What Is Vitreous Hemorrhage: A Complete Guide for Patients
- Dr Rahul Dubey
- Jan 15
- 17 min read
Imagine waking up one morning and noticing a sudden cloud of red specks drifting across your vision, like tiny fireworks in the back of your eye. That feeling is often the first clue that something called vitreous hemorrhage is happening.
In plain terms, vitreous hemorrhage is bleeding into the clear gel‑like substance (the vitreous) that fills the space between the lens and the retina. When blood leaks into that gel, it scatters light and creates the floaters, shadows, or hazy curtain you might see. It’s not just a nuisance – it can signal an underlying retinal problem that needs prompt attention.
So why does the vitreous start bleeding? The most common triggers are retinal tears, diabetic retinopathy, or age‑related changes that cause the retina to pull away (posterior vitreous detachment). For example, a 62‑year‑old patient in Sydney who came to our clinic after a sudden “rain‑storm” vision described it as “seeing a burst of blood in my eye after a brisk walk on the harbour foreshore.” A quick scan showed a small retinal tear, and we scheduled a laser seal to stop further bleeding.
Another real‑world scenario: a younger adult with uncontrolled diabetes may develop fragile new vessels on the retina. Those vessels can rupture, spilling blood into the vitreous. In our practice, we’ve seen patients who thought the floaters would disappear on their own, only to notice worsening vision and a dark spot growing larger. Early intervention with anti‑VEGF injections or vitrectomy often preserves sight.
What should you do if you suspect vitreous hemorrhage? Here are three actionable steps: (1) Stop any strenuous activity and avoid rubbing the eye; (2) Book an urgent appointment with a retina specialist – time matters; (3) Keep a note of any recent eye trauma, flashes of light, or sudden vision changes to share with the doctor. You can read more about the typical causes in our detailed guide Vitreous Hemorrhage Causes: What Triggers This … .
While you’re sorting out appointments, consider supporting your overall eye health with lifestyle tweaks – balanced diet, regular blood‑sugar checks, and staying hydrated. Platforms like XLR8well offer proactive health programs that complement eye‑care by focusing on nutrition and wellness, which can help reduce the risk of future bleeding events.
Bottom line: vitreous hemorrhage is a warning sign, not a diagnosis. By recognizing the symptoms early and acting fast, you give yourself the best chance to keep your vision clear and enjoy Sydney’s beautiful sunsets without the unwanted “rain” in your eyes.
TL;DR
Vitreous hemorrhage is bleeding into the eye’s clear gel, causing sudden floaters, shadows, or a curtain‑like haze that can signal retinal tears, diabetic damage, or age‑related changes.
If you notice these signs, stop activity, avoid rubbing, and book an urgent retinal specialist appointment—early treatment such as anti‑VEGF injections or vitrectomy can preserve your vision.
Understanding Vitreous Hemorrhage
When you first hear the term vitreous hemorrhage, it probably sounds like medical jargon you’d only find in a textbook. In plain English, it simply means that blood has leaked into the clear, jelly‑like substance (the vitreous) that fills the back of your eye.
Why does that happen? The most common culprits are tiny tears in the retina, fragile new vessels that grow in diabetic retinopathy, or the natural pulling apart of the vitreous as we age—what eye doctors call a posterior vitreous detachment.
Imagine you’re on a weekend walk around the harbour, and suddenly a cascade of red specks flutters across your vision like confetti. That’s the blood scattering in the vitreous, and it can turn a clear view into a curtain‑like haze within seconds.
The good news is that vitreous hemorrhage itself rarely destroys vision permanently. What’s risky is what lies underneath—usually a retinal tear that could progress to a retinal detachment if left untreated.
In our Sydney clinic, we often see patients who think the floaters will fade on their own. More often than not, the bleeding settles in layers, making the “curtain” thicker each day. That’s a sign you need to act fast.
How do we confirm it’s a vitreous hemorrhage and not something else? A quick dilated eye exam lets us look through the pupil with special lenses. If we spot blood floating in the vitreous, we’ll also check for retinal tears, holes, or signs of diabetic retinopathy.
When a retinal tear is found, we can seal it in the office with laser photocoagulation—think of it as tiny stitches that prevent the tear from widening and bleeding further.
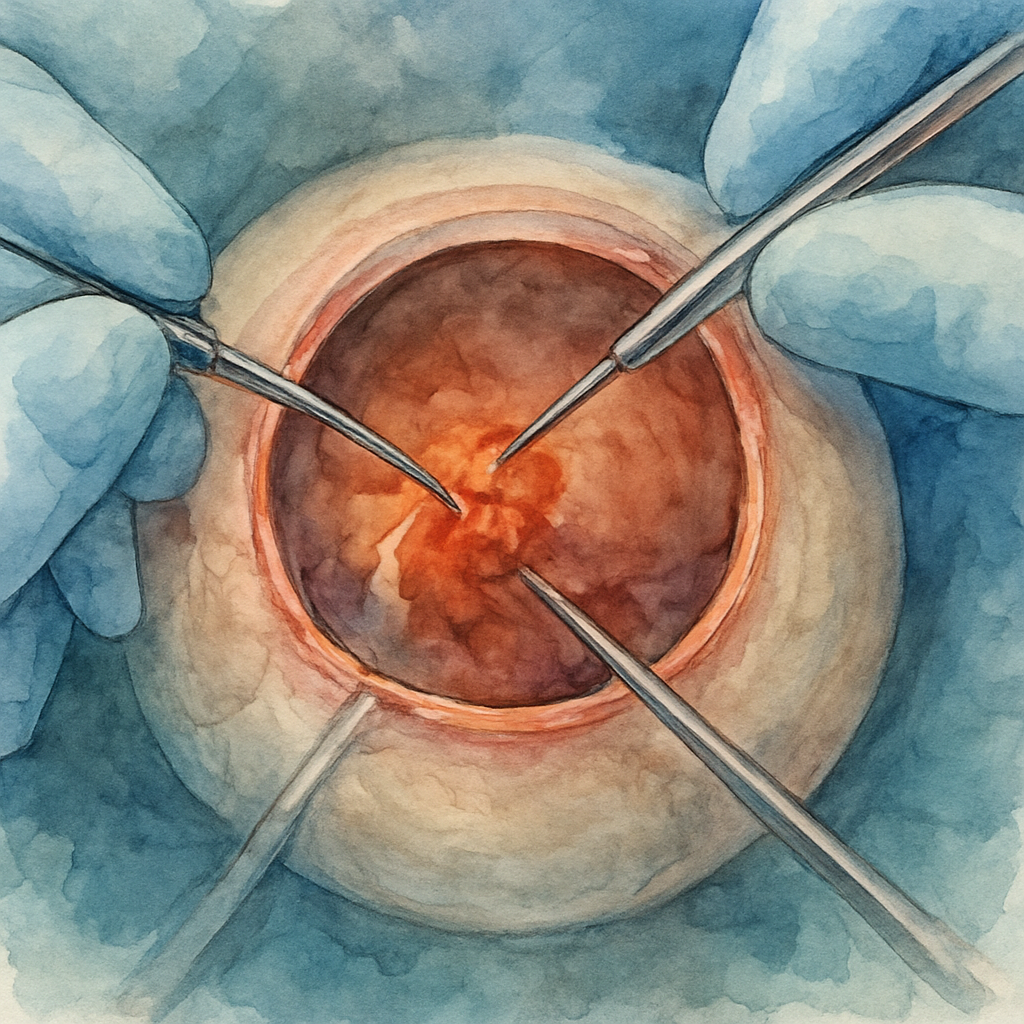
If the blood is dense or the retina is already detached, we may recommend a vitrectomy. During that procedure, we remove the vitreous gel and any clotted blood, then replace it with a clear saline solution. Modern vitrectomy has a success rate above 90 % for restoring vision when done promptly.
You might wonder whether lifestyle can influence the risk of bleeding. While you can’t control age‑related vitreous changes, keeping blood sugar stable, staying hydrated, and protecting your eyes from blunt trauma all help reduce the odds of a tear.
If you’re a visual learner, this short video walks through what you’d see during an eye exam for vitreous hemorrhage.
Notice how the ophthalmologist gently shines a light and uses a special lens to spot the floating blood cells. That same technique helps us decide whether laser or surgery is needed.
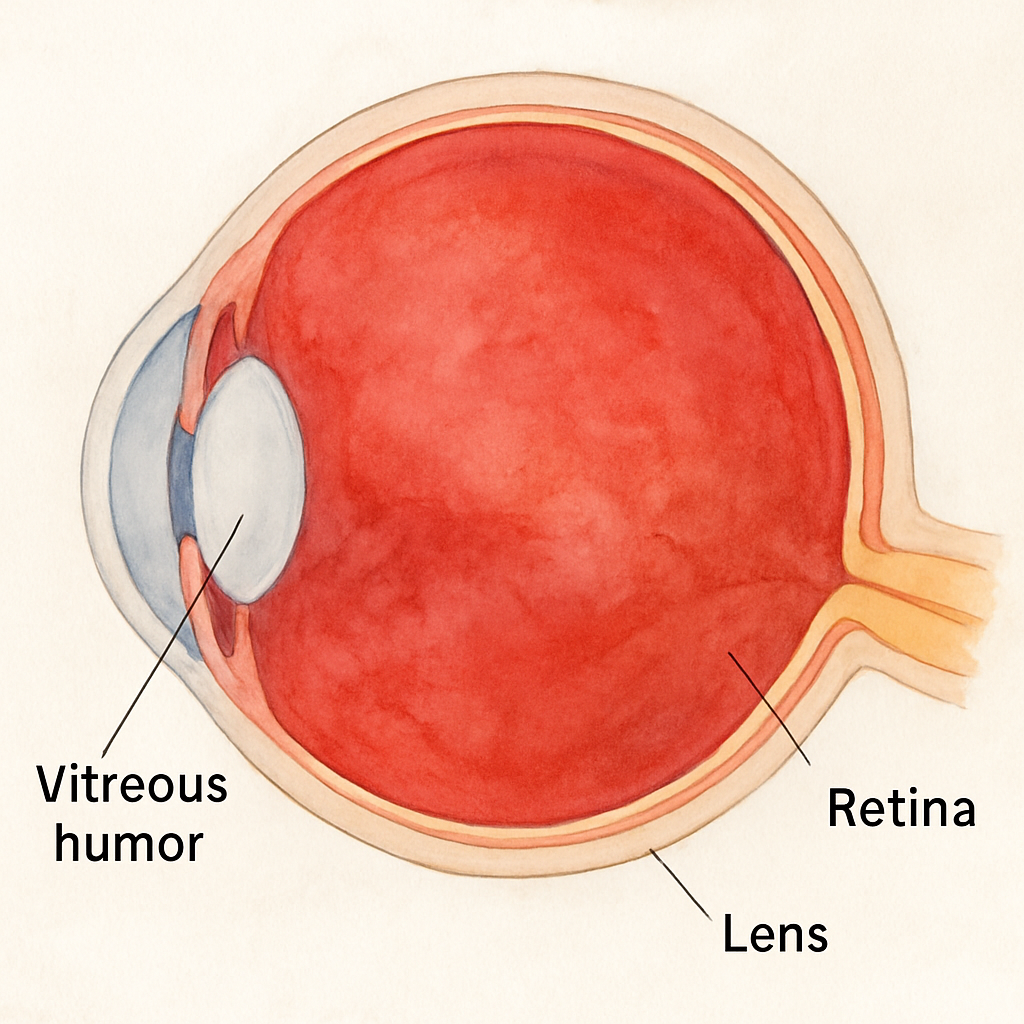
Below is a simple illustration of the eye’s anatomy, showing where the vitreous sits relative to the retina and lens.
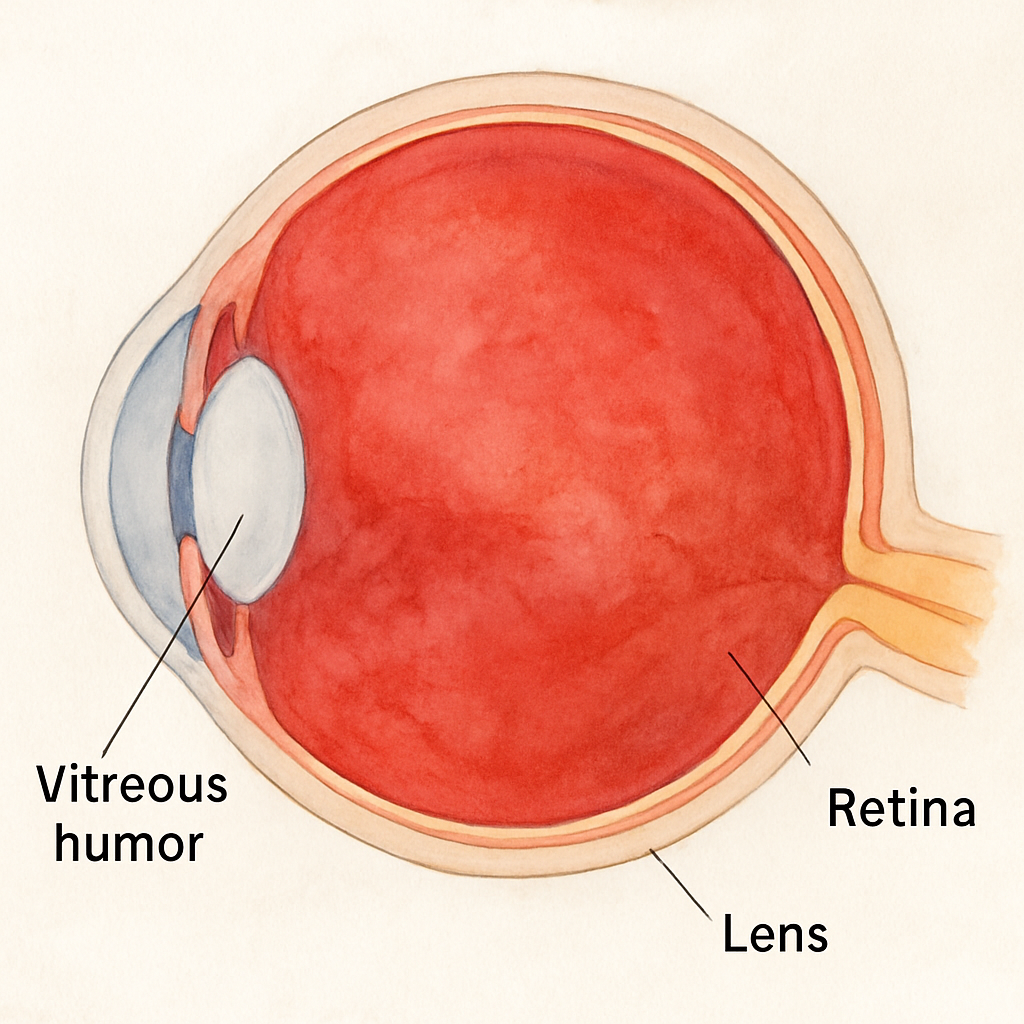
Understanding where the bleeding occurs helps you grasp why the visual disturbance looks like a curtain or a swarm of specks—light is simply being scattered by blood instead of passing cleanly through the gel.
If you notice any sudden floaters, shadows, or a dark curtain, pause what you’re doing, avoid rubbing the eye, and call your retinal specialist within 24 hours. Early assessment gives the best chance to preserve your sight.
Causes and Risk Factors
When that sudden curtain of red specks appears, it’s natural to wonder why your eye decided to throw a little party inside. The short answer? Something’s letting blood leak into the vitreous, and a handful of common culprits tend to be the party crashers.
First up, retinal tears. Imagine the retina as a delicate wallpaper glued to the back of your eye. A sudden tug – maybe from a vigorous swing on the harbour bridge or an unexpected cough – can rip that wallpaper just enough for tiny vessels to burst. In my clinic, I’ve seen a 58‑year‑old Sydney‑based cyclist who felt a flash of light after a hard stop on a hill. A quick dilated exam revealed a peripheral retinal tear, and a laser seal saved his vision before the bleed got out of hand.
Then there’s proliferative diabetic retinopathy (PDR). High blood sugar builds fragile, new‑growth vessels on the retina that are prone to rupture. A recent study of 579 eyes with diabetic retinopathy found that uncontrolled glycated haemoglobin (HbA1c) levels were a massive predictor of recurrent vitreous haemorrhage after surgery (OR ≈ 21) (Springer study) . In plain terms, the higher your A1c, the more likely those delicate vessels will leak.
Age‑related changes also play a starring role. As we get older, the vitreous gel slowly liquefies and pulls away from the retina – a process called posterior vitreous detachment (PVD). Most of the time it’s harmless, but in about 22 % of cases it creates enough traction to tear the retina, especially in people with high myopia. That’s why we often remind our patients who wear glasses for distance to get an eye check if they notice new floaters after a weekend of beach volleyball.
Systemic hypertension is another silent accomplice. Elevated blood pressure stiffens retinal arterioles, making them brittle. When a sudden spike occurs – think of a stressful meeting or a heavy lifting session – those vessels can give way. A 2024 NCBI review notes that hypertension, alongside diabetes, accounts for a large share of intra‑ocular haemorrhages (NCBI) . Managing your BP with lifestyle tweaks or medication can shave off a lot of risk.
Blood‑thinning medications are a double‑edged sword. If you’re on aspirin, warfarin, or newer anticoagulants, even a minor eye trauma can turn into a full‑blown bleed. One of my patients on long‑term anticoagulation after a heart valve replacement came in after a minor garden rake accident; the bleed lingered for weeks because his clotting was deliberately suppressed.
So, what can you do to keep those risk factors in check?
Control diabetes rigorously – aim for an HbA1c below 7 % if possible. Regular eye exams every six months are a must.
Maintain blood pressure within the 120/80 mmHg range. Salt reduction, regular exercise, and stress‑management techniques (like a short walk by the harbour) help.
If you’re on anticoagulants, discuss with your cardiologist whether a dose adjustment is safe before any eye‑intensive activity.
Stay alert to symptoms: sudden floaters, flashes of light, or a “curtain” effect should prompt an urgent call to a retina specialist.
Consider protective eyewear during high‑risk activities (e.g., sports, DIY projects) to minimise trauma.
And remember, you don’t have to navigate this alone. For a deeper dive into the top triggers behind vitreous haemorrhage, check out our guide Vitreous Hemorrhage Causes: What Triggers This … . Understanding the why helps you act faster, and fast action often means a simple laser or injection instead of a more invasive surgery.
Symptoms and When to Seek Care
Imagine you’re sipping a flat white on the balcony and suddenly a curtain of red specks drifts across your vision. That moment feels like someone turned on a faulty projector inside your eye. It’s unsettling, right? That’s often the first clue that a vitreous haemorrhage is happening.
Most people notice painless floaters that look like tiny fireworks, a hazy veil that seems to settle over the centre of their view, or a sudden loss of sharpness. The blood settles at the bottom of the gel, so the “cloud” can look worse in the morning when you’ve been lying down – the particles have drifted under the macula.
Common symptom patterns
• Floaters that appear out of nowhere and don’t fade within a few days.
• A shadow or “curtain” that moves as you shift your gaze.
• Occasional flashes of light, especially after a brisk walk or a sudden head movement.
• Mild discomfort or a feeling of pressure, but rarely pain.
One of my patients, a 61‑year‑old cyclist from Bondi, described the floaters as “tiny red confetti after a ride”. He thought it would clear on its own, but by the evening the vision‑blocking veil had grown. That’s a classic red‑flag that something needs professional attention.
When to pick up the phone
We love to reassure people that not every floaters need surgery, but there are clear cut‑offs where waiting becomes risky. Call your retina specialist (or head straight to the emergency department) if you notice any of the following:
Sudden, significant loss of vision – you can’t read a street sign or recognise a familiar face.
The “curtain” covers the central visual field, making it hard to drive or read.
Accompanying pain, redness, or a noticeable increase in eye pressure.
Flashes of light that persist for more than a few seconds, especially after an eye‑trauma or vigorous activity.
Symptoms that worsen over a day or two rather than improve.
These signs often point to an underlying retinal tear or detachment, which can progress quickly. In our Sydney clinic, we’ve seen a 48‑year‑old DIY enthusiast who ignored a brief flash after hammering a wall. Within 24 hours the bleed expanded, and we had to perform an urgent laser seal to prevent a full‑thickness detachment.
Quick self‑check checklist
Before you book an appointment, run through this short checklist. Keep a pen handy and note what you experience – it helps the doctor piece together the puzzle.
When did the symptoms start? (Exact date and time if you can.)
What did you see? (Floaters, veil, colour, size, movement.)
Any recent eye trauma, heavy lifting, or sudden head movement?
Do you have diabetes, high blood pressure, or are you on blood‑thinners?
Have you noticed similar episodes in the past?
Bring this list to your consultation. It speeds up the history‑taking and lets us focus on the exam.
What the exam looks like
During the visit we’ll dilate your pupils and use an indirect ophthalmoscope to scan the retina. If the blood is too dense, a B‑scan ultrasound helps us see whether a retinal break is hiding beneath the haze. In many cases we can spot the source of the bleed without waiting for the blood to clear.
For a deeper dive into what a flash of light might mean and how to act, check out our guide on flashes of light in one eye . It walks you through the same red‑flag symptoms we’re discussing here.
Practical steps you can take right now
1. Stop any strenuous activity – no heavy lifting, intense sports, or garden raking until you’ve been evaluated.
2. Keep your head slightly elevated, especially when you sleep, so the blood settles away from the macula.
3. Avoid rubbing the eye; friction can aggravate a hidden tear.
4. If you’re on anticoagulants, note the dosage and bring it to the appointment – we may need to coordinate with your cardiologist.
5. Schedule an urgent appointment (ideally within 24‑48 hours) with a retina specialist. Early laser or anti‑VEGF treatment can stop the bleed and preserve vision.
Remember, vitreous haemorrhage is a warning sign, not a diagnosis. Prompt action often means a quick office procedure rather than a more invasive vitrectomy later on. If you act fast, you’ll protect the beautiful Sydney sunsets you love to watch from your balcony.
Diagnosis and Tests
When those red specks first appear, the biggest question on your mind is probably: “What’s really going on inside my eye?” The answer lies in a systematic work‑up that lets us pinpoint the source of the bleed and decide how to stop it.
First up is a thorough history. Write down when the floaters started, any recent flashes of light, head trauma, heavy lifting, or a change in your diabetes or blood‑pressure meds. In my clinic we ask patients to bring a list of any anticoagulants they’re on – even a low‑dose aspirin can tip the balance.
Next, we dilate the pupils and take a look with an indirect ophthalmoscope. If the vitreous is packed with blood, the view can be murky. That’s where a B‑scan ultrasound becomes a lifesaver – it can reveal a hidden retinal tear or detachment even when you can’t see the retina directly.
Optical coherence tomography (OCT) is another cornerstone. It gives us a cross‑sectional map of the retina, showing whether the hemorrhage sits in the vitreous cavity, under the internal limiting membrane, or has seeped into the sub‑retinal space. In a recent study of abusive head trauma, OCT helped identify vitreous haemorrhage that covered the entire retina in 50 % of eyes, highlighting how essential imaging is for a full picture.
Fluorescein angiography (FA) isn’t always needed, but when we suspect vascular abnormalities – like proliferative diabetic retinopathy or retinal vein occlusion – it shows us leaking vessels in vivid colour. That information guides whether you’ll need anti‑VEGF injections, laser photocoagulation, or a more invasive vitrectomy.
Blood tests are the unsung heroes of diagnosis. A complete blood count, coagulation profile, and HbA1c can reveal systemic contributors. For example, patients with uncontrolled diabetes (HbA1c > 9 %) are far more likely to develop neovascular bleeds that require prompt anti‑VEGF therapy.
In children, the work‑up takes a slightly different turn. Wide‑field fundus photography is now the gold standard for spotting retinal haemorrhages that stretch from the posterior pole to the far periphery – a pattern that, in 86 % of abusive head trauma cases, involves both arteries and veins. That distribution is a red flag that the bleed is trauma‑related rather than from simple venous stasis.
So, how do you know you’re on the right track? Here’s a quick checklist you can run through before you leave the doctor’s office:
Did the clinician dilate your pupils and examine the retina directly?
Was an OCT or B‑scan performed to locate the bleed?
Are you getting blood work to rule out systemic issues?
If you’re a parent, did the doctor capture wide‑field images to assess peripheral involvement?
If any of those boxes are unchecked, call the clinic back and ask for clarification – early, accurate diagnosis can be the difference between a simple office laser and a full‑blown vitrectomy.
When the source is a retinal tear, we often seal it with a laser barrage in the same visit. If the bleed is from proliferative diabetic retinopathy, anti‑VEGF injections are the first line – they shrink the fragile vessels and clear the vitreous over weeks. For dense, non‑resolving haemorrhage, a pars plana vitrectomy removes the blood and restores vision, and our success rates in Sydney hover around 90 % for uncomplicated cases.
One practical tip that patients love: keep a simple symptom diary. Note the date, time of day, lighting conditions, and whether the floaters shift when you lie down. That record helps the retina specialist track the haemorrhage’s movement – blood settles inferiorly, so you’ll see more floaters in the morning.
And remember, the eye is a window to your overall health. If you’ve got hypertension, aim for a reading below 120/80 mmHg; if you’re on blood thinners, discuss dose adjustments with your cardiologist before any eye‑intensive activity.
For a deeper dive into what a retina specialist actually does during this diagnostic journey, check out our guide What Does a Retina Specialist Do: A Practical Guide for Patients . It walks you through each step, from dilation to possible surgery, so you know exactly what to expect.
Treatment Options and Recovery
So you’ve got the diagnosis and you’re wondering what comes next. The good news is that most vitreous haemorrhages can be managed with a clear plan, and you don’t have to live in fear of permanent vision loss.
First, we always ask yourself: how much blood are we talking about, and what’s the underlying cause? If the bleed is tiny and the retina looks stable, we often adopt a watch‑and‑wait approach. You’ll keep a symptom diary – note the time of day, lighting, whether the floaters shift when you lie down – and return for a follow‑up in a week or two. In many cases the body clears the blood on its own within eight to twelve weeks.
But if the haemorrhage is dense, or if you have proliferative diabetic retinopathy, we move to more active treatment. Anti‑VEGF injections are usually the first line. They shrink the fragile new vessels, reduce further bleeding and often clear the vitreous over a few weeks. In our Sydney clinic, we see patients report noticeable improvement in floaters after just two injections.
When the blood is stubborn – for example, a thick curtain that blocks the central field – a pars plana vitrectomy becomes the go‑to. Think of it as a tiny, precise cleanup crew that removes the blood and restores the clear gel. Our recent audit shows a success rate hovering around 90 % for uncomplicated cases, and you can read more about those numbers in this guide Vitrectomy Success Rate: What You Need to Know .
Laser photocoagulation also has its place. If we spot a retinal tear that’s the source of the bleed, we can seal it in the same visit with a laser barrage. It’s quick, painless and often prevents the need for surgery later on.
Now, let’s talk recovery. After an injection, you’ll usually resume normal activities the next day, but keep your head slightly elevated for a few nights – that helps the medication settle where it belongs. After vitrectomy, we recommend a two‑week “eye‑rest” period: no heavy lifting, no vigorous sports, and keep your eyes protected from dust or wind.
Here’s a simple checklist you can follow once you’ve had a procedure:
Day 1: Apply any prescribed eye drops exactly as instructed.
Day 2‑7: Keep the head elevated while sleeping; avoid bending over.
Week 2: Attend the post‑op review – the surgeon will check for residual blood and intra‑ocular pressure.
Week 3‑4: Gradually re‑introduce light activities; still avoid heavy lifting.
Month 1: Full vision assessment and discussion of any ongoing eye‑health steps.
What about lifestyle tweaks? Maintaining blood‑sugar control, keeping blood pressure in the 120/80 mmHg range, and moderating anticoagulant dosage (under your cardiologist’s guidance) all shave down the risk of a repeat bleed. And yes, staying hydrated helps the vitreous stay supple.
Some patients ask if there are any adjunct therapies that could support recovery. While we focus on evidence‑based medical care, a few folks find low‑level frequency devices helpful for overall wellbeing. If you’re curious, you can explore options like the Healy Frequency Device – just be sure to discuss any complementary tools with your eye surgeon first.
Below is a quick comparison of the most common treatment pathways.
Option | Typical Setting | Recovery Time |
Observation | Clinic follow‑up every 1‑2 weeks | 4‑12 weeks for natural clearance |
Anti‑VEGF injection | In‑office procedure, 1‑5 min | 1‑2 days for daily activities; vision may improve over 4‑6 weeks |
Laser seal | Office‑based laser session | Same day activity, minor eye‑irritation for a few days |
Pars plana vitrectomy | Operating theatre, general or local anaesthetic | 2‑3 weeks of limited activity; full visual recovery 4‑6 weeks |
Remember, every eye is unique. If you notice new floaters, a worsening curtain, or any pain, call your retina specialist right away. Early intervention usually means a simpler, less invasive procedure and a smoother road back to clear vision.
Bottom line: you have a toolbox of proven treatments, and with the right plan you can get back to watching those Sydney sunsets without the unwanted “rain” in your eye.
Conclusion
If you’ve made it this far, you already know that asking “what is vitreous hemorrhage?” is the first step toward protecting your sight.
We’ve seen a retiree on an arvo walk by the Harbour Bridge whose sudden “rain‑storm” vision turned out to be a tiny retinal tear, and a young professional with diabetes whose bleed cleared after a prompt anti‑VEGF injection. Those stories remind us that early detection and swift action usually keep the treatment simple.
So, what should you do next? First, write down when the floaters started, any recent flashes, and any meds you’re on. Bring that list to your retina surgeon – it speeds up the exam and helps us decide whether observation, laser sealing, or vitrectomy is right for you.
Second, protect your eye while you wait for care: keep your head elevated at night, avoid heavy lifting, and don’t rub the eye. A few minutes of caution can keep a small bleed from becoming a big problem.
Finally, remember that you’re not alone. In our Sydney practice we tailor each plan to your lifestyle – whether you need a quick office laser or a more involved vitrectomy, the goal is the same: clear vision for those sunset walks.
Take the notebook, make that call, and give your eye the chance to heal. Your next clear‑view sunrise is just a decision away.
FAQ
What is vitreous hemorrhage and what causes it?
Vitreous hemorrhage is bleeding into the clear gel that fills the inside of your eye, the vitreous. The blood scatters light, so you see floaters, a hazy veil, or a “curtain” over part of your vision. The most common triggers are a retinal tear, proliferative diabetic retinopathy, or the natural pulling apart of the vitreous (posterior vitreous detachment). Less often, trauma, high blood pressure, or blood‑thinners can set it off.
How do I know if I need urgent care?
If the floaters appear suddenly, you notice a rapid loss of central vision, or a dark curtain spreads across your sight, treat it as an emergency. Persistent pain, redness, or a sudden increase in eye pressure also demand prompt attention. In our Sydney practice we advise you to call a retina surgeon within 24 hours – the sooner the cause is identified, the easier it is to prevent permanent damage.
What tests will the retina specialist perform?
The first step is a dilated eye exam with an indirect ophthalmoscope. If the blood blocks the view, a B‑scan ultrasound will reveal hidden retinal tears. Optical coherence tomography (OCT) maps the retina’s layers and shows where the bleed sits. Occasionally we add fluorescein angiography to pinpoint leaking vessels, especially in diabetic patients. These imaging tools help us decide whether observation, laser, injection, or surgery is right for you.
Can vitreous hemorrhage clear on its own?
Small bleeds often resolve within 8‑12 weeks as the eye naturally clears the blood. You’ll still need a follow‑up to make sure the underlying cause – like a tiny tear – has healed. If the hemorrhage is dense, blocks the macula, or is linked to active diabetic vessels, we usually intervene with anti‑VEGF injections or a vitrectomy to speed recovery and protect vision.
What are the treatment options and how long is recovery?
We start with the least invasive approach. Observation works for tiny, stable bleeds. Anti‑VEGF injections shrink new vessels and clear blood over a few weeks. Laser photocoagulation seals retinal tears in the same visit. When the blood won’t move, pars plana vitrectomy removes it surgically; recovery typically involves two weeks of limited activity and full visual recovery by six weeks. Post‑op eye drops and head‑elevation help the eye heal.
How can I lower my risk of another bleed?
Control diabetes tightly (HbA1c < 7 %), keep blood pressure around 120/80 mmHg, and discuss any anticoagulant adjustments with your cardiologist before high‑impact activities. Wear protective eyewear during sports or DIY projects, and avoid heavy lifting or straining until you’ve had a clean bill of health. Regular six‑month retinal checks are a simple way to catch early changes before they turn into bleeding.
What should I bring to my first retina appointment?
Write down when the symptoms started, what you saw (floaters, curtain, flashes), any recent eye trauma, and a list of medications—including blood‑thinners. Bring recent blood‑test results if you have diabetes or hypertension. This checklist lets the specialist focus on the exam and speeds up decision‑making about imaging or treatment, giving you a clearer path to recovery.






Comments