Understanding Epiretinal Membrane Symptoms: A Practical Guide
- Dr Rahul Dubey
- Nov 23, 2025
- 17 min read
Imagine you’re reading a book and suddenly the words start to blur right in the middle of a sentence – that unsettling feeling is a lot like what many people experience when epiretinal membrane symptoms begin. You might notice a slight distortion in straight lines, like a crooked grid on a road sign, or find that colors look a bit washed out, especially when you look at a bright sky.
One of my patients, a 62‑year‑old avid gardener, first thought his vision was just “getting old” because she kept misreading the labels on her seed packets. Over weeks, the distortion worsened; she described it as “seeing the world through a frosted window.” That’s a classic sign of an epiretinal membrane pulling on the macula and warping your central vision.
Another real‑world scenario: a 48‑year‑old graphic designer noticed that fine details in her work became fuzzy, and reading the smallest print felt like straining through a smudge. She also reported occasional floaters that seemed to drift across her field of view. Both examples share two key symptoms – blurred or distorted central vision and the presence of floaters.
So, how do you know when it’s time to act? Start with a quick self‑check:
Can you read a newspaper headline without squinting?
Do straight lines appear wavy or bent?
Are you seeing new or worsening floaters?
If you answer “yes” to any of these, schedule an eye exam. An ophthalmologist will use optical coherence tomography (OCT) to see the thin scar tissue on the macula. Early detection often means you can monitor the membrane and avoid surgery until vision loss becomes significant.
While you’re waiting for your appointment, try these three actionable steps:
Keep a daily vision diary – note any changes in clarity, distortion, or floaters.
Reduce eye strain by using proper lighting and taking the 20‑20‑20 break (every 20 minutes, look at something 20 feet away for 20 seconds).
Maintain a healthy diet rich in omega‑3 fatty acids, which supports overall retinal health.
Understanding the warning signs empowers you to seek care before the membrane progresses. For a deeper dive into what an epiretinal membrane is and how it’s treated, check out Epiretinal Membrane information on Dr. Rahul Dubey’s site. And if you’re a small business owner looking to support your team’s eye health, you might find how to offer health insurance to employees a useful resource.
TL;DR
If you’ve noticed wavy lines, blurry central vision, or new floaters, those are classic epiretinal membrane symptoms that signal it’s time to schedule an eye exam and start tracking changes.
Meanwhile, keeping a vision diary, taking regular 20‑20‑20 breaks, and eating omega‑3‑rich foods can help you manage discomfort while you await professional care, giving you clearer insight and potentially delaying surgery.
What Are Epiretinal Membrane Symptoms?
Ever glance at a street sign and feel like the letters are dancing? That fleeting, unsettling wobble is often the first clue that an epiretinal membrane is tugging at your macula. You might think it’s just eye‑strain, but the brain picks up on that subtle distortion before you do.
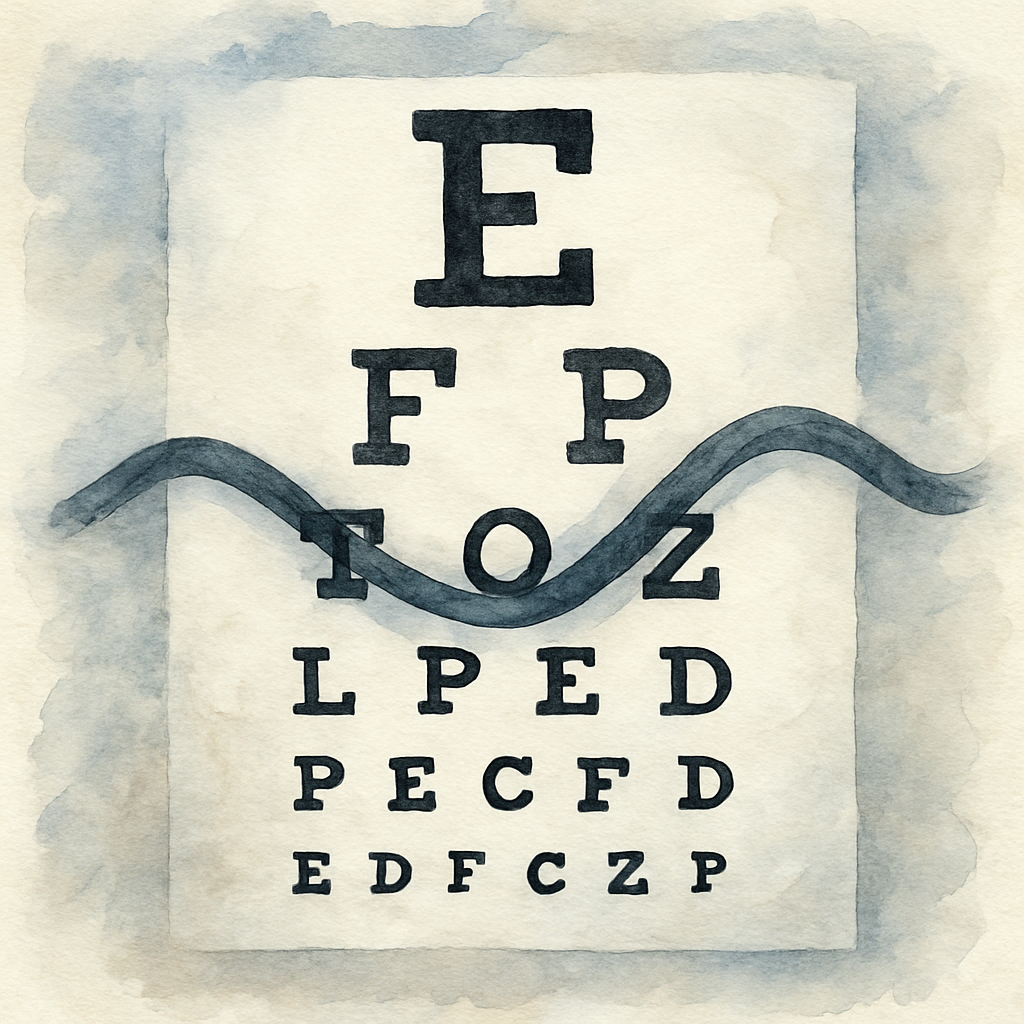
One of the most common complaints is a waviness in straight lines – a road divider that looks like a gentle wave, or a computer monitor grid that seems to ripple. This happens because the thin scar tissue on the surface of the macula pulls on the retinal layers, literally bending how light is focused. You may also notice colors looking a shade duller, especially against a bright sky or a white wall.
Floaters and Dark Spots
Floaters often get lumped in with cataracts, but in the context of an epiretinal membrane they can be a warning sign. Small specks that drift across your vision, or a shadow that seems to follow a moving object, may indicate that the membrane is interacting with the vitreous humor. It’s not always painful, but the sensation of something “floating” can be unnerving.
Blurred Central Vision
When the membrane thickens, the central part of your sight – the area you use to read, recognize faces, or thread a needle – can become hazy. You might find yourself holding a newspaper farther away just to make out the headline, or you might need to squint more often. This isn’t the peripheral blur you get from a cataract; it’s a focused loss right in the middle of your view.
So, how do you know when it’s time to act? Here’s a quick self‑check:
Do straight lines appear wavy or bent?
Are colors looking washed out, especially in bright light?
Are new floaters or shadows appearing in your field of vision?
If you answered “yes” to any of those, schedule an eye exam. An ophthalmologist will likely run an optical coherence tomography (OCT) scan to visualize the membrane’s thickness and decide whether monitoring or surgery is needed.
Want a deeper dive into what the membrane actually looks like and how it’s treated? Check out Epiretinal Membrane | Dr Rahul Dubey for a concise overview.
While you wait for your appointment, keep a vision diary – note the time of day, lighting conditions, and any new distortions. This record helps your doctor see patterns that might otherwise slip by.
Beyond the eye‑specific steps, there are broader tools that can ease the stress of managing a health condition. For businesses looking to streamline operations and free up time for personal health, Assistaix - AI Business Automation That Works offers solutions that automate routine tasks, giving you more breathing room for doctor visits and self‑care.
If you’re a small‑business owner wondering how to support your team’s eye health through benefits, How to Offer Health Insurance to Employees: A Step‑by‑Step Guide for Small Businesses provides a clear roadmap to adding vision coverage that can catch issues like epiretinal membranes early.
Remember, the symptoms often start subtle. By staying observant, keeping a simple diary, and acting promptly, you can often delay or avoid surgery altogether. Your eyes are the windows to the world – treat them with the same care you’d give a favorite pair of glasses.
How Symptoms Progress Over Time
When you first notice a wavy line on your Amsler grid, it can feel like a minor annoyance. But a few weeks later, that same line might look like a ripple on a pond – subtle, yet unmistakable. That shift is the hallmark of epiretinal membrane symptoms evolving as the scar tissue tightens and pulls on the macula.
Imagine you’re watching a movie and the picture starts to blur just around the main character’s face. At first you think it’s the seat, then you realize the screen is actually dimming in that spot. In the eye, the membrane behaves the same way: it begins as a thin, almost invisible layer, then gradually contracts, distorting the central vision you rely on for reading, driving, or recognizing faces.
Early Phase: Flickers and Floaters
In the first few months, many patients report new floaters or brief flashes of light. Those are often the first clues that the vitreous has shifted enough to let glial cells migrate and form a membrane. At this stage, visual acuity may still be 20/20, but you might notice a slight “ghost” effect when looking at a bright sky or a white wall.
Take Maya, a 45‑year‑old teacher. She thought the specks were dust until she tried the Amsler grid and saw a faint distortion. Her ophthalmologist ordered an OCT, which showed a thin membrane that wasn’t yet tugging on the fovea. Maya’s symptom timeline illustrates why early monitoring matters.
Mid‑Stage: Metamorphopsia Takes Hold
As months turn into a year, the membrane often becomes more contractile. Straight lines start to bend, and reading a newspaper headline feels like trying to decipher a wave‑washed billboard. The distortion may be intermittent at first – you see it on one eye, then the other – but it soon becomes a constant background hum.
John, a 60‑year‑old carpenter, described the moment like this: “I was sanding a piece of wood and the straight grain looked like it was dancing. I stopped, rubbed my eyes, and it was still there.” An OCT confirmed that the membrane thickness had increased, pulling the retinal layers together. For John, the progression from occasional floaters to daily metamorphopsia happened over roughly eight months.
Advanced Phase: Declining Visual Acuity
When the membrane reaches a critical tension, central visual acuity drops. You may need to hold a phone closer, or you might find that facial expressions become harder to read. Studies show that about 20% of epiretinal membranes progress to the point of needing surgery within five years, but many patients stay stable for much longer if the change is caught early.
Sarah, a 70‑year‑old retiree, waited three years before seeing her surgeon because her vision was still functional. When she finally sought care, the membrane had caused a small macular puckering that reduced her best‑corrected vision to 20/40. She now plans a membrane‑peeling vitrectomy, which Dr. Dubey explains can restore up to two lines of vision in most cases.
Actionable Steps to Track Progress
1.Update your vision diary weekly.Note any new wobble, change in reading distance, or increase in floaters. A simple table with date, eye, and description works wonders.
2.Re‑test with the Amsler grid every two weeks.Compare the pattern you draw today with the one from last month. Even a tiny shift matters.
3.Schedule a follow‑up OCT every 3–6 monthsif your doctor recommends monitoring. The scan will show you exactly how thick the membrane is becoming.
4.Watch your systemic health.High blood pressure and cholesterol can accelerate membrane formation. Keep your diet heart‑healthy and stay active.
5.Know when to call your retina specialist.If you notice a sudden increase in distortion, flashes of light, or a drop in reading clarity, book an appointment immediately.
And remember, you don’t have to navigate this alone. Our Vitreous Floaters | Dr Rahul Dubey page explains how floaters often signal the early stages of membrane development and offers tips on when to seek care.
For a broader perspective on eye‑health wellness, you might find the resources at e7D‑Wellness helpful – they focus on clinician wellbeing, which is essential when you’re managing a chronic eye condition.
Video: Recognizing Epiretinal Membrane Symptoms in a Clinical Exam
When you sit in the exam chair, the first thing the doctor does is look for the subtle clues that whisper, “I’ve got an epiretinal membrane.” It’s not always a dramatic flare‑up; often it’s a quiet tug on the macula that shows up as a tiny distortion on your Amsler grid.
So, what should you actually be watching for? Think about the classic signs: wavy lines that should be straight, a faint “ghost” floaters drifting across a bright sky, and that odd sensation that the center of your vision feels a little off‑kilter, like you’re peering through frosted glass.
Step 1: The Visual Inspection
The doctor starts with a lamp and a simple handheld lens. They’ll ask you to focus on a single point while they shine a light across your retina. If the membrane is pulling, you might notice a slight shimmer or a tiny retinal fold that looks like a microscopic ripple.
During this part of the exam, they’ll also check the foveal avascular zone (FAZ). A reduced FAZ size can hint at traction. Recent OCT research shows that deeper retinal folds (measured as MDRF) line up with the severity of aniseikonia, a distortion of image size that patients actually feel.
Step 2: The OCT Scan
Next comes the optical coherence tomography (OCT). This isn’t a fancy term for a “high‑tech selfie”; it’s a cross‑sectional image of your retina that lets the doctor see the membrane’s thickness, the depth of any folds, and how the inner nuclear layer (INL) is swelling.
Look for numbers in the report: a maximum depth of retinal fold (MDRF) above 70 µm often correlates with the point where patients start noticing real trouble with binocular vision. If your scan shows a deeper fold, your surgeon may suggest early intervention before the aniseikonia reaches that 3 % threshold that messes with daily activities.
Step 3: The Functional Tests
Beyond imaging, you’ll likely do an Amsler grid test right there in the office. Cover one eye, stare at the central dot, and note any wavy lines. Then switch eyes. The doctor might also use a M‑CHARTS card to quantify metamorphopsia – the technical name for that “wiggly” vision.
These functional tests help translate the OCT numbers into what you actually experience. If the grid looks distorted and the OCT shows a thickened INL, that combination is a strong hint that the membrane is actively pulling on the macula.
Step 4: Putting It All Together
At this point, the doctor will discuss what the findings mean for you. If the traction is mild and your vision is still sharp, they may recommend watchful waiting with regular Amsler checks. If the MDRF is edging toward 90 µm or your aniseikonia is creeping past 3 %, they’ll likely talk about membrane peeling surgery.
Remember, you’re not alone in this decision. Our Cataract | Dr Rahul Dubey page explains how we approach related retinal conditions and why timing matters for preserving quality of vision.
Here’s the video that walks you through what the clinician actually sees on the screen. Pay attention to the highlighted retinal folds and the way the doctor points out subtle changes in the FAZ.
After watching, you’ll have a clearer picture of what “epiretinal membrane symptoms” look like under the microscope. The next step is simple: schedule that follow‑up, bring your vision diary, and ask your retina specialist to show you the OCT slices. Seeing the membrane in real time helps you understand why those wavy lines matter and gives you confidence in the treatment plan.
Bottom line: the clinical exam is a layered process—visual inspection, OCT imaging, functional testing—all aimed at catching the membrane before it steals your visual comfort. Stay proactive, keep tracking changes, and don’t hesitate to ask the doctor to explain any number or image you don’t get. Your eyes deserve that level of care.
Comparing Symptom Severity: Mild vs. Moderate vs. Severe
When you first notice something off in your vision, it can be hard to tell whether it’s a fleeting annoyance or the start of a real problem. That’s why understanding how epiretinal membrane symptoms scale from mild to severe matters.
In the mild zone, the changes are almost whisper‑quiet. You might catch a single wavy line on an Amsler grid or need to squint a little more when reading a headline. Vision acuity often stays at 20/20, so you can still drive, work, and scroll your phone without thinking twice.
But have you ever felt that those subtle distortions start to creep into daily tasks? That’s the jump to moderate severity. The metamorphopsia becomes noticeable on more than one line, straight edges look bent in multiple places, and you may need to hold reading material closer. Floaters can become more numerous, and you might notice occasional flashes.
Now imagine the world turning a little more fuzzy every morning – that’s the severe end. Central visual acuity drops below 20/40, straight lines warp dramatically, and reading becomes a chore. You may see a “shadow” over the center of your vision, and everyday activities like recognizing faces or reading street signs feel compromised.
How to tell where you are on the spectrum
Ask yourself these quick checks:
Do you need extra lighting or a closer view for small print? (Mild)
Are multiple lines on an Amsler grid wavy, and do floaters bother you more than before? (Moderate)
Has your best‑corrected vision declined noticeably, or do you see a central dark spot? (Severe)
These questions help you map your experience to the three tiers, and they also give your retina specialist a clear picture of what to look for on OCT scans.
What the science says
A 2016 review of epiretinal membrane research notes that symptom severity often correlates with central foveal thickness measured on OCT, with thicker membranes driving more pronounced metamorphopsia and visual loss according to the Dove Press study . In other words, the more the membrane contracts, the harsher the symptoms.
Why the difference matters for treatment
If you’re in the mild stage, most doctors recommend watchful waiting. Regular Amsler checks and a quarterly OCT keep the membrane in view while you maintain your routine.
At moderate severity, you and your doctor might start discussing early intervention options—perhaps a pars plana vitrectomy with membrane peeling—especially if the distortion begins to affect work or hobbies.
When severe symptoms appear, surgery becomes a stronger consideration because the risk of permanent photoreceptor damage rises. The goal shifts from preserving vision to restoring as much function as possible.
For a concise rundown of what each level looks like, see the table below.
Severity | Typical Signs | Recommended Action |
Mild | Occasional wavy line on Amsler, 20/20 acuity, few floaters | Monitor with Amsler, OCT every 6‑12 months |
Moderate | Multiple distorted lines, need to hold reading material closer, increased floaters, acuity 20/30‑20/40 | Discuss early vitrectomy, increase OCT frequency (3‑6 months) |
Severe | Significant metamorphopsia, central dark spot, acuity ≤20/40, frequent flashes | Plan surgery promptly, consider retinal specialist referral |
Remember, you don’t have to navigate this alone. Our About | Dr Rahul Dubey page explains the expertise behind the retina team and how we tailor treatment plans to each severity level.
So, where do you think you fall? Take a moment to run through the checklist, note any changes in your vision diary, and book that follow‑up if the signs point toward moderate or severe. Early action can mean the difference between a quick recovery and a long‑term visual handicap.
When to Seek Treatment: Red Flags and Medical Advice
You've probably gotten good at spotting the early wavy‑line warning signs, but there comes a point when you need to stop monitoring and start calling your eye doctor. The difference between a “just keep an eye on it” and a “let's get this fixed” can be subtle, yet it matters a lot for preserving the fine detail you need for reading, driving, or simply enjoying a sunset.
Red‑Flag Symptoms That Can’t Wait
These are the clues that signal the membrane is tightening or that something else is brewing behind the scenes. If any of them show up, grab your phone and schedule an appointment right away.
Sudden increase in metamorphopsia – straight lines look dramatically wavy or bent, not just a faint ripple.
New or worsening floaters accompanied by flashes of light, especially if they appear in the peripheral vision.
Noticeable drop in visual acuity (e.g., you now need to hold a book at arm’s length to read the headline).
Development of a dark spot or shadow in the center of your vision that wasn’t there before.
Any symptom that interferes with daily tasks – misreading medication labels, difficulty recognizing faces, or trouble navigating stairs.
According to the American Society of Retina Specialists, about 2 % of people over 50 and up to 20 % over 75 have an epiretinal membrane, but only a fraction progress to these red‑flag stages Medical News Today explains . That means most of us won’t need surgery, but those who do should catch the warning signs early.
When to Call Your Retina Specialist
Think of your retina specialist as a co‑pilot. You’re the one noticing the turbulence; they have the instruments to navigate it.
Here’s a quick decision tree you can use the next time something feels off:
Run the Amsler grid. If the grid looks distorted in more than one area, note the pattern.
Check your vision diary. Has the distortion been getting bigger over the past week?
If you answered “yes” to either, call the office within 48 hours. Mention the specific red‑flag symptom (e.g., “I’m seeing new flashes and a central dark spot”).
During the call, ask whether they want you to come in for an urgent OCT scan. That quick, non‑invasive scan lets the doctor see the exact thickness of the membrane and decide if surgery should be scheduled.
Real‑World Examples
Take Maya, a 45‑year‑old teacher. She thought a sudden surge of floaters was just “dust in the eye” until she started seeing brief flashes while reading. The next day she did an Amsler test, saw a new wavy line, and called her retina clinic. An OCT showed the membrane had thickened from 70 µm to 95 µm in just a few weeks – a clear sign that intervention was needed.
John, a 60‑year‑old carpenter, ignored a gradual “blurriness” for months because he could still finish his work. When the blur turned into a dark patch that covered half a newspaper column, he finally booked an appointment. The surgeon explained that waiting longer would have made the surgery more complex and reduced the chance of regaining his previous 20/30 vision.
Actionable Checklist You Can Use Tonight
Print this out or keep it on your phone. When you notice any change, run through the steps – it only takes a minute, but it could save months of vision loss.
Mark the date and time of the new symptom.
Perform an Amsler grid test – draw any distortion.
Record how many floaters or flashes you see.
Rate how much the change affects a daily task (1 = none, 5 = can't do it).
Call your retina specialist if the rating is 3 or higher, or if the Amsler grid shows new wavy lines.
While you wait for your appointment, keep protecting your eyes: use good lighting, follow the 20‑20‑20 rule, and maintain a heart‑healthy diet rich in omega‑3s. These habits don’t reverse a membrane, but they reduce additional stress on the retina.
Dr. Rahul Dubey often reminds patients that early surgery “can restore up to two lines of visual acuity in most cases,” but the key is acting before the membrane causes permanent photoreceptor damage.
Bottom line: you know your own vision better than anyone else. If any of the red‑flag symptoms pop up, trust your gut, document it, and get that OCT scan. Prompt action is the simplest way to keep your world sharp.
FAQ
What are the earliest epiretinal membrane symptoms I should notice?
Most people first spot a subtle distortion when they look at straight lines – a newspaper headline might look a little wavy, or a window blind seems bent. You may also notice a few new floaters drifting across a bright sky, but your overall clarity stays at 20/20. These clues are often the only warning before the membrane starts pulling on the macula.
How can I tell if my floaters are related to an epiretinal membrane?
Floaters are common, but when they appear alongside flashes of light or a new sense of “ghosting” in the center of your vision, they can signal that the vitreous has shifted enough to let scar tissue form. If the floaters become more numerous or you start seeing a faint shadow where you used to see sharp detail, it’s time to run an Amsler grid test and call your retina specialist.
When should I start using an Amsler grid, and how often is enough?
Begin the grid as soon as you notice any metamorphopsia – that wavy‑line feeling. Test one eye at a time, 14 inches away, and sketch any distortion. Do it once a day for the first two weeks; if the pattern stays stable, drop to every other day. If you see new wavy lines or the distortion spreads, schedule an urgent OCT scan.
What does a sudden increase in metamorphopsia mean for my treatment options?
A rapid jump from a faint ripple to a clearly bent line usually means the membrane is tightening. At this stage, many surgeons recommend moving from watchful waiting to a discussion about vitrectomy with membrane peeling. Early surgery can often restore up to two lines of visual acuity, so catching the change quickly can make a big difference.
Can lifestyle changes slow down the progression of epiretinal membrane symptoms?
While nothing can erase the scar tissue, keeping blood pressure and cholesterol in check reduces overall retinal stress. Eating omega‑3‑rich foods, protecting your eyes from bright glare, and taking regular 20‑20‑20 breaks help maintain the health of the surrounding retina. These habits won’t reverse the membrane, but they can prevent additional damage that makes symptoms worse.
How often should I get an OCT scan if my symptoms are mild?
If your Amsler grid stays clean and you’re still seeing 20/20 vision, most doctors suggest an OCT every six to twelve months. The scan shows the exact thickness of the membrane and whether it’s starting to tug on the fovea. If the scan shows any increase in thickness or new retinal folds, you’ll likely move to a three‑to‑six‑month monitoring schedule.
What red‑flag signs mean I need to call my retina specialist right away?
Any of the following should trigger a call: a sudden surge in wavy lines on the Amsler grid, new flashes of light, a dark spot or shadow in the center of your vision, or a noticeable drop in reading distance (you now need to hold a book at arm’s length). When you notice one of these, note the date, run a quick grid test, and request an urgent OCT appointment.
Conclusion
We've walked through what epiretinal membrane symptoms feel like—from the first wavy line on an Amsler grid to the moment a dark spot creeps into the center of your view. You now know the early clues, the red‑flag signs, and the simple habits that can keep the retina from getting worse.
So, what should you do next? Grab your vision diary, run a quick Amsler test today, and note any change. If the grid looks distorted or you notice new floaters, flashes, or a shift in reading distance, schedule an OCT scan within a week. Early monitoring often lets doctors keep the membrane stable without surgery.
Remember, you don't have to guess what the doctor will say. Bring your diary, your grid sketches, and a clear list of questions to the appointment. That preparation turns a routine check‑up into a focused conversation about whether watchful waiting or an early vitrectomy is right for you.
Finally, if any of the red‑flag symptoms pop up—or if you simply want peace of mind—reach out to a retina specialist you trust. A prompt call can spare you months of uncertainty and protect the clarity of your world.
Take the first step today; your eyes will thank you tomorrow.






Comments