Metamorphopsia Causes Explained: What Triggers This Vision Distortion
- Dr Rahul Dubey
- 11 hours ago
- 18 min read
Ever stared at a hallway and thought the walls were bending?
That unsettling distortion is called metamorphopsia, and it can turn everyday life into a visual puzzle.
If you’ve ever wondered why it happens, you’re not alone – the causes are surprisingly varied.
One of the most common metamorphopsia causes is a problem with the macula, the tiny central part of the retina that gives us sharp vision.
When a macular hole forms, the tissue actually tears, and straight lines start to look wavy.
Diabetic macular edema, a swelling that results from long‑term diabetes, pushes the retina out of shape, creating the same distortion.
Central serous retinopathy, where fluid builds up under the retina, can also make objects appear stretched or compressed.
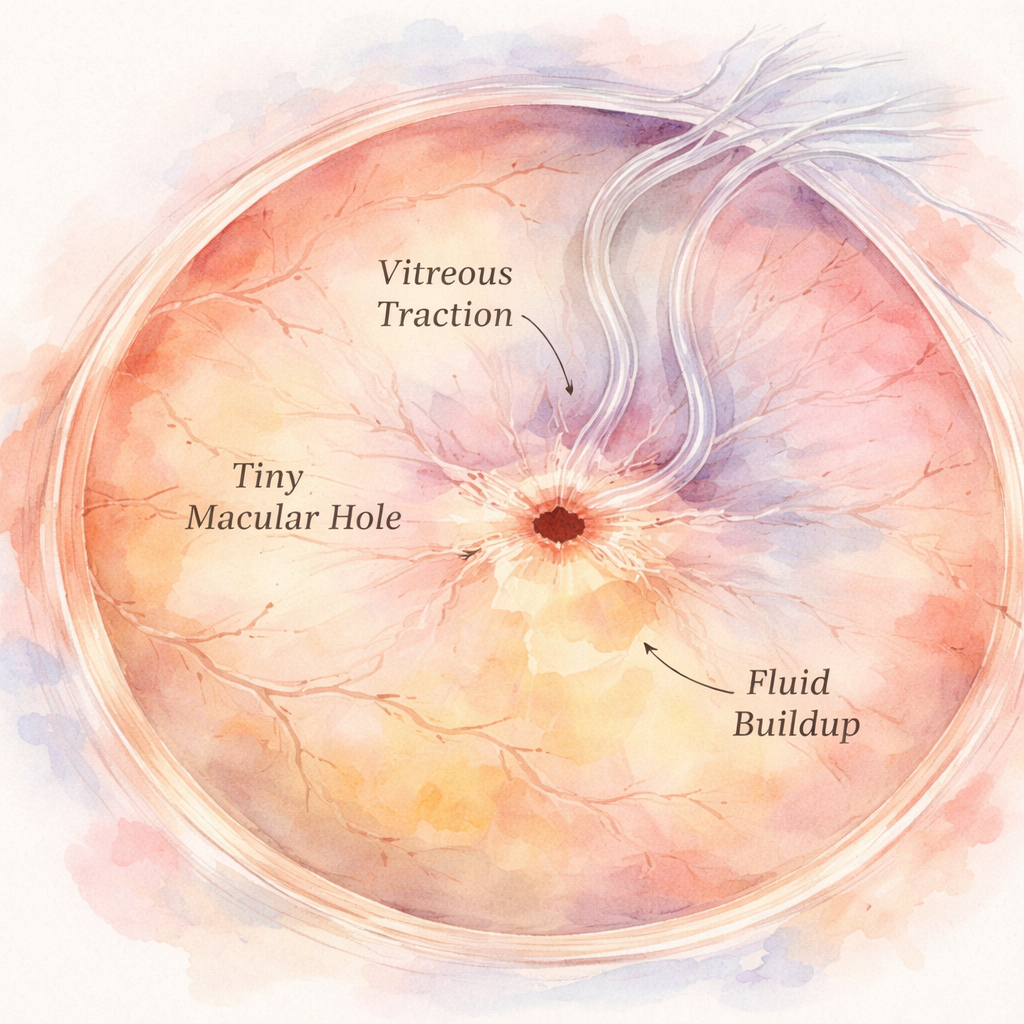
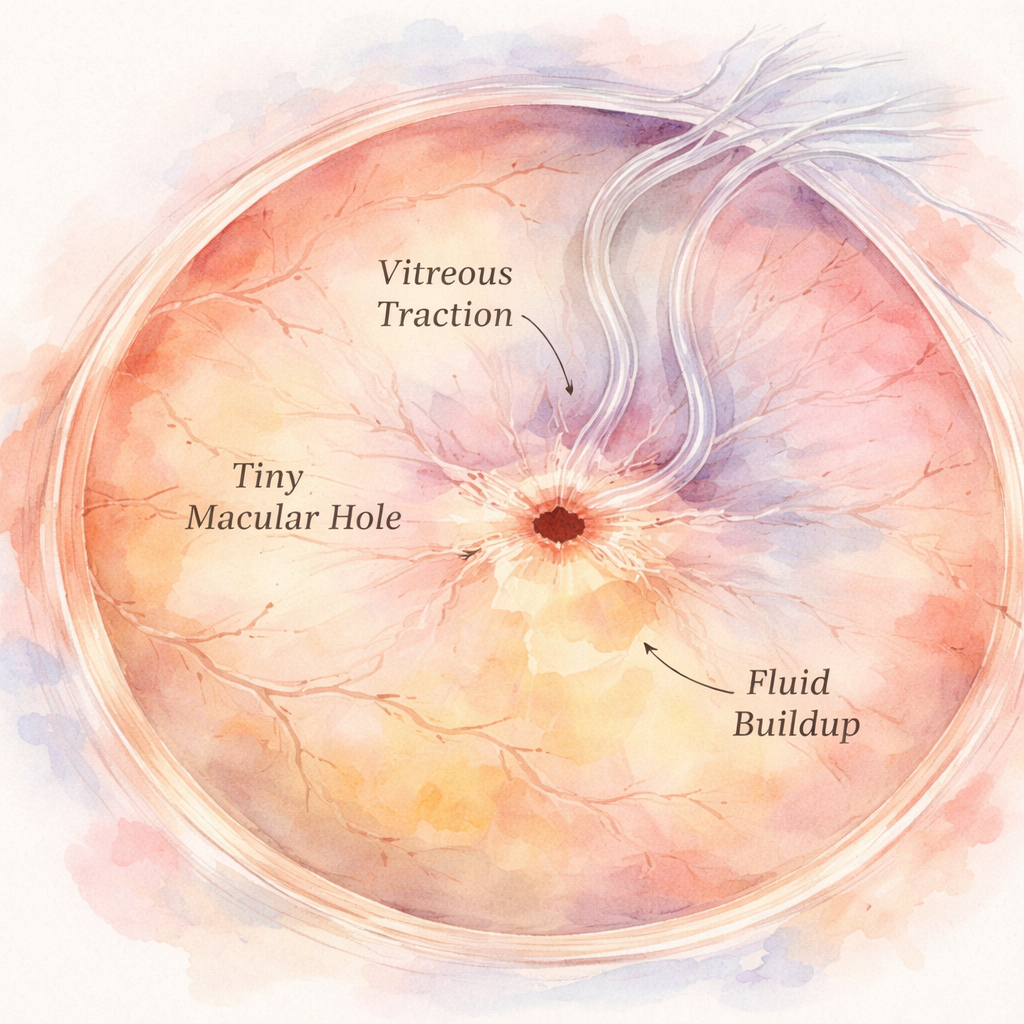
Vitreomacular traction occurs when the gel‑like vitreous pulls on the macula, tugging at the retina and producing a warped view.
Age‑related macular degeneration, retinal detachment, severe eye injury or even rare ocular tumours can all trigger metamorphopsia as they alter the retinal surface.
When you notice these changes, it’s a sign your eye needs a professional look.
At our Sydney clinic, Dr Rahul Dubey evaluates these underlying issues with advanced imaging and can recommend treatments ranging from laser therapy to minimally invasive injections.
If you’re seeing wavy lines, don’t wait – schedule an appointment, because early detection often preserves vision.
So, what should you do the next time a straight line looks crooked?
Understanding the metamorphopsia causes helps you act fast and protect your sight.
TL;DR
If you’ve ever seen straight lines wobble, the likely metamorphopsia causes range from macular holes to diabetic macular edema, and spotting them early can save your vision.
Schedule an appointment with Dr Rahul Dubey in Sydney so we can pinpoint the issue with advanced imaging and discuss the best treatment options for you.
What Is Metamorphopsia?
Ever looked at a straight line and thought it was wobbling? That unsettling feeling is what we call metamorphopsia – a distortion where straight edges appear bent, stretched or compressed. It’s not a trick of the mind; it’s your retina sending the brain a scrambled picture.
At its core, metamorphopsia is a symptom, not a disease. It tells you something’s off in the macula, the tiny central patch of retina responsible for the sharpest vision. When that area gets deformed, the brain struggles to piece together a clear image.
So, what actually causes the macula to misbehave? The list is surprisingly varied. A hole in the macula tears the tissue, leaving a literal gap that skews any line that crosses it. Fluid build‑up from diabetic macular edema pushes the retinal layers apart, creating a ripple effect. And when fluid pools under the retina – as in central serous retinopathy – it lifts the macula just enough to throw off the focus.
But it’s not just fluid. The vitreous gel that fills the eye can contract with age, pulling on the macula in a condition called vitreomacular traction. That tug feels like a tiny rope yanking at the back of your eye, warping the visual field.
We also see metamorphopsia with age‑related macular degeneration, where drusen and scar tissue change the contour of the macula. Even an epiretinal membrane – a thin sheet that grows on the retinal surface – can wrinkle the retina like a crumpled piece of paper.
When you’re dealing with any of these issues, early detection matters. In our clinic we often run OCT scans to map the retinal layers and pinpoint the exact source of distortion. If you want a deeper dive into how each cause shows up clinically, check out our guide on Metamorphopsia: Symptoms, Causes, and Treatment Options – it breaks down the anatomy in plain language.
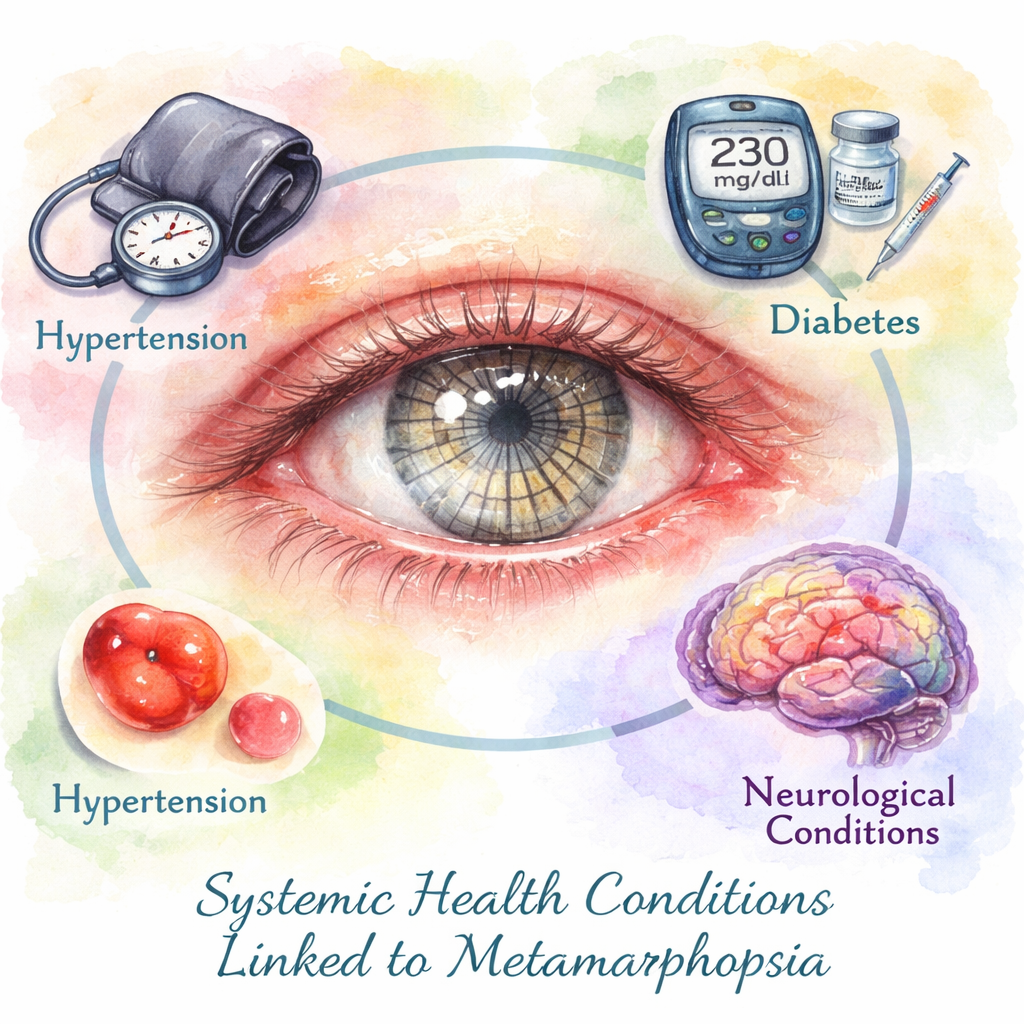
Beyond the eye, systemic health plays a big role. Uncontrolled diabetes, for example, fuels macular edema, while hypertension can aggravate retinal bleeding. That’s why a holistic approach to wellness helps protect your vision. Programs like XLR8well offer proactive health monitoring that catches blood‑sugar spikes before they damage the retina.
Seeing the video can help you visualise how different retinal layers shift during distortion. It’s one thing to read about “fluid under the retina,” another to actually watch a 3‑D model of it.
On the practice side, keeping meticulous records of these changes is crucial. A solid client‑management system ensures every scan, note and follow‑up is stored securely and accessed quickly. That’s where tools like ClientBase come in handy for ophthalmology clinics – they streamline compliance and help us focus on what matters: your eyesight.
Bottom line? Metamorphopsia is a warning light. It tells you the macula is under stress, whether from a hole, fluid, traction or age‑related wear. Recognising the symptom early, getting a proper scan, and addressing any underlying systemic issues can keep those wavy lines from becoming permanent.
Common Ocular Causes
When you first notice that straight line on a door looks like it’s wobbling, your brain is basically screaming, “something’s off in the eye.” The most frequent culprits live right on the retina, especially around the macula, and they each have their own little story.
Let’s walk through the usual suspects, sprinkle in a few real‑world snapshots, and give you clear steps to act on each.
1. Macular Hole – a literal tear in the centre of your vision
Imagine a 68‑year‑old Sydney retiree who loves knitting. One morning the stitches look stretched, as if someone’s pulling the yarn. An OCT scan shows a tiny hole in the macula. Light that should land on a smooth surface now falls into a void, creating that wavy distortion.
What you can do: book an urgent retinal review. If diagnosed early, a vitrectomy can close the hole and often restore normal vision.
2. Diabetic Macular Edema (DME) – the swelling that puffs up the macula
John, a 55‑year‑old accountant with type 2 diabetes, starts seeing the edges of his desk bending inward. Fluid leaks from damaged retinal vessels, turning the macula into a soggy sponge. The result is a funhouse‑mirror effect.
Action steps: control blood sugar, schedule regular retinal checks, and discuss anti‑VEGF injections if swelling persists.
3. Central Serous Retinopathy (CSR) – a silent leak under the retina
A young graphic designer under a tight deadline notices a blurry patch in the centre of his vision after a sleepless night. Stress‑related cortisol spikes can cause a tiny leak, lifting the macula just enough to scramble the image.
What helps: reduce stress, avoid steroids if possible, and monitor with OCT. Most cases resolve on their own, but persistent fluid may need laser treatment.
4. Vitreomacular Traction (VMT) – the vitreous gel pulling at the macula
Emma, a 62‑year‑old who enjoys gardening, feels a subtle “pull” when looking at her phone. The aging vitreous slowly contracts, tugging on the macula and causing distortion.
Steps: get a detailed scan. If the traction is significant, a vitrectomy can relieve the pull and stop the wobble.
5. Age‑Related Macular Degeneration (AMD) – the slow, progressive loss of macular cells
Mike, a 70‑year‑old retiree, begins to notice that straight lines look slightly wavy, especially in low light. Drusen deposits build up under the retina, eventually disrupting the photoreceptors.
What to do: regular AREDS‑2 supplements, lifestyle changes (stop smoking, protect eyes from UV), and in the wet form, anti‑VEGF injections.
All these conditions share a common thread: they change the shape or position of the macula, and that’s why you see the world tilt. In our clinic we rely heavily on OCT imaging to pinpoint which of these metamorphopsia causes is at play, then tailor the treatment to the specific problem.
Quick checklist you can run at home:
Grab an Amsler grid. Cover one eye, focus on the central dot. If any lines appear wavy, note which eye.
Check for accompanying symptoms: sudden flashes, new floaters, or a shadow in peripheral vision.
Write down any recent health changes – new meds, stress spikes, blood‑sugar swings.
Schedule a retinal scan within a week if anything feels off.
Below is a handy comparison of the most common ocular causes, their hallmark signs, and typical interventions.
Cause | Typical Visual Cue | Common Treatment |
Macular Hole | Straight lines look stretched; central blind spot | Vitrectomy surgery |
Diabetic Macular Edema | Wavy lines, blurred central vision | Anti‑VEGF injections, blood‑sugar control |
Central Serous Retinopathy | Localized blur, “melting” effect | Observation, focal laser if persistent |
Remember, catching these signs early gives you the full toolbox of options – from lifestyle tweaks to minimally invasive injections. If you notice any distortion, don’t wait. Your eyes are telling you something, and a prompt visit to a retina specialist in Sydney can make all the difference.
Neurological Causes
When the distortion comes from the brain rather than the retina, the story feels a bit like a glitch in the software that translates light into images. You might notice the wobble after a migraine, or you could wake up with a sideways world after a minor head bump. In those moments your eye is fine – it’s the visual‑processing centre that’s sending mixed signals.
Take Emma, a 42‑year‑old graphic designer who lives in Sydney’s inner‑west. One evening she had a classic migraine aura – flashing zig‑zags across her vision – and then the lines on her computer screen stayed slightly curved for a few hours. That lingering distortion is a classic neurological metamorphopsia. In most cases it resolves as the migraine subsides, but the episode is a useful warning sign that your brain’s visual pathways are hypersensitive.
Another scenario involves an older gentleman, Tom, who experienced a brief, painless loss of the right visual field after a mild fall. He later reported that straight edges in his left eye appeared “bent” even though his eye exam was normal. An MRI revealed a small occipital‑lobe infarct – a stroke that hit the part of the brain that stitches together the picture. Here, the metamorphopsia is a permanent clue that a vascular event has occurred.
Neurological triggers you might encounter include:
Migraine aura – affects roughly 1 in 7 Australians; can cause transient visual distortion.
Occipital‑lobe stroke – makes up about 5% of all strokes but often presents with visual‑field changes.
Multiple sclerosis lesions – demyelination in the optic radiations can scramble shape perception.
Optic neuritis – inflammation of the optic nerve, frequently linked to MS, can warp the image.
Brain tumours or cavernous malformations near the visual cortex – rare but notable for persistent metamorphopsia.
So, how do you differentiate a brain‑based cause from an ocular one? First, note the timing. If the distortion appears suddenly after a headache, stress, or head injury, think neurological. Second, check whether the distortion is the same in both eyes – a bilateral, symmetric change often points to the brain. Finally, look for accompanying symptoms: facial numbness, speech changes, or weakness could indicate a stroke.
What can you do right now? Here are three actionable steps:
Document the episode. Write down when it started, how long it lasted, and any related symptoms (headache, nausea, weakness). A clear timeline helps neurologists pinpoint the cause.
Get a neuro‑imaging referral. If the distortion persists beyond 24‑48 hours, ask your GP for an MRI of the brain. Early detection of a tiny stroke or MS plaque can dramatically improve outcomes.
Manage migraine triggers. Keep a diary of foods, stress levels, and sleep patterns. Proven strategies – regular sleep, hydration, and magnesium supplements – can cut aura frequency by up to 30% according to recent Australian health surveys.
In our clinic, we work closely with neurologists to rule out these causes. When a patient’s OCT scan looks normal but they still report metamorphopsia, we coordinate a brain MRI and, if needed, refer them for further neuro‑rehabilitation. This collaborative approach ensures we don’t miss a hidden stroke or early multiple sclerosis.
For a broader look at how visual distortion can stem from both eye and brain, you might find our overview of Causes of Visual Distortion and Wavy Vision helpful. It ties together retinal and neurological pathways in a single, easy‑to‑read guide.
If you’re already managing systemic health conditions like diabetes, consider a proactive health partner. XLR8well offers wellness programs that monitor blood‑sugar, blood‑pressure, and stress – all factors that can influence both retinal and brain health.
Bottom line: neurological metamorphopsia isn’t something to brush off. It’s your brain’s way of saying, “Hey, something’s off up there.” By logging symptoms, seeking timely imaging, and addressing underlying triggers, you give yourself the best chance of keeping the world straight‑lined.
Systemic Health Conditions Linked to Metamorphopsia
When you notice straight lines wobbling, it’s tempting to blame the eye alone. But the truth is a lot of the distortion can come from the rest of your body – especially the systems that keep your blood, nerves, and hormones in check.
Think about the last time you felt a migraine flare or had a bout of high blood pressure. Did you also see the world tilt a bit? That’s not a coincidence. Your brain and retina are wired together, so anything that throws the whole network off‑balance can show up as metamorphopsia.
Diabetes and Blood‑Sugar Swings
High glucose levels damage tiny blood vessels throughout the body, including the retina. When those vessels leak, fluid pools in the macula – that’s diabetic macular edema, a classic cause of wavy vision. Even if you’re managing diabetes well, occasional spikes can still tip the retinal surface enough to create distortion.
What you can do right now: check your blood‑sugar before you notice any visual change, log the numbers alongside an Amsler‑grid result, and bring both to your next retinal review. Early detection lets us use anti‑VEGF injections before the swelling becomes permanent.
Hypertension and Vascular Health
High blood pressure is a silent culprit. It can narrow or rupture retinal vessels, leading to retinal vein occlusion – a condition that often presents with sudden metamorphopsia. In some cases, the blockage also affects the optic nerve, compounding the visual distortion.
Action step: if you’ve been diagnosed with hypertension, keep your systolic reading under 130 mmHg. Schedule an eye exam every six months, and ask your GP to include a retinal check if you’ve had any recent spikes.
Autoimmune and Inflammatory Disorders
Conditions like lupus, sarcoidosis, or even severe allergies can cause inflammation in the retinal layers. The inflammation can mimic fluid‑related swelling, making straight lines appear curved. One case report described a child who developed prosopometamorphopsia after a Mycoplasma pneumoniae infection – an example of how systemic infection can briefly hijack visual processing.
Tip: whenever you’re treated with systemic steroids for an autoimmune flare, ask your ophthalmologist to do a quick OCT scan. Steroids can raise intra‑ocular pressure and aggravate fluid buildup.
Neurological Triggers – Stroke, MS, and Migraine
Not every distortion starts in the eye. A tiny stroke in the occipital lobe, a demyelinating plaque from multiple sclerosis, or a severe migraine aura can all scramble the brain’s visual map. The result feels exactly like a retinal problem – wavy walls, stretched letters – but the eye exam comes back clean.
When this happens, we coordinate a brain MRI and, if needed, refer you for neuro‑rehabilitation. The good news is that treating the underlying neurological issue often restores normal vision.
Kidney Disease and Fluid Balance
Chronic kidney disease can cause systemic fluid overload, which sometimes seeps into the retinal layers. Patients with late‑stage renal failure report intermittent metamorphopsia that improves after a dialysis session.
Practical advice: keep your dialysis schedule consistent, and if you notice visual distortion after a missed session, flag it to both your nephrologist and eye specialist.
Medication Side‑Effects
Some drugs – especially certain chemotherapy agents, antimalarials, and high‑dose vitamin A – can be toxic to the retina. The toxicity often presents as subtle distortion before any loss of acuity.
If you’re on any of these medications, ask your doctor for a baseline retinal scan and schedule follow‑ups every three months. Early signs are easier to treat than full‑blown damage.
All these systemic threads tie back to a single principle: your eye is a window onto the rest of your health. When something’s off in your blood, nerves, or hormones, the visual system often shouts first.
For a quick reference on how a macular hole can cause similar symptoms, check out our guide on Macular Hole: Causes, Symptoms, and Surgical Treatment . It’s a good reminder that both eye‑local and body‑wide issues can land you in the same wavy‑vision boat.
So, what should you do today? First, write down any recent health changes – new meds, blood‑pressure readings, or infections. Second, perform an Amsler‑grid test and note any distortion. Third, bring that notebook to your next appointment, whether it’s with your GP, endocrinologist, or us at the retina clinic. The more data you give us, the faster we can pinpoint the root cause and tailor a treatment plan.
Remember, tackling systemic health isn’t just about preventing heart attacks or kidney failure; it’s also about keeping your world straight‑lined.
Risk Factors and Who Is Most Affected
Ever wonder why you suddenly see a straight line wobble while driving down the Pacific Highway? It’s usually not a trick of the mind – it’s a signal that something in your eye or body is out of balance. The good news is that most of the risk factors are measurable, and many of them are things you can keep tabs on every day.
Age is the biggest headline‑grabber. As we get into our 60s and beyond, the retina naturally thins and the vitreous gel starts to contract. That tiny pull can create vitreomacular traction, which often shows up as metamorphopsia. In our clinic we see a spike in reports from retirees who’ve just swapped their morning surf for a quieter life on the North Shore.
Diabetes tops the list of systemic culprits. Even when blood‑sugar levels look decent on paper, occasional spikes can damage the tiny vessels that feed the macula. The resulting fluid‑filled swelling – diabetic macular edema – literally reshapes the retina, making straight edges look like they’re on a funhouse mirror.
Hypertension is another silent player. High pressure can cause tiny retinal vein occlusions, and those blockages often produce sudden, localized distortion. If you’ve had a recent bout of high‑blood pressure, keep an eye out for any new wavy lines and book a review within a week.
Auto‑immune and inflammatory conditions, such as lupus or sarcoidosis, can also send inflammation marching through the retinal layers. The swelling mimics fluid‑related causes, so you might notice distortion even though your eye exam looks otherwise normal.
Now, let’s talk about a less obvious but surprisingly common trigger: stress. Chronic cortisol elevation can lead to Central Serous Retinopathy (CSR) , where a tiny leak under the retina lifts the macula just enough to scramble the image. It’s the kind of thing you might experience after pulling an all‑night shift at the hospital or a deadline‑driven design sprint.
Medications matter, too. Certain steroids, antimalarials and high‑dose vitamin A can be toxic to the retina. If you’ve started a new prescription, ask your doctor for a baseline OCT scan – it’s a quick, painless way to catch early changes before they become permanent.
Neurological factors shouldn’t be overlooked. Migraine aura, especially in people who get the visual “zig‑zag” type, can cause temporary metamorphopsia. A small occipital‑lobe stroke, although rare, may produce a persistent wobble that doesn’t improve with rest. In those cases, a brain MRI is the gold‑standard follow‑up.
So, who’s most at risk? The overlap tends to look like this: people over 55, anyone with long‑standing diabetes or hypertension, individuals on systemic steroids, and those who experience frequent migraine auras. Add a family history of retinal disease, and you’ve got a perfect storm for visual distortion.
What can you do right now? First, grab an Amsler grid from your optometrist and test each eye. Note any wavy lines, then write down recent health changes – new meds, blood‑pressure readings, stress spikes. Second, schedule a retinal scan if anything feels off; our Sydney practice can run an OCT in under 15 minutes. Third, keep your systemic health in check: aim for a systolic pressure under 130 mmHg, maintain A1C below 7 %, and manage stress with regular exercise or mindfulness.
Lastly, remember that record‑keeping is a lifesaver. A simple notebook or a phone note that tracks your vision changes alongside your blood‑sugar logs gives us a clear picture of what’s happening over time. When you bring that data to your next appointment, we can pinpoint the exact cause and tailor a treatment plan – whether that means anti‑VEGF injections, a vitrectomy, or just adjusting your blood‑pressure meds.
Diagnosis and When to Seek Help
First thing’s first – you’ve just spotted a wavy line, a stretched letter or a subtle blur. Your brain is flashing a warning sign, and it’s time to treat that signal like an alarm clock.
In our clinic we start with the simplest tool: an Amsler grid. Cover one eye, stare at the central dot and note any broken or curvy lines. If something looks off, write down which eye and how severe the distortion feels. That notebook becomes your most valuable piece of evidence.
When to call the office
Don’t wait for the wobble to get worse. If you notice any of these, pick up the phone right away:
New or sudden metamorphopsia – especially after a head bump, new medication or a migraine.
Accompanying flashes, floaters or a shadow in your peripheral vision.
Distortion that’s present in both eyes, which often hints at a neurological cause.
Even if the change feels mild, an early retinal scan can make the difference between a quick fix and a longer recovery.
What the exam looks like
When you arrive, we’ll do a quick visual acuity check, then move on to optical coherence tomography (OCT). OCT gives us a cross‑sectional view of the retina in microns – think of it as an ultra‑high‑definition selfie of the macula. It spots macular holes, epiretinal membranes, fluid pockets and subtle traction that the eye‑exam alone can miss.
For many patients, the next step is a functional test. A recent study showed that a smartphone‑based hyperacuity test can reliably track metamorphopsia before and after surgery, offering a practical way to monitor progress at home (research on digital assessment tools) . While we still rely on OCT for structural detail, the app helps us gauge how your everyday vision is changing without needing an extra clinic visit.
In a handful of cases, the Amsler grid and OCT both look normal, yet the distortion persists. That’s our cue to look beyond the eye – a quick neurology referral for an MRI can rule out occipital‑lobe strokes or migraine‑related cortical spreading depression.
Quick checklist you can use at home
Grab a pen and run through these steps:
Test each eye with an Amsler grid – note any wavy lines.
Record recent health changes: new meds, blood‑pressure spikes, stress levels.
Check for extra symptoms: flashes, floaters, vision loss in part of the field.
If anything feels off, call our Sydney retina office within 48 hours.
We’ll usually fit you in for an OCT that takes under 15 minutes. The results guide us toward the right treatment – whether that’s a vitrectomy for a macular hole, anti‑VEGF injections for swelling, or simply adjusting systemic health factors.
One thing we’ve learned over the years: patients who bring a written log of their vision changes and health metrics get a faster, more precise diagnosis. It’s like giving us a map instead of a vague direction.
So, what should you do right now? Grab that grid, jot down what you see, and give us a call. The sooner we see the picture, the sooner we can straighten it out.
Remember, metamorphopsia isn’t just an odd visual glitch – it’s your eyes telling you something needs attention. Listening early gives you the full toolbox of options, from lifestyle tweaks to the latest retinal surgeries.
Conclusion
We've walked through the main metamorphopsia causes, from macular holes and diabetic swelling to stress‑related leaks and even brain‑based triggers.
The pattern is clear: whenever something reshapes or fluid‑loads the macula, the straight lines you rely on start to wobble.
That's why the simple Amsler grid test, a quick health log, and a timely OCT scan are your best first‑line defense.
If any of those wavy signs appear, call our Sydney retina office within 48 hours – we can fit you in for a 15‑minute OCT and decide whether a vitrectomy, anti‑VEGF injection, or lifestyle tweak is right.
Remember, catching the distortion early gives you the full toolbox – from laser therapy to minimally invasive macula surgery – and protects your vision for years to come.
So grab your grid, note what you see, and give us a call. We'll help you turn those wavy lines back into straight ones.
When you bring a clear log of vision changes and health metrics, we can pinpoint the exact metamorphopsia cause faster and tailor the right treatment plan for you.
Because your eyes are a window onto your overall health, staying proactive now saves you headaches – and potential sight loss – later.
Take the first step today; your future self will thank you.
FAQ
What are the most common metamorphopsia causes?
Most of the time the distortion comes from something reshaping the macula – a macular hole, diabetic macular edema, or a tiny leak that creates central serous retinopathy. Fluid‑related swelling and traction from the ageing vitreous are also big players. In our Sydney clinic we see these three categories show up over 80 % of the time. If left untreated, the lines can stay wavy permanently, making everyday tasks frustrating.
How can I tell if my metamorphopsia is eye‑related or brain‑related?
If the wavy lines appear in only one eye, it’s usually an ocular issue. When both eyes show the same distortion, or you notice accompanying headaches, nausea or weakness, think neurological. A quick check is to cover one eye with an Amsler grid; if the other eye looks fine, the problem likely lives in the eye you just covered. Write down which eye is affected and the date – it helps us pinpoint the cause faster.
When should I book an OCT scan after noticing wavy vision?
Call us within 48 hours of the first change. Early OCT imaging lets us see fluid pockets, traction or holes that a slit‑lamp exam can miss. The sooner we capture the picture, the more treatment options stay on the table – from anti‑VEGF injections to a vitrectomy. If you bring a simple log of what you saw on the Amsler grid, we can compare it directly to the scan and decide the best next step.
Can stress really cause metamorphopsia and how?
Yes. Stress spikes cortisol, which can thin the retinal pigment layer and trigger a tiny leak under the macula – the classic picture of central serous retinopathy. You’ll often notice the distortion after a late‑night project or a stressful arvo. Managing stress with regular sleep, hydration and short breaks can keep that leak from forming. Try a quick mindfulness pause each afternoon – even five minutes of breathing can lower cortisol enough to protect your retina.
Are there lifestyle changes that reduce the risk of metamorphopsia?
Keeping blood sugar steady, maintaining blood pressure below 130 mmHg, and avoiding unnecessary steroids are the biggest safeguards. Regular eye checks every six months, especially if you have diabetes or hypertension, catch fluid build‑up before it warps your vision. A simple daily Amsler grid habit adds an extra safety net. Write the date each time you test – patterns over weeks often reveal a subtle rise in fluid that you’d otherwise miss.
What treatments are available for metamorphopsia caused by a macular hole?
When a hole is small, a vitrectomy with a gas bubble can close it in a few weeks and often restores straight lines. Larger holes sometimes need a flap technique, but the success rate stays high in experienced hands. Post‑op positioning – face‑down for a few days – helps the gas press the retina back into place. We usually schedule a follow‑up OCT two weeks later to confirm the hole is sealed and the macula is flat again.
How do diabetic blood‑sugar spikes affect metamorphopsia?
High glucose damages the tiny vessels that feed the macula. Even brief spikes can leak fluid, creating diabetic macular edema that bends the retinal surface. Tracking your A1C and doing regular OCT scans when you notice any wavy lines lets us intervene early with anti‑VEGF injections or tighter sugar control. If you’re on insulin, aim for a stable pattern rather than occasional lows and highs – the retina responds best to consistency.






Comments