Retina Specialist vs Ophthalmologist: Key Differences Explained
- Dr Rahul Dubey
- Nov 22, 2025
- 20 min read
Ever stared at the eye chart and wondered whether the doctor you’re about to see is a general eye doctor or a retina specialist?
If you’ve ever felt that uneasy tug—“Am I getting the right expertise for my macular degeneration or a retinal tear?”—you’re not alone. The difference between a retina specialist and an ophthalmologist can feel like navigating a maze of medical jargon, especially when vision is on the line.
Here’s what I mean: an ophthalmologist is a medical doctor who can diagnose and treat a wide range of eye conditions, perform surgeries like cataract removal, and prescribe glasses. A retina specialist, on the other hand, is an ophthalmologist who has completed additional fellowship training focused exclusively on diseases of the retina and macula, such as diabetic eye disease, age‑related macular degeneration, and retinal detachments.
Think about it way—if your eye health were a car, an ophthalmologist handles the routine oil changes and brake checks, while a retina specialist is the mechanic you call when the engine itself starts sputtering.
Real‑world example: Mary, a 62‑year‑old Sydney resident, noticed a dark spot in the center of her vision. Her general ophthalmologist ran a quick exam, flagged a possible macular hole, and promptly referred her to a retina specialist. Within weeks, Dr Rahul Dubey performed a vitrectomy that saved her central vision. Stories like Mary’s illustrate why the right specialist matters.
So, how do you decide who to see? Ask yourself three quick questions: 1) Is the problem affecting the front of the eye (like cataracts) or the back (retina, macula)? 2) Does the condition require advanced imaging such as OCT or fluorescein angiography? 3) Have you been referred by an eye doctor for a retina‑focused evaluation?
When the answer leans toward the back of the eye, schedule a consultation with a retina specialist. In Sydney, Dr Rahul Dubey combines surgical expertise with cutting‑edge laser treatments, and you can learn more about Dr Rahul Dubey on his practice page.
And if you’re a small business owner worrying about covering these specialist visits, a quick read of this health insurance guide can show you how employee plans often include retinal surgery benefits.
Bottom line: knowing whether you need an ophthalmologist or a retina specialist empowers you to act fast, protect your vision, and avoid unnecessary appointments. Let’s dive deeper into the specific conditions each doctor treats and what to expect during a visit.
TL;DR
If your vision problem sits at the back of the eye—macular degeneration, retinal tear, or diabetic eye disease—you need a retina specialist, not just an ophthalmologist.
Choosing the right doctor speeds treatment, protects sight, and saves you from unnecessary appointments, so you can get back to seeing the world clearly.
Table of Contents
Understanding the Role of a Retina Specialist
When you hear the phrase “retina specialist vs ophthalmologist,” it can feel like a jargon‑filled duel. But the reality is simpler: a retina specialist is an ophthalmologist who has spent extra years mastering the back‑of‑the‑eye. Think of it as a chef who goes back to culinary school to perfect pastry – the basics are the same, but the expertise is laser‑focused.
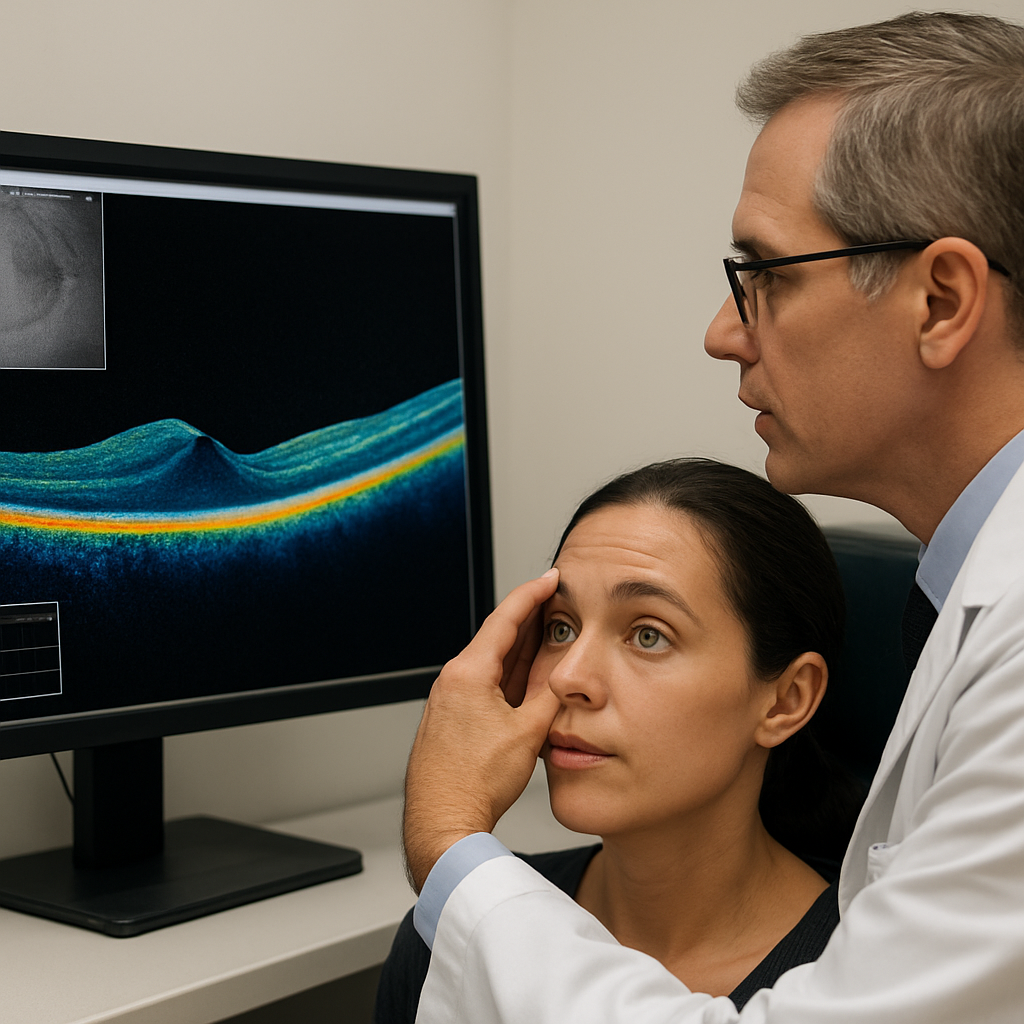
So, what does that extra training look like? After completing medical school and a general ophthalmology residency, a retina specialist adds a fellowship that dives deep into vitreoretinal medicine. They learn to interpret optical coherence tomography (OCT) scans, perform fluorescein angiography, and master delicate surgeries on tissue thinner than a butterfly’s wing. Retina Consultants of America explains that this additional education equips them to handle complex conditions like wet age‑related macular degeneration (AMD) and proliferative diabetic retinopathy.
Imagine you’re John, a 58‑year‑old accountant who suddenly notices a shadow drifting across his central vision. A general ophthalmologist can run a basic exam, but when the OCT reveals fluid under his macula, the next step is a retina specialist. Dr. Rahul Dubey, for example, would evaluate the scan, discuss intravitreal injection options, and decide whether a vitrectomy is needed. That decision‑making power comes from the subspecialty training.
Here’s a quick checklist to help you decide if you need that extra layer of expertise:
Is the problem affecting the back of the eye (blurred central vision, floaters, flashing lights)?
Do you need advanced imaging like OCT or fluorescein angiography?
Has a general eye doctor referred you for a retina‑focused evaluation?
If you answered “yes” to most of these, you’re probably looking at a retina specialist. The difference isn’t just academic – it translates to faster, more precise treatment.
What can you expect during your first visit? According to the American Society of Retina Specialists, a retina appointment often lasts two to three hours. You’ll share your full medical history, get your pupils dilated, and undergo imaging that creates a detailed map of your retinal health. The ASRS notes that this thorough approach helps catch subtle changes early, which can be the difference between preserving vision and losing it.
Real‑world example: Sarah, a 45‑year‑old teacher, was diagnosed with a retinal tear after a sudden “curtain” sensation. Her ophthalmologist booked her with a retina specialist within 24 hours. The specialist performed a laser retinopexy that sealed the tear, preventing a full‑thickness detachment. Without that rapid, specialized intervention, Sarah might have faced emergency surgery and permanent vision loss.
Now, let’s talk practical steps you can take right now:
Ask your eye doctor whether your condition involves the retina or macula.
Request an OCT scan if you haven’t already – it’s the gold‑standard imaging for retinal disease.
If a retina specialist is recommended, review their Services | Dr Rahul Dubey page to see which procedures they offer (e.g., anti‑VEGF injections, vitrectomy, laser therapy).
Schedule the appointment within two weeks; early treatment improves outcomes for conditions like wet AMD.
Bring a friend or family member for support, especially because dilation can blur your vision for several hours.
It’s also worth noting that retina specialists are often involved in cutting‑edge research and clinical trials. This means you might have access to newer therapies before they become mainstream – another advantage of choosing a subspecialist.
One lingering question many patients have is whether seeing a retina specialist means higher costs. In most Australian health schemes, specialist consultations and necessary procedures are covered, especially when a referral is provided. If you’re navigating private insurance, check whether intravitreal injections and laser treatments are listed benefits.
Finally, a quick side note for anyone juggling health and fitness: staying active can improve circulation, which is beneficial for retinal health, especially in diabetic patients. For broader wellness tips, you might explore Fitness and Wellness Starts Here | Athlemove – they offer resources that complement eye‑care regimens.
Understanding the Role of an Ophthalmologist
When you hear “retina specialist vs ophthalmologist,” it’s easy to get lost in the jargon. But at its core, an ophthalmologist is a medical doctor who can handle anything from a simple prescription to a complex eye surgery. That breadth of training is why they’re often the first line of defence when you notice a change in vision.
Think about the path to becoming an ophthalmologist: four years of undergrad, four years of medical school, then at least four more years of residency where they learn to diagnose, operate, and manage systemic diseases that affect the eye. The American Academy of Ophthalmology explains that this extensive education equips them to treat a wide range of conditions, not just the retina according to the AAO . In other words, they’re the Swiss‑army knife of eye care.
So, what does that look like in everyday practice? Imagine you’re Jane, a 55‑year‑old accountant who’s been getting occasional floaters. She books an appointment with her local eye doctor, who turns out to be an ophthalmologist. During the exam, the doctor dilates her pupils, runs an OCT scan, and spots early signs of diabetic retinopathy. Because the ophthalmologist can both interpret the scan and perform laser treatment on the spot, Jane avoids a referral delay and gets the laser therapy the same day.
Contrast that with a scenario where the first contact is an optometrist who can’t perform laser procedures. Jane would have to be sent to another clinic, wait days for an appointment, and risk disease progression. That extra step can be the difference between preserving vision and facing a more invasive surgery later.
Here’s a quick checklist to help you decide if you need the full scope of an ophthalmologist’s skills:
Are you experiencing symptoms that affect the front of the eye (cataract, glaucoma) or the back (fluid, bleed, tearing)?
Do you need advanced imaging like OCT or fluorescein angiography?
Is there a possibility you’ll need a procedure that only a medical doctor can perform, such as intra‑vitreal injections or vitrectomy?
If you answered “yes” to any of those, you’re likely better off seeing an ophthalmologist first. Their ability to both diagnose and treat means fewer appointments, faster intervention, and often better outcomes.
What can you expect during that first visit? Most ophthalmology appointments last between two to three hours. You’ll share your full medical history, undergo pupil dilation (which can blur your vision for a few hours), and sit through imaging that creates a 3‑D map of your retina. The doctor will walk you through what they see, explain any findings in plain language, and outline a treatment plan—whether that’s medication, laser, or surgery.
Real‑world example: Tom, a 68‑year‑old retiree, noticed a “shadow” in his central vision. His ophthalmologist ordered an OCT, diagnosed wet age‑related macular degeneration, and administered an anti‑VEGF injection during the same visit. The quick action slowed the disease progression and preserved his ability to read the newspaper.
Now, let’s talk actionable steps you can take today:
Schedule a comprehensive eye exam with an ophthalmologist if you have any chronic conditions like diabetes or hypertension.
Ask for an OCT scan if you notice sudden changes in central vision, floaters, or flashes.
Keep a symptom diary – note when you first saw the change, what you were doing, and any associated discomfort.
Bring a support person, especially if you’ll be dilated; they can help you get home safely.
Review the doctor’s post‑visit instructions carefully – many treatments require eye drops or activity restrictions.
If you want to dive deeper into how an ophthalmologist manages age‑related macular degeneration, check out our dedicated page on Age Related Macular Degeneration | Dr Rahul Dubey . It breaks down the diagnostic process, treatment options, and lifestyle tips you can start using right now.
Staying active while you recover can also boost circulation to the eyes. For a simple way to keep moving at home, you might explore FitCore Supply – they offer portable equipment that’s easy on the joints and fits into a busy schedule.
Training and Certification Differences
When you start comparingretina specialist vs ophthalmologist, the first thing you’ll notice is how their education paths diverge.
An ophthalmologist spends four years in medical school, then a year of internship, followed by at least three years of hospital‑based residency where they learn to diagnose, treat and surgically manage every part of the eye. Some stay in general ophthalmology, while others add another one‑to‑two‑year fellowship in a focused area like glaucoma or pediatric eye care.
Most ophthalmologists also chase board certification through the American Board of Ophthalmology, a two‑part exam that proves they’ve mastered the core knowledge. After passing, they must keep up with continuing medical education to stay certified.
A retina specialist walks the same road up to the end of residency, then chooses a vitreoretinal fellowship that lasts another one to two years. During that time they become fluent in interpreting optical coherence tomography (OCT) scans, performing fluorescein angiography, and mastering delicate surgeries on tissue thinner than a butterfly wing. This extra training is why they can do vitrectomies, laser retinopexy and intra‑vitreal injections with confidence.
According to the American Academy of Ophthalmology, the combination of residency and subspecialty fellowship equips retina specialists with the expertise to handle the most complex retinal and vitreous diseases (AAO training overview) .
What does that mean on the exam room floor? A retina specialist can read the subtle fluid pockets on an OCT, decide whether an anti‑VEGF injection is needed, and if the situation calls for it, schedule a same‑day vitrectomy. An ophthalmologist can do many of those steps, but without the fellowship they might refer you to a retina colleague for the advanced procedure.
So, why should you care about the difference?
What the certifications mean for you
Here’s a quick checklist to help you interpret the credentials you’ll see on a doctor’s profile:
Board‑certified by the American Board of Ophthalmology – a baseline guarantee of competence.
Fellowship title (e.g., “Vitreoretinal Fellow” or “Retina Specialist”) – signals additional, focused training.
Procedural privileges listed (vitrectomy, laser retinopexy, intravitreal injections) – shows they can perform the specific treatment you need.
If you spot a retina‑focused fellowship, you’re likely looking at a clinician who handles conditions like epiretinal membranes, macular holes and proliferative diabetic retinopathy on a daily basis. For example, our Epiretinal membrane treatments page showcases how a retina specialist manages that specific disorder.
Below is a short video that walks you through a typical retinal consultation, from dilation to imaging and treatment planning.
Notice how the doctor explains each scan in plain language and then outlines the next step. That level of communication usually comes from someone who has spent extra months—or years—perfecting those skills.
When you’re deciding who to book, ask two simple questions: Does the doctor list a vitreoretinal fellowship? Are they board‑certified? If the answer is yes, you’ve likely found the right specialist for complex back‑of‑the‑eye issues.
Actionable tip: before you click “schedule,” pull up the clinician’s profile, look for the fellowship line, and confirm they perform the specific procedure you need (e.g., vitrectomy, laser). If anything feels unclear, give the office a quick call and ask, “Do you have a retina‑trained surgeon on staff for my condition?” That small step can shave weeks off your treatment timeline.
When to See a Retina Specialist vs an Ophthalmologist
Spot the red flags early
Ever notice a sudden flash of light in the corner of your eye, or a tiny dark spot that seems to grow each day? Those are the kinds of signals that usually mean something’s happening at the back of the eye, where the retina lives.
If you’ve also been dealing with persistent floaters, blurred central vision, or a “curtain” sensation, it’s time to ask yourself: am I looking at a problem that needs a retina‑focused mind?
What the retina specialist brings to the table
A retina specialist is an ophthalmologist who has added a fellowship‑level deep dive into the vitreous and retina. That extra training translates into mastery of OCT imaging, fluorescein angiography, and microsurgical techniques that are simply not part of a general ophthalmologist’s daily toolkit.
For example, imagine you’re Jane, a 57‑year‑old teacher who suddenly sees a shadow drifting across her reading material. An OCT reveals fluid under her macula. A retina specialist can interpret that fluid, decide whether an anti‑VEGF injection is needed, and schedule a same‑day vitrectomy if the situation calls for it. That rapid, precise decision‑making is backed by data: a study cited by Austin Retina shows retina‑focused care reduces the time to treatment for wet AMD by up to 30%.
When an ophthalmologist is the right first stop
Ophthalmologists are the front‑line doctors who can diagnose, treat, and perform surgery for everything from cataracts to glaucoma. If your symptoms are limited to the front of the eye—like blurry vision that improves with glasses, eye redness, or mild dry‑eye irritation—an ophthalmologist will usually handle it without needing a referral.
But even ophthalmologists know their limits. When they spot signs of retinal disease during a routine exam, they’ll refer you to a retina specialist. The Associated Retina Consultants guide explains that common referral triggers include retinal tears, proliferative diabetic retinopathy, and macular holes.
Real‑world decision tree
Let’s walk through a few everyday scenarios so you can see where the line is drawn.
Scenario A – Flashes and Floaters:You notice flashes of light after a weekend bike ride and a few new floaters. These are classic vitreous traction signs.Action:Call your eye doctor and ask for an OCT; if fluid or a tear is detected, schedule a retina specialist within 48 hours.
Scenario B – Gradual Blur in One Eye:Your vision slowly becomes hazy, especially when reading. No pain, no flashes. This could be early cataract or early macular edema.Action:Book an ophthalmology appointment first. If the exam shows macular changes, ask for a referral to a retina specialist.
Scenario C – Sudden Vision Loss:You wake up with a “black curtain” over half of your visual field. This is an emergency retinal detachment.Action:Seek urgent care and request to be seen by a retina surgeon immediately—time is vision.
Check‑list before you pick up the phone
Identify the symptom location: front (lens, cornea) vs back (retina, vitreous).
Ask if advanced imaging (OCT, angiography) is needed.
Verify the doctor’s credentials: board‑certified ophthalmologist with a vitreoretinal fellowship for back‑of‑the‑eye issues.
Look at the clinic’s service list to confirm they perform the specific procedure you might need—laser retinopexy, vitrectomy, or intravitreal injection.
Schedule the appointment within two weeks; early intervention improves outcomes for most retinal diseases.
And here’s a quick tip that often gets overlooked: bring a friend or family member. After dilation, your vision will be blurry for several hours, and having a buddy can help you get home safely.
Quick reference table
Condition | Typical Provider | Key Treatment(s) | When to See |
Retinal tear / detachment | Retina specialist | Laser retinopexy, vitrectomy | Sudden “curtain” vision, flashes, floaters |
Wet age‑related macular degeneration | Retina specialist | Anti‑VEGF injections, photodynamic therapy | Rapid central vision loss, distortion |
Cataract | Ophthalmologist | Phacoemulsification, lens replacement | Gradual clouding, glare, difficulty reading |
Putting it all together
Think of the eye like a house. An ophthalmologist is the general contractor who can fix the roof, replace windows, and handle the plumbing. A retina specialist is the specialist you call when the foundation cracks—those are the tiny, delicate structures that hold everything together.
If you’re ever in doubt, start with your ophthalmologist. Ask plainly, “Do my symptoms involve the retina or macula?” If the answer is yes, request a referral to a retina‑trained surgeon. And don’t forget to peek at the clinic’s Macular Hole | Dr Rahul Dubey page to see which retinal procedures they specialize in.
Bottom line: catching retinal issues early and getting the right specialist on board can be the difference between preserving your sight and facing invasive surgery later. So the next time you see a flash, a float, or a shadow, use the checklist, act quickly, and you’ll be giving your eyes the best possible chance to stay clear.
Procedures and Treatments Compared
When you finally sit down with a doctor, the first thing you’ll notice is the menu of procedures on the table. The same symptom can lead to a laser spot from a retina specialist or a lens swap from an ophthalmologist. Understanding what each treatment actually does helps you decide who’s the right hand to hold.
Laser retinopexy vs cataract surgery
A retina specialist will often start with laser retinopexy if they spot a tiny retinal tear. A quick, painless laser creates tiny burns that seal the retina to the underlying tissue, stopping a detachment before it spreads. It’s an office‑based procedure that takes minutes, and you’re usually home by the end of the day.
By contrast, an ophthalmologist’s go‑to for cataracts is phacoemulsification – a tiny incision, ultrasound to break up the cloudy lens, and a clear artificial lens placed inside. That’s a surgical suite event, usually under local anaesthetic, and you’ll need a day of limited vision while the eye heals.
Anti‑VEGF injections vs lens replacement
If wet age‑related macular degeneration shows up on your OCT, a retina specialist will offer anti‑VEGF injections. These tiny drug drops into the vitreous cavity curb abnormal blood vessel growth and can stabilize—or even improve—sharpness. You’ll get a series of monthly shots, each lasting just a few minutes.
Meanwhile, an ophthalmologist might recommend lens replacement if the cataract is the primary culprit behind blurred vision. The new lens can also be chosen to reduce the need for glasses, something you can’t achieve with an injection.
Vitrectomy vs general eye surgery
When there’s significant vitreous bleeding or a macular hole, a retina specialist performs a vitrectomy. They remove the gel‑like vitreous, clean out any blood, and may place a gas bubble to flatten the retina while it heals. It’s a more involved microsurgery, but the precision comes from the extra fellowship training retina doctors receive — a point highlighted by the Elman Retina Group, which notes that retina specialists “focus on diseases and conditions related to the vitreous and retina” after a dedicated fellowship according to their overview .
General ophthalmologists can also do vitrectomies, especially if they’ve pursued additional subspecialty training, but many will refer you to a retina‑focused surgeon to ensure the latest techniques are applied.
How to match the procedure to the specialist
Here’s a quick checklist you can run through after your exam:
Is the problem at the back of the eye (fluid, tears, holes)? → Look for a retina specialist.
Do you need a lens swap or glaucoma drainage? → An ophthalmologist is the right fit.
Will the treatment involve frequent office visits (injections) or a one‑time surgery? → Ask which doctor’s clinic offers the schedule that works for you.
Remember, the same condition can sometimes be managed by both types of doctors, but the retina specialist’s deeper focus often means faster access to the newest anti‑VEGF drugs or the latest vitrectomy equipment. Advanced Eye Specialists points out that “ophthalmologists differ from optometrists and opticians in their levels of training and in what they are able to diagnose and treat” — including both medical and surgical options as described on their site .
So, what should you do next? If your doctor mentions a laser scar, a gas bubble, or a series of injections, ask whether they’re a retina‑trained surgeon. If they talk about a lens power or cataract grading, you’re likely in ophthalmology territory.
Bottom line: matching the right procedure to the right specialist isn’t just semantics—it can shave weeks off your recovery, reduce the number of visits, and give you a clearer picture of what to expect. Keep this comparison in mind the next time you’re asked to choose a doctor, and you’ll walk into the clinic knowing exactly which tool‑box you need.
Insurance, Costs, and Finding the Right Doctor
When you finally decide you need an eye specialist, the first thing that pops into most people’s heads is the price tag. It feels a bit like walking into a car dealership and hearing “$20,000” before you even sit in the driver’s seat.
So, what should you do next? First, separate the myth from the reality: most of the expensive‑looking procedures for retinal disease or cataract surgery are covered by Australia’s Medicare or private health funds—provided you have the right referral and the doctor’s billing code is listed.
Vision insurance vs. medical insurance
Vision‑only plans usually take care of routine eye exams, glasses, and contact lenses. They rarely cover laser retinopexy, anti‑VEGF injections, or vitrectomy. Those are considered medical procedures, so you’ll need to claim them under your medical insurance or Medicare. The Eye MD explains the split between vision and medical coverage , which mirrors the Australian system: the bulk of retina‑focused care falls under the medical umbrella.
Does this mean you’re stuck paying out of pocket? Not necessarily. Many private health insurers in Australia list “intra‑vitreal injections” and “laser retinal surgery” as scheduled benefits. The key is to check your policy’s “extras” list before you book.
Step‑by‑step cost‑check checklist
Confirm your GP or optometrist has given a written referral to a retina specialist or ophthalmologist.
Log into your health fund portal and search for the specific procedure code (e.g., “retinal laser” or “cataract extraction”).
Ask the clinic’s billing office for an estimate that includes the doctor’s fee, facility fee, and any anaesthetic charges.
If you have Medicare, verify whether the procedure is “bulk‑billed” or requires a co‑pay.
Keep receipts and itemised statements; they’re your ticket for claiming any out‑of‑pocket portion later.
And here’s a little secret: some retina surgeons, including Dr Rahul Dubey in Sydney, offer a “no‑gap” option for eligible Medicare patients. That means the government pays the full fee and you walk away with a zero balance. It’s worth asking the front desk about it.
Finding the right doctor without breaking the bank
When you start hunting for the right eye doctor, don’t just chase the lowest price. Think of it like choosing a mechanic: you’d rather pay a bit more for someone who knows the engine inside‑out than gamble on a cheap fix that could cost you twice as much later.
Ask these three quick questions during your first call:
Do you have a vitreoretinal fellowship (retina specialist) or are you a general ophthalmologist?
Are you bulk‑billed for Medicare‑eligible procedures, or do you offer a no‑gap arrangement?
Can you provide a transparent cost estimate before the first visit?
If the answer is “yes” to all three, you’ve likely found a provider who balances expertise with affordability.
What about location? Sydney’s public hospitals often have retina clinics that are fully covered, but wait times can stretch weeks. Private clinics move faster—sometimes within a few days—but you’ll need to confirm your insurance coverage ahead of time.
Real‑world example
Take Sarah, a 48‑year‑old teacher who noticed sudden floaters. She called her optometrist, got a referral, and asked about costs. The clinic told her the laser retinopexy would be bulk‑billed under Medicare, with a $20 co‑pay for the consumables. Because she had a “no‑gap” arrangement, the co‑pay disappeared. She walked into the clinic the next day, got the laser treatment, and avoided a retinal detachment. A simple cost check saved her both vision and money.
That story underscores a simple truth: a few minutes of insurance homework can shave weeks off your treatment timeline and keep your wallet from taking a hit.
Quick tip for the budget‑conscious
Keep a “vision health notebook” – jot down your policy number, the referral date, the doctor’s name, and the exact procedure codes you’ve been quoted. When you get the bill, compare it line‑by‑line with your notes. Discrepancies are easier to contest when you have everything written down.
Bottom line: the “retina specialist vs ophthalmologist” decision isn’t just about medical expertise; it’s also about navigating insurance pathways, understanding what’s covered, and choosing a doctor who makes the paperwork as painless as the procedure itself. Take a few minutes now to run through the checklist, ask the right questions, and you’ll walk into your appointment feeling confident—not confused.
FAQ
What’s the real difference between a retina specialist and an ophthalmologist?
Think of an ophthalmologist as a Swiss‑army‑knife eye doctor – they can treat cataracts, glaucoma, infections and even do basic retinal work. A retina specialist is an ophthalmologist who’s taken an extra fellowship to become a microsurgeon of the back‑of‑the‑eye. That extra training means they’re comfortable with OCT‑driven diagnoses, laser retinopexy, vitrectomy and the latest anti‑VEGF injections. In short, both can see you, but the retina specialist has a deeper toolbox for complex retinal disease.
When should I see a retina specialist instead of a general ophthalmologist?
If you’re experiencing flashes, new floaters, a sudden “curtain” in your vision, or central distortion that feels like looking through a warped window, those are red‑flag signs that the problem lives at the back of the eye. In those cases, ask your ophthalmologist straight away, “Does this involve the retina or macula?” If the answer is yes, a referral to a retina specialist will get you the advanced imaging and targeted treatment you need without unnecessary delays.
Can an ophthalmologist perform the same retinal procedures as a retina specialist?
Many ophthalmologists can do basic laser treatments and even give anti‑VEGF injections, especially if they’ve pursued extra training. However, the most delicate surgeries – like vitrectomy for a macular hole or complex retinal detachments – are usually reserved for retina specialists who have spent a year or two mastering those microsurgical techniques. If your doctor mentions a “vitrectomy” or a “gas bubble” for healing, double‑check that they list a vitreoretinal fellowship in their credentials.
Do retina specialists cost more than general ophthalmologists?
In Australia’s Medicare system, both types of doctors bill the same schedule when you have a valid referral, so the base fee is often identical. The difference shows up in the procedure codes: laser retinopexy, vitrectomy and anti‑VEGF injections are covered as medical services, not vision‑only benefits. If you have a “no‑gap” arrangement, the out‑of‑pocket cost can disappear completely, just like the story of Sarah who walked in for a bulk‑billed laser treatment and saved both sight and money.
How long does it usually take to get an appointment with a retina specialist?
Public hospital retina clinics can have wait times of several weeks, especially for non‑emergency cases. Private retina specialists often schedule a consultation within 7‑10 days if you bring a clear referral and any relevant OCT images. The key is to have your paperwork ready – policy number, referral date, and the exact procedure you’re being considered for – so the clinic can slot you in quickly and avoid unnecessary admin delays.
What should I bring to my first retina specialist visit?
Pack a small notebook (or use your phone) and write down your symptoms, when they started, and any recent eye‑related events like a bike fall or sudden flashes. Bring your referral, any recent test results (especially OCT scans), and a list of medications you’re on. Because dilation will blur your vision for a few hours, bring sunglasses and a friend to drive you home – that little extra prep makes the whole experience smoother.
Is there anything I can do at home while waiting for my specialist appointment?
Yes – keep a symptom diary. Note the frequency of flashes, the size of any floaters, and any changes in vision clarity. Stay hydrated, manage blood‑sugar if you’re diabetic, and avoid heavy lifting that can increase vitreous traction. Gentle eye‑friendly activities like walking or light stretching improve circulation without stressing the eye, and the diary will give your doctor a clear picture of how fast things are progressing.
Conclusion
So, after wandering through the maze of eye‑care options, what should you walk away with?
You now know that the main difference between a retina specialist and an ophthalmologist is depth of training and the types of procedures they perform.
If your symptoms sit at the back of the eye – flashes, new floaters, or a sudden shadow – a retina‑focused doctor will likely get you the OCT scan and any injection or laser you need in the fastest possible window.
When the problem is more front‑focused – cataract blur, glaucoma pressure, or routine vision checks – an ophthalmologist can diagnose, treat, and often handle surgery without a second referral.
A quick way to decide is to ask yourself two questions: Is the issue centered on the retina or macula? And does the treatment plan mention OCT‑driven decisions, anti‑VEGF shots, or vitrectomy?
Whatever path you choose, keep a symptom diary, bring your referral and insurance details, and don’t hesitate to ask the clinic about bulk‑billing or no‑gap options – that’s how you protect both your sight and your wallet.
Ready to take the next step? Book your comprehensive eye exam, ask if the doctor has a vitreoretinal fellowship, and let the right specialist guide you back to clear vision.






Comments