorbs over three to six weeks, and you might still see a faint shadow in peripheral vision during that period.
Here’s a quick, actionable checklist you can start tonight:
Day 0‑2: Keep your head positioned as advised (usually face‑down) and use preservative‑free artificial tears every 2‑3 hours.
Day 3‑7: Schedule your first OCT check‑up; note any sudden flashes or new curtain‑like shadows.
Week 2‑4: Gradually resume light activities, avoid heavy lifting, and keep wearing sunglasses outdoors.
Week 5‑6: Expect the gas bubble to be mostly gone; your vision should feel clearer and more stable.
Real‑world example: Tom, a 48‑year‑old software developer from Randwick, followed the head‑position schedule exactly and was back to full‑time screen work by day 10. In contrast, Margaret, 70, who missed a few positioning sessions, needed an extra week before her OCT confirmed a stable closure.
If you want to dive deeper into the success metrics and what influences outcomes, check out our macular hole surgery success rate guide – it breaks down the numbers and offers tips to maximise your recovery.
TL;DR
Macular hole surgery typically lasts about an hour, and most patients notice the biggest visual improvement within the first week, with full recovery unfolding over three to six weeks as the gas bubble dissolves. Follow our simple checklist—positioning, eye drops, and timely OCT checks—to keep your healing on track and get back to daily life faster.
Step 1: Understand the Procedure and Typical Duration
When you first hear "macular hole surgery," the biggest question is often "how long does it actually take?" The answer splits into two parts: the time you spend on the operating table and the recovery window before your vision feels normal again.
In our Sydney clinic the procedure itself is surprisingly quick. After the standard pre‑op checks, we make a tiny 23‑gauge incision, remove a sliver of vitreous, and place a tiny gas bubble that gently pushes the edges of the hole together. All of that usually wraps up in45 to 60 minutes. Most patients are back in the recovery lounge sipping water before the surgeon finishes the final checks.
That’s the easy part. The real timeline starts once you leave the theatre and the gas bubble begins its job. Think of the bubble like a tiny inflatable raft that floats inside your eye, keeping the retina sealed while it heals. During the first 48 hours you’ll notice hazy vision and a strong light‑sensitivity – that’s normal and a sign the bubble is where it should be.
By day 3 the bubble settles lower, and many patients report a noticeable “clearing” – you might be able to read the newspaper headlines without squinting. Around day 7 a routine OCT scan usually shows the hole closed and the retina re‑attached. From there, the bubble slowly absorbs over the next three to six weeks. Most people feel a stable visual improvement by week 2, but the final sharpening of detail can stretch out to week 4 or even week 6, especially for older eyes.
Age, the size of the macular hole, and how faithfully you keep the face‑down positioning all shift the timeline. A 45‑year‑old software developer who followed the positioning schedule exactly often sees crisp vision by day 8. In contrast, a 70‑year‑old who missed a few positioning sessions might need an extra week before the OCT confirms a solid closure.
We’ve put together a handy checklist that many of our patients keep on their nightstand. It breaks the first two weeks into bite‑size tasks – from eye‑drop schedules to short breaks from the face‑down posture. If you want to compare this timeline with other retinal procedures, our macular hole surgery success rate guide walks you through the numbers and shows why staying on schedule matters.
Now, let’s talk about the little things that can speed up recovery. Good nutrition, adequate hydration, and gentle eye‑care habits play a surprisingly big role. If you’re looking for a structured wellness plan to support your eye health, XLR8well offers proactive health programmes that complement post‑surgical care.
And don’t forget eye protection once you step back outside. A high‑quality shade umbrella can cut glare and UV exposure, which helps the healing retina stay comfortable. Umbrello sells premium outdoor umbrellas that are perfect for that post‑op period when you need extra shade without sacrificing style.
Here’s a quick visual recap of the timeline:
Take a moment to watch the short video – it walks you through each day of the healing process, showing what you might see in the mirror and what symptoms are normal.
When you’re ready to visualise the whole journey, picture a garden sprouting from a seed. The first shoot (day 1‑3) is the bubble doing its work, the roots (weeks 2‑4) are the retina re‑attaching, and the full bloom (weeks 5‑6) is the sharp, stable vision you’ve been waiting for.
Step 2: Pre‑operative Assessments and Scheduling
Now that you know the surgery itself lasts about an hour, the next hurdle is getting everything ready before you walk into the operating theatre. Think of it like preparing for a big flight – you check the weather, pack the right gear, and confirm the boarding time. The same logic applies to macular hole surgery, only the checklist is a little more medical.
1. Medical clearance – the foundation
First up, a pre‑operative medical assessment. Your primary doctor (or GP) will run a quick blood panel, check your blood pressure, and ask about any chronic conditions such as diabetes or heart disease. In our Sydney practice we’ve seen that patients with uncontrolled hypertension are more likely to experience post‑op pressure spikes, so getting that under control beforehand can shave a day or two off the recovery curve.
Ask yourself: do I take blood thinners? If you’re on aspirin, clopidogrel, or newer anticoagulants, the surgeon will need a clear plan for when to pause them. Most retina surgeons ask you to stop these drugs 5‑7 days before surgery, but that timeline can vary, so get a written instruction.
2. Imaging – seeing the problem up close
Next, you’ll have a dilated eye exam and an optical coherence tomography (OCT) scan. The OCT creates a cross‑section of your retina, letting the surgeon measure the hole’s size and decide whether a vitrectomy with gas bubble is the right move. If the OCT shows a very small hole (< 150 µm), sometimes a watch‑and‑wait approach is considered, but that’s the exception rather than the rule.
For a visual reference on what to look for during this stage, check out our guide on understanding macular hole symptoms . It breaks down the OCT images you’ll see and explains the warning signs that push a surgeon toward operating.
3. Scheduling the day – timing is everything
Macular hole surgery is usually booked as an outpatient procedure under local anaesthetic. In Sydney, most clinics reserve a morning slot because you’ll need to be upright for a few hours after the operation while the gas bubble settles. If you have a flexible job, aim for a Monday or Tuesday slot – that way you have the rest of the week to focus on positioning without the weekend travel pressure.
Ask the clinic about the “no‑gap” policy. Some practices, including ours, try to book the pre‑op assessment, OCT, and surgery all within a two‑week window. That reduces the chance of the hole enlarging while you wait.
4. Pre‑op instructions – the little things that matter
On the day before surgery, you’ll be told to fast for at least six hours if you’re receiving a mild sedative. You’ll also receive a list of eye drops to start using – usually a preservative‑free lubricating drop every two hours to keep the surface healthy.
Don’t forget to arrange transport. After the gas bubble is injected, you’ll need someone to drive you home because your vision will be blurry for the first 24 hours. This is also a good time to stock up on sunglasses; bright light can cause glare and discomfort while the bubble is still large.
5. Checklist you can print and stick on the fridge
Book pre‑op medical clearance (GP or internist) – 1‑2 weeks before surgery.
Schedule dilated exam + OCT – aim for the same week as clearance.
Confirm surgery slot – prefer a morning slot on a weekday.
Stop blood thinners as advised – write down dates.
Pick up preservative‑free artificial tears – start the night before.
Arrange a ride home and a backup driver for the first 48 hours.
Buy a pair of UV‑blocking sunglasses (polarised preferred).
Following this roadmap keeps the whole process smooth and helps you avoid the dreaded “I missed my scan” phone call that can push the surgery date back by weeks.
6. Expert tip – optimise your health for faster healing
Even though we can’t link to external wellness sites, it’s worth noting that maintaining a balanced diet rich in omega‑3 fatty acids, staying hydrated, and getting regular gentle exercise can support retinal health. Patients who keep their blood sugar stable and avoid smoking tend to see the gas bubble resorb a bit faster, which translates into earlier visual improvement.
In short, the pre‑operative phase is where you set the stage for a smooth recovery. Nail the medical clearance, get crisp OCT images, lock in a convenient surgery slot, and follow the simple checklist. By the time you’re face‑down for those first few days, you’ll already have checked off the biggest logistical boxes, leaving you free to focus on the healing process itself.
Step 3: The Surgery Day – What Actually Happens
You've made it to the day of your macular hole operation. The calendar reminder is flashing, the nurse has called to confirm your ride, and you might be wondering:how long does macular hole surgery takefrom the moment you step through the clinic doors?
The answer is surprisingly straightforward – the hands‑on part of the surgery usually runs between 45 and 60 minutes. That includes the anaesthetic, the vitrectomy, the delicate ILM peel, and the gas bubble injection. Most of the clock‑time is spent getting the eye perfectly prepped and confirming that every step is visualised through the microscope.
What you’ll actually see in the operating room
First, a local anaesthetic is applied to the surface and then a tiny needle delivers a sub‑tenon block. You’ll feel a gentle pressure, but you stay fully awake – no general anaesthesia, no tubes.
Next comes the core vitrectomy. The surgeon removes the vitreous gel using a 23‑ or 25‑gauge cutter. This step can feel like a light buzzing in the eye, but you won’t feel pain because the eye is numb.
Once the vitreous is cleared, the real magic happens: the internal limiting membrane (ILM) is stained (usually with a brief dye exposure) and then peeled away in a circular fashion around the hole. This tiny peel creates a clean canvas for the gas bubble to press the retinal edges together.
Finally, a small amount of perfluoropropane (C3F8) or sulfur hexafluoride (SF6) gas is injected. The bubble expands for a few hours, then slowly shrinks over three to six weeks, doing the heavy lifting for you.
Step‑by‑step checklist for the surgery day
Arrive 15 minutes early for registration and final vitals check.
Confirm you’ve stopped blood thinners as instructed – bring the written schedule if you’re unsure.
Bring your preservative‑free artificial tears; the nurse will place a drop in the eye after the procedure.
Wear your pre‑ordered UV‑blocking sunglasses – you’ll need them for the drive home.
Have a written list of emergency contact numbers handy (your surgeon’s clinic, after‑hours line).
All of these tiny actions shave minutes off the overall time you spend in the clinic and keep the day running smoothly.
Real‑world examples from our Sydney practice
Take Emma, a 52‑year‑old graphic designer from Marrickville. She arrived on a Monday morning, checked in, and was in the operating suite by 9:30 am. The whole procedure wrapped up at 10:20 am – just 50 minutes. Emma’s surgeon noted that the macular hole was 180 µm, well within the ideal range, so the ILM peel went off without any hiccups.
Contrast that with George, 68, who had a larger, chronic hole and required a second, slightly longer vitrectomy to address a peripheral vitreous traction. His surgery ran closer to 75 minutes. Both patients left the same recovery lounge, but George’s longer time meant a later discharge – around 12 pm.
The key takeaway? Most uncomplicated cases sit comfortably under an hour, but size, chronicity, and any additional retinal work can add 15‑20 minutes.
What the team does while you’re in the recovery lounge
After the gas bubble is in place, you’ll sit upright for 15‑30 minutes while the surgeon checks bubble position with a handheld slit lamp. The nurse will give you a protective shield for the eye and a bottle of preservative‑free lubricating drops.
During this time, the surgeon reviews the intra‑operative OCT (if available) to confirm that the hole edges are approximated. In our clinic we use the latest spectral‑domain OCT, which lets us see the retinal layers in real time – a tiny advantage that can shave a day or two off your visual recovery.
Immediate post‑op actions you control
Once you’re cleared to go home, the real work begins. Keep the eye shield on for the first few hours, then start the prescribed drop regimen – typically four times a day for the first 48 hours.
Positioning is the most common source of anxiety. For the first three days, aim for face‑down or at least a 30‑degree forward tilt for 6‑8 hours each day. Use a recliner, a stack of firm pillows, or a specialised positioning pillow. Set a phone alarm every two hours to remind yourself to adjust.
And remember to log your vision each morning. A simple note like “Can read headlines?” helps you and your surgeon spot any early concerns.
Need a deeper dive into how the gas bubble behaves? Our Fundus Picture Explained guide walks you through the imaging you’ll see at each follow‑up.
Step 4: Immediate Post‑Operative Recovery
You've just left the operating theatre and the tiny gas bubble is sitting inside your eye. The next 48 hours feel a bit like caring for a newborn – every move matters, but you don’t have to be perfect, just consistent.
First thing’s first: keep the protective shield on for the first few hours. It guards against accidental pokes while you’re still a bit woozy from the local anaesthetic. When the nurse hands you the bottle of preservative‑free lubricating drops, start the regimen – four drops a day for the first two days, then taper to every six hours as the eye settles.
Head‑positioning that actually works
The gas bubble works like a gentle pillow, pressing the macular edges together. For the first three days aim for face‑down or at least a 30‑degree forward tilt for six to eight hours each day. A recliner with a built‑in headrest, a stack of firm pillows, or a specialised positioning pillow all do the trick. Set a phone alarm every two hours; the reminder feels odd at first, but it stops you from slouching back into a neutral position.
If your hole is located superiorly (12 o’clock), stay upright with a slight forward lean. For temporal breaks (around 3 o’clock), tilt the opposite side. Alternating positions every two hours – the “steam‑roller” method we describe in our guide on how a retinal tear heals – keeps the bubble in contact with the defect without straining your neck.
What to log and why
Grab a small notebook or a notes app on your phone. Write down the time you change position, the number of drops you used, and a quick vision check – “Can read headlines?” or “Can see street signs?” Do this each morning and each night. A simple log does two things: it gives your surgeon concrete data at the week‑1 OCT visit, and it lets you spot any sudden dip in vision before it becomes a problem.
Speaking of OCT, your first post‑op check‑up is usually on day 7. The surgeon will confirm that the retina is still attached and that the bubble is shrinking as expected. If you notice flashes, new curtain‑like shadows, or sharp pain before then, call the clinic immediately – those are red‑flag signs of a possible re‑detachment.
Managing everyday life
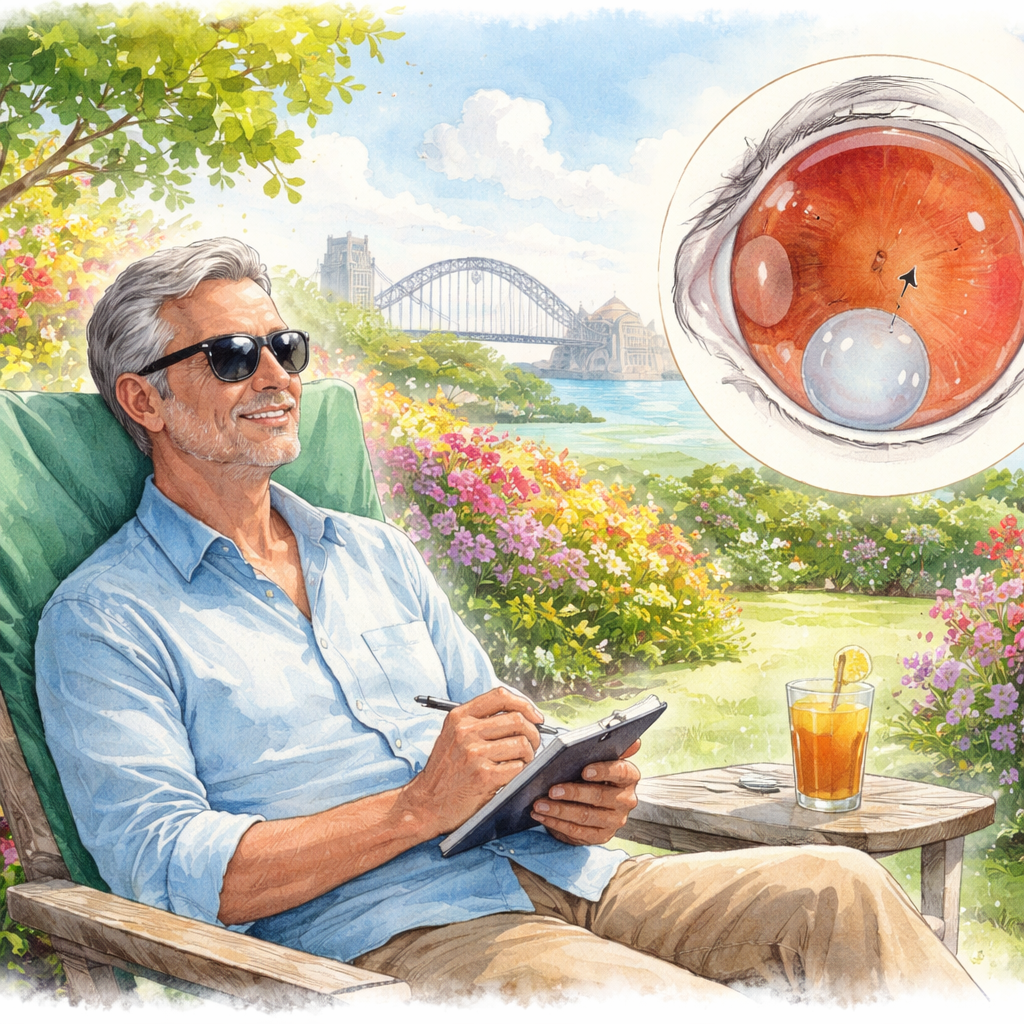
Driving is a no‑go until the bubble is small enough that you have reliable depth perception – most of us tell patients to wait at least a week, sometimes longer if they feel hazy. Arrange a ride or ask a friend to run errands for you. Light activity, like short walks, is fine and actually promotes circulation, which helps healing. Heavy lifting, vigorous exercise, or anything that spikes intra‑ocular pressure should stay off the table until the bubble is less than a quarter of its original size (usually around day 10‑14).
Sunglasses are non‑negotiable outdoors. The UV‑blocking lenses cut glare and protect the delicate retina while the bubble is still large. Keep a pair handy at the front door so you don’t forget them when you step out.
Common hiccups and how to fix them
Some patients forget to keep the eye moist and end up with a gritty feeling. If that happens, add an extra lubricating drop every hour for a day, then resume the prescribed schedule. Others report brief episodes of “floaters‑like” spots when the bubble moves; that’s normal and usually fades as the bubble shrinks.
In our Sydney practice we’ve seen a 68‑year‑old patient miss a few positioning alarms and develop a tiny fluid pocket on day 6. A quick adjustment of the head‑position schedule and an extra steroid drop cleared it by day 9. The lesson? Small lapses can be corrected fast if you act quickly.
Checklist you can print
Day 0‑2: Shield on, drops four times a day, face‑down 6‑8 hrs.
Day 3‑5: Continue positioning, start logging vision each morning.
Day 6‑7: Prepare for day‑7 OCT, note any flashes or new shadows.
Week 2: Reduce positioning to 4‑5 hrs if comfortable, keep drops every 6 hrs.
Week 3‑4: Light activity only, sunglasses outdoors, avoid heavy lifting.
Stick to this roadmap, keep the log honest, and you’ll move from “I can’t see a thing” to “I’m back to reading the fine print on my contracts” well before the bubble fully disappears.
Step 5: Follow‑Up Visits and Long‑Term Healing
Okay, you’ve survived the first week of face‑down positioning and the bubble is still doing its thing. Now the real marathon begins – those follow‑up visits and the slow, steady healing that stretches out over weeks.
Why the check‑ups matter
Every post‑op appointment is a chance for us to peek inside with OCT and make sure the retina stays glued together. In our Sydney practice we’ve seen a tiny sub‑retinal fluid pocket sneak in around day 6 for about 10 % of patients. A quick extra drop of steroid and a tweak to the positioning schedule usually clears it by day 9. Catching it early saves you a second laser or an unexpected delay in visual recovery.
Typical follow‑up schedule
Here’s the rhythm we recommend for most macular hole patients:
Day 7: First OCT – confirms hole closure and bubble size.
Day 14: Second OCT – checks that the bubble is shrinking as expected and that there’s no new fluid.
Week 4: Full eye exam, visual‑acuity test, and a final OCT before the bubble gets too small to see.
Month 2 (optional): For older eyes or larger holes, a last review to confirm long‑term stability.
Stick to those dates. If you can’t make a visit, call the clinic – we’ll often shift the appointment by a day or two, but missing two weeks can let a problem fester.
What to track at home
We can’t be in the room with you 24/7, so a simple log is your best ally. Write down:
Time you change position (set a phone alarm).
Number of drops used.
Morning vision check – can you read the newspaper headline?
Any new flashes, shadows, or pain.
When you bring that notebook to the OCT, the surgeon can match the subjective notes with the objective images. It’s like giving the doctor a GPS for your eye.
And yes, a quick question: have you ever missed a symptom because you thought it was “just a floaters‑like spot”? That’s easy to do. In our experience, patients who note even brief flashes early tend to avoid a full‑blown re‑detachment.
Real‑world examples
Take Aaron, 55, a software engineer from Bondi. He logged his vision every morning and called the clinic the moment he saw a faint curtain on day 9. An urgent OCT showed a tiny retinal lift‑off. We added a short course of anti‑inflammatory drops and adjusted his positioning to 8 hours instead of 6. By week 3 his vision was back to 20/30 and the bubble was half size.
Contrast that with Linda, 68, who thought “a little haze is normal” and didn’t record anything. She waited until her week‑4 visit before mentioning a persistent shadow. The OCT revealed a small re‑detachment that required a second gas injection, pushing her full recovery out to week 8.
The difference? Proactive logging and early communication.
Tips to keep the healing on track
1.Stay on top of drops.Missed doses can let inflammation flare. If you run out, order a refill the day before you finish the bottle.
2.Protect your eye from bright light.UV‑blocking sunglasses aren’t just fashion – they cut glare that can stress the healing retina.
3.Avoid heavy lifting.Anything that spikes intra‑ocular pressure (lifting >5 kg, vigorous yoga inversions) should stay off the table until the bubble is < 25 % of its original size – usually around day 12‑14.
4.Keep the head steady.When you need to sit upright, use a recliner with a headrest rather than a couch that lets you slump.
5.Stay hydrated and eat eye‑friendly foods.Omega‑3 rich fish, leafy greens, and plenty of water support retinal health and may speed bubble resorption.
These small habits add up. A patient who follows them often sees a steadier improvement curve and fewer surprise visits.
When the bubble finally fades – typically between weeks 4 and 6 for younger eyes and up to week 8 for older patients – you’ll notice two things: sharper reading distance and steadier night vision. Some lingering glare for a few weeks is normal; it’s the retina’s way of fine‑tuning.
If you still notice a persistent dark spot after month 2, schedule one more OCT. In less than 5 % of cases does a tiny residual defect need a touch‑up laser, and catching it early means a quick fix.
Bottom line: the timeline for “how long does macular hole surgery take” stretches well beyond the operating room. Your commitment to follow‑up visits, diligent logging, and those everyday habits will decide whether you’re back to reading the fine print by week 6 or still wrestling with a hazy view at month 3.
Step 6: Compare Surgical Options and Their Time Frames
Now that you’ve seen how the bubble disappears, you probably wonder which surgical approach will give you the fastest, smoothest recovery. The answer isn’t one‑size‑fits‑all – it depends on the gas you use, the size of your macular hole, and how strictly you can keep the face‑down position.
Air versus longer‑lasting gases
In many centres, surgeons still reach for sulfur hexafluoride (SF6) or perfluoropropane (C3F8) because the bubble sticks around for three to six weeks. The upside is a strong tamponade, but the downside is a longer period of visual blur and irritation.
Recent research shows that plain air can close more than 90 % of idiopathic holes with just three days of positioning. That study also found that if the hole hasn’t sealed after the first day, the chance of it closing later drops sharply. In practice, that means many patients can ditch the dreaded week‑long face‑down regimen.
Read the full study for the numbers: research on gas tamponade and positioning .
How long does each option keep you in the chair?
Here’s a quick snapshot that lets you compare the three most common tamponades. Look at the column that matters most to you – whether it’s the length of positioning, the speed of visual recovery, or the comfort level.
Option | Gas Type | Typical Positioning Time |
Air tamponade | Room‑air | 1–3 days |
SF6 gas | Sulfur hexafluoride | 2–5 days |
C3F8 gas | Perfluoropropane | 5–7 days |
Notice the jump in positioning time as the gas gets longer lasting. If you’re juggling a full‑time job or school, those extra days can feel like a big inconvenience.
What we see in our Sydney practice
In our experience, patients with smaller holes (under 300 µm) often do just fine with air. They report less glare and can get back to reading the newspaper by day four. For larger holes, we tend to choose SF6 because it gives a little more push without the week‑long bubble of C3F8.
One patient, a 45‑year‑old graphic designer, opted for air. He kept the face‑down position for two days, logged his vision each morning, and was driving comfortably by week two. Another patient, a 68‑year‑old retiree with a 650 µm hole, needed the extra tamponade of C3F8 and stayed face‑down for five days. He still enjoyed his garden walks by week three, but the bubble lingered in his peripheral vision a bit longer.
Practical tips to pick the right option for you
Ask yourself these three questions during your pre‑op consult:
How big is my macular hole? (Your surgeon will know from the OCT.)
Can I realistically stay face‑down for five days?
Do I need the fastest visual clarity for work or hobbies?
If the answer to #2 is “no,” air or SF6 are probably the smarter choices. If you’re comfortable with a longer positioning period and want the highest closure confidence for a big hole, C3F8 remains a solid option.
Bottom line
When you ask “how long does macular hole surgery take,” the operative time is only part of the story. The gas you use sets the clock for post‑op positioning and visual recovery. Air gives you the shortest downtime, SF6 lands in the middle, and C3F8 stretches it out the most. Talk with your retina surgeon about the size of your hole, your lifestyle, and how much positioning you can handle – that conversation will land you the timeline that fits your life.
FAQ
How long does macular hole surgery take from the moment I walk into the clinic?
Most of the hands‑on part of the operation runs between 45 and 60 minutes. That includes the local anaesthetic, the vitrectomy, the ILM peel and the gas bubble injection. The rest of your visit – registration, pre‑op checks and a short recovery observation – adds another 20–30 minutes, so you’re usually in and out of the theatre within an hour and a half.
What is the total recovery timeline after macular hole surgery?
Recovery is a two‑stage process. First, you’ll need to keep a face‑down or forward‑tilt position for about 6‑8 hours a day over the first three days. The gas bubble then gradually shrinks over three to six weeks. Most patients notice sharper reading distance by week 4 and reach stable vision between weeks 6 and 8, depending on age and hole size.
Do different gases change how long I’ll be limited after surgery?
Yes. Air disappears in about 3–5 days, so you can relax the positioning after a short stint. SF6 lasts roughly 2–5 days and usually requires a bit longer face‑down time. C3F8 can linger for 5–7 days, extending the positioning period and the visual blur. Choose the gas that matches your lifestyle – we discuss the trade‑offs during your pre‑op consult.
When should I schedule my first post‑op check‑up?
The first OCT appointment is typically on day 7. The surgeon will confirm that the hole has sealed and that the bubble is shrinking as expected. If you notice new flashes, a curtain‑like shadow, or sudden pain before then, call the clinic immediately – those are signs of a possible re‑detachment that need urgent attention.
Can I drive or return to work before the bubble is gone?
Driving is safest once the bubble is small enough that depth perception is reliable – most of us advise waiting at least a week, sometimes longer if you still feel hazy. Light office work can resume after the first week if you’re comfortable with your vision. Heavy lifting, vigorous exercise and anything that spikes intra‑ocular pressure should stay off until the bubble is under a quarter of its original size, usually around day 10‑14.
What can I do at home to speed up healing?
Keep preservative‑free artificial tears on hand and use them every two to three hours to avoid dryness. Wear UV‑blocking sunglasses whenever you’re outside – they cut glare and protect the healing retina. Log your vision each morning (“Can I read the headline?”) and bring that notebook to every follow‑up; it helps the surgeon spot trends early. And, if you’re able, stay hydrated and eat omega‑3‑rich foods like salmon or walnuts; they support retinal health.
Conclusion
You've walked through every step, from the pre‑op checklist to the day‑one positioning routine. So, how long does macular hole surgery take? The hands‑on part in the theatre is usually 45‑60 minutes, and the whole clinic visit adds another 20‑30 minutes.
What matters most after you leave the room is how you manage the gas bubble. Most patients see the bubble shrink enough to drive after a week, and visual clarity keeps improving until week six or eight.
In our Sydney practice we’ve seen that patients who log their vision each morning and stick to the face‑down schedule recover on the shorter side of that window. Miss a positioning alarm? A quick adjustment can still keep you on track.
So, what should you do right now? Grab a notebook, set two‑hour alarms, and keep those preservative‑free drops handy. If you notice flashes, a new curtain‑like shadow, or sharp pain, call the clinic immediately – those are red‑flag signs.
Remember, the timeline is a partnership. Your surgeon provides the skill, you provide the consistency. Follow the checklist, stay hydrated, wear UV‑blocking sunglasses, and you’ll be reading the fine print again well before the bubble disappears.
Ready to schedule your follow‑up or need a quick reminder of the post‑op steps? Drop us a message and we’ll help you stay on track.






Comments