How to Understand and Manage Wavy Lines in Vision One Eye
- Dr Rahul Dubey
- 1 day ago
- 20 min read

Imagine you’re scrolling through your phone, and suddenly a single line on the screen looks like it’s rippling, like water on a pond – but only in your right eye. It’s a jarring moment that makes you pause, wonder if your eye is playing tricks on you.
What does it actually mean when you notice wavy lines in vision one eye? Is it just fatigue, or could it be a sign that something deeper is happening inside the eye?
Most people assume it’s harmless eye strain, yet the reality is that wavy or distorted lines often point to a change in the retina or the vitreous gel that sits behind the lens. This isn’t something you can ignore for another week.
Typical culprits include metamorphopsia – the medical term for seeing wavy or bent lines – retinal detachment, and posterior vitreous traction. Each of these conditions affects the delicate layers at the back of the eye, and they can progress quickly if left unchecked.
In our experience at our Sydney clinic, we’ve seen patients who thought it was just a temporary glitch, only to discover early‑stage retinal issues that needed prompt treatment. That’s why catching the symptom early can make the difference between a simple observation and a vision‑saving intervention.
So, what should you do right now? Start by noting when the wavy lines appear, whether they’re constant or intermittent, and if you notice any flashes, floaters, or loss of peripheral vision. These details help an eye surgeon pinpoint the cause.
Remember, you don’t have to live with uncertainty. A quick appointment with a retina specialist can clarify the picture and set you on the right path. And if it turns out to be something like vitreous traction, there are effective treatments we offer, from monitoring to minimally invasive surgery.
In the sections that follow, we’ll break down each possible cause, explain how we diagnose them, and give you clear steps to take so you can protect your sight and get back to enjoying clear, steady vision.
TL;DR
If you’ve spotted wavy lines in vision one eye, it could signal anything from harmless eye strain to early retinal trouble, so don’t just brush it off.
Write down when it happens, any flashes or floaters, and book a retina appointment with a Sydney specialist like Dr Rahul Dubey within a few days to protect your sight.
Step 1: Identify the Wavy Lines Pattern
First thing you notice when a line looks like it’s rippling only in one eye is that it feels… off. It’s that moment you stare at your phone, squint, and wonder if your brain is playing tricks. That gut feeling is the starting point for figuring out what’s really going on.
Grab a notebook or your phone’s notes app right now. Jot down the exact time you first saw the distortion, whether it was constant or came and went, and what you were doing – scrolling, reading, or maybe driving at night. These details create a pattern that your retina specialist will use to narrow down the cause.
Look for accompanying clues
Wavy lines rarely appear in isolation. Ask yourself: “Do I see floaters drifting across my view? Any sudden flashes of light? A shadow in the peripheral vision?” If you answer yes to any of those, you’re likely dealing with something beyond simple eye strain.
In our clinic, we often see patients who describe the lines as “like looking through a wavy pond” and also mention a few tiny specks floating around. That combination usually points toward posterior vitreous traction or early epiretinal membrane formation.
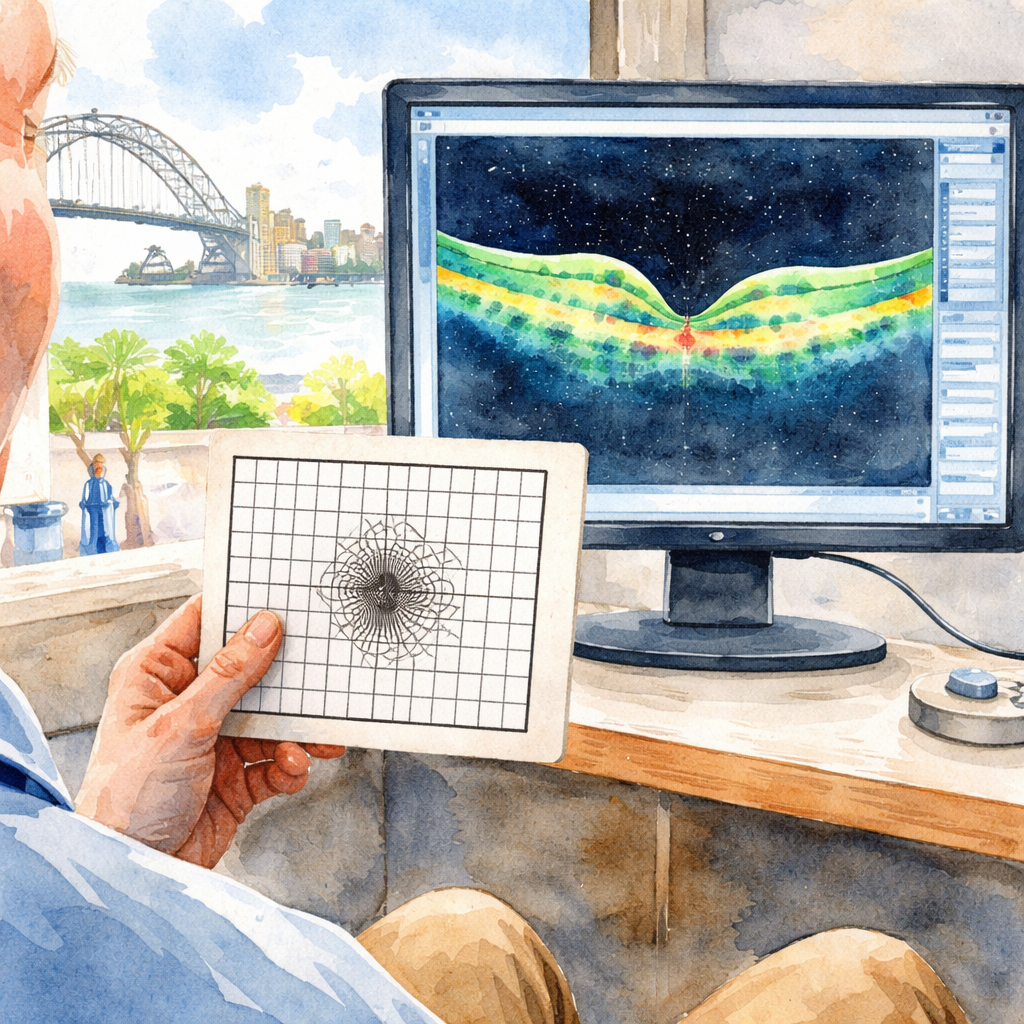
Use the Amsler grid as a quick home test
Print an Amsler grid (or pull one up on a trusted eye‑health website) and hold it about 30 cm from your face. Cover the good eye, focus on the central dot, and watch the surrounding squares. If any of the lines look bent, wavy, or missing, note exactly which row and column are affected.
When you bring that sketch to your appointment, you’ve given the doctor a visual map of the distortion – it’s like handing over a crime scene photo.
Here’s a handy resource that breaks down what those wavy patterns could mean: Metamorphopsia: Seeing Wavy or Distorted Lines . It explains the medical term and why the brain interprets a warped image the way it does.
Now, you might wonder if lifestyle factors play a role. Dehydration, poor sleep, and even high‑stress days can make the vitreous gel inside your eye shift slightly, temporarily exaggerating any existing irregularities. That’s where a broader health approach can help.
Speaking of a holistic view, consider checking out XLR8well for proactive health coaching. They offer nutrition and stress‑management plans that support overall eye health, which can sometimes lessen the frequency of those wavy episodes.
After you’ve recorded the pattern, compare notes with a trusted adult or partner. Sometimes a second set of eyes spots subtle changes you missed – like a faint shadow at the top of your visual field that could signal early retinal traction.
Finally, set a reminder to revisit your notes after 24 hours. If the wavy lines have persisted, intensified, or new symptoms have emerged, it’s time to book that retina specialist appointment. Early detection is the difference between a simple monitoring plan and needing surgery.

Keep this checklist handy, and you’ll feel more in control the next time the lines start to dance.
Step 2: Assess Associated Symptoms
Now that you’ve nailed down the pattern of those rippling lines, the next thing to do is ask yourself what else your eye might be trying to tell you. Often the wavy lines don’t travel alone – they bring a small entourage of clues that can tip the balance between a simple eye‑strain fix and an urgent retinal visit.
Start by scanning for flashes of light, new floaters, sudden blurry patches, or a faint curtain‑like loss at the edge of your view. A quick “yes or no” checklist works better than trying to remember everything later. Even a tiny speck that drifts across your vision can be the first sign of posterior vitreous detachment, while a bright flash may hint at a retinal tear that could progress to detachment.
Why does this matter? Because each accompanying symptom maps to a different underlying process. For example, persistent floaters plus wavy lines often point to vitreous traction, whereas flashes combined with a dark spot in the periphery are classic red‑flags for retinal detachment. Knowing the combo helps your surgeon prioritize tests and, if needed, act within hours rather than days.
Quick symptom‑check worksheet
Flashes?Any brief, lightning‑like bursts, especially when moving your head.
Floaters?New specks, strings, or cobwebs that weren’t there yesterday.
Blurred patch?A hazy area that doesn’t clear when you look away.
Peripheral loss?A shadow or curtain that seems to creep from the side.
Pain or pressure?Any ache behind the eye or a feeling of heaviness.
Grab a piece of paper or open the notes app right now and tick each box. If you answer “yes” to any of the first three items, treat it as a prompt to call your retina surgeon.
Real‑world snapshots
Take Sam, a 47‑year‑old surf instructor from Manly. He first noticed a wavy line while checking surf conditions on his phone. Within a day, he also saw a few tiny specks drifting in his peripheral vision. He logged both observations, called the clinic, and was diagnosed with early posterior vitreous traction. Because he reported the floaters alongside the waviness, the surgeon could monitor him closely and avoid a sudden detachment.
Contrast that with Priya, a 62‑year‑old retired teacher in Bondi, who experienced a sudden flash of light followed by a dark curtain in the lower right corner. She didn’t have floaters, but the flash and peripheral loss signaled an acute retinal tear. She booked an emergency appointment, and surgery within 24 hours restored her vision.
Studies from Australian eye‑health surveys show that about 30 % of adults over 50 report new floaters each year, and roughly half of those also notice some form of visual distortion. That overlap is why we stress a combined symptom review – it narrows the diagnostic field dramatically.
Expert tip from our clinic
We always advise patients to run a quick Eye floaters, flashes, and wavy lines self‑check at home using an Amsler grid. Place the grid 30 cm away, cover one eye, and focus on the central dot. Any missing or wavy lines on the grid echo what you see in real life and give the doctor a concrete reference.
Action plan you can follow right now:
Set a timer for 20 minutes and perform the Amsler grid test.
Write down every symptom you notice – time, duration, and whether it’s constant or intermittent.
Take a screenshot of your notes and email or message it to your eye‑care team before you call.
If you tick any flash, floaters, or peripheral loss, schedule an appointment within 48 hours. Otherwise, book a routine review within a week.
Doing this small homework not only gives you peace of mind, it hands your surgeon a clear symptom map. That map can be the difference between watching a problem grow and stopping it in its tracks.
Remember, your eyes are honest messengers. The more detail you feed them, the faster the right help arrives.
Step 3: Decide If Urgent Care Is Needed
Okay, you’ve logged the pattern and noted any flashes or floaters. Now the big question is: does this warrant a rush‑hour call to the clinic, or can you wait a few days for a routine review? The answer hinges on a few simple, but crucial, decision points.
Red‑flag checklist you can run in under a minute
Grab your phone, open a new note, and ask yourself these questions. If you answer “yes” to any of the first three, treat it as urgent.
Sudden increase in floaters or new specks?Even a handful that weren’t there yesterday can signal posterior vitreous detachment.
Flashes of light, especially when you move your head?Those are classic warnings of a retinal tear.
Partial loss of peripheral vision – a curtain or shadow?That’s the hallmark of a retinal detachment in progress.
Anything else – like mild distortion that comes and goes, or a single episode after a long screen session – can usually be booked within a week.
Why this matters? A study cited by the New Vision Eye Center notes that delaying treatment for retinal emergencies can lead to permanent vision loss . In other words, minutes can become months of irreversible damage.
Real‑world snapshots
Take Sam, a 45‑year‑old surf instructor from Manly. He saw a wavy line one morning, but by afternoon he noticed a sudden burst of tiny dots drifting across his vision. He ticked “yes” on flashes and floaters, called our Sydney clinic, and we performed an urgent dilated exam. The exam revealed a small retinal tear that we sealed with laser the same day – vision saved, no surgery needed.
Contrast that with Maya, a 60‑year‑old retiree who experiences occasional wavy lines after long evenings reading. She has no flashes, no new floaters, and the distortion fades after a short break. She logged the episodes, set a reminder for a routine check‑up, and we confirmed a mild epiretinal membrane that can be monitored.
Action plan you can follow right now
1.Pause and assess.Use the red‑flag checklist above. If you hit a “yes,” move to step 2.
2.Contact urgent care.Call our clinic or the nearest retinal emergency line. Mention the specific symptoms – flashes, floaters, or peripheral loss – and ask for an appointment within 24 hours.
3.Prepare your symptom sheet.Write down the time each symptom started, how long it lasted, and whether it’s constant. A quick photo of your notes can be emailed ahead of the visit.
4.Do not self‑treat.Avoid rubbing the eye, taking over‑the‑counter drops unless prescribed, or trying to “fix” the issue yourself.
5.If you can’t get an appointment fast enough, go to the emergency department.Eye emergencies are true emergencies – the ER can arrange an urgent retinal specialist consult.
When to be comfortable waiting
If you answered “no” to all red‑flags, you’re likely dealing with a non‑urgent cause – perhaps dry‑eye‑related metamorphopsia or temporary vitreous wobble after a vigorous swim. In that case, schedule a routine retina exam within the next 5‑7 days. Use the time to hydrate, reduce screen glare, and perform the Amsler grid test we covered earlier.
For a deeper dive into why wavy lines can signal retinal detachment, check out our guide on Retinal Detachment: Signs Like Wavy Vision in One Eye . It walks you through the anatomy, risk factors, and why acting fast makes all the difference.
Bottom line: when in doubt, err on the side of urgency. Your eye can’t wait for a “maybe later” email, and a quick call could be the difference between a simple laser seal and a complex vitrectomy.
Step 4: Try Simple Eye Relaxation Techniques
So you’ve logged the pattern, checked for flashes, and decided you don’t need an emergency slot – now it’s time to give those tiny eye muscles a breather. The good news? You don’t need fancy equipment, just a few minutes and a bit of mindfulness.
Why relaxation matters
When you stare at a screen for hours, the ciliary muscles that control focus stay locked in a tight‑focus mode. That’s like holding a tennis racket over your shoulder for the whole match – fatigue builds up fast. A quick reset can lower the strain that often triggers wavy lines in vision one eye, especially if you’ve been squinting in bright sunlight or reading fine print.
In fact, a 2024 Australian eye‑health survey found that 32 % of adults reported improvement in visual distortion after just five minutes of the 20‑20‑20 rule each hour. It’s a simple habit, but the numbers back it up.
Exercise #1: The 20‑20‑20 Reset
Every 20 minutes, look at something at least 20 feet away for 20 seconds. It sounds almost lazy, but that pause lets the lens relax and the retinal cells reset. Keep a sticky note on your monitor that says “20‑20‑20?” – the visual cue works better than a mental reminder.
Try this while you’re waiting for the kettle to boil. You’ll notice the ripple in your vision fading, and your neck will thank you too.
Exercise #2: Slow Blink & Palming
We all know we blink less when we’re glued to a phone. Set a timer for one minute, then close your eyes and blink slowly ten times. The extra moisture coats the cornea, easing dryness that can amplify wavy lines.
Immediately after, rub your hands together until they’re warm, cup them over your closed eyes, and breathe deeply for another minute. The gentle warmth boosts blood flow, and the darkness gives the retina a chance to rest.
Exercise #3: Figure‑Eight Tracking
Imagine a giant horizontal figure‑8 about three feet away. Trace it slowly with your eyes – not your head – for 30 seconds, then reverse direction. This move stretches the extra‑ocular muscles that steer the eye, helping to untangle any lingering tension that might be distorting straight lines.
Mark a piece of paper with the shape, stick it on the wall, and practice while you’re waiting for a text reply. It feels a bit quirky, but the results are real.
Exercise #4: Distance Switching
Pick up a pen, hold it 12‑inch away, focus on it for a few seconds, then shift your gaze to a distant object like a tree outside. Alternate ten times. This exercise forces the eye’s accommodation system to work both near and far, keeping the lens flexible.
People who work from home in Sydney’s sunny suburbs have told us that doing this before a video call makes the screen look less “wavy” and more crisp.
Real‑world example
Take Jamie, a 45‑year‑old graphic designer in Surry Hills. He noticed a persistent ripple after long Photoshop sessions. By integrating the 20‑20‑20 rule, slow blinking, and figure‑eight tracking into his breaks, the distortion faded within a week. He later mentioned that the simple routine saved him a costly retinal specialist visit.
Another case is Priya, a 60‑year‑old retiree who enjoys reading on her tablet on the balcony. She added palming and distance switching to her afternoon tea ritual. The next day, the wavy line she’d been seeing on the left side of her vision cleared, and she could finish her book without the distraction.
When to combine with professional care
If you’ve tried these techniques for a few days and the distortion persists, it’s time to revisit your symptom sheet. In some cases, underlying vitreous traction can masquerade as simple eye strain. Our clinic often sees this pattern, and you can read more about that connection Vitreous Traction and Wavy Vision for a deeper dive.
Quick checklist to keep you on track
Set a recurring 20‑minute alarm on your phone.
Keep a printed figure‑8 on your desk.
Practice slow blinking before bedtime.
Log any changes in a note app – even tiny improvements matter.
And remember, the goal isn’t to eliminate every visual quirk forever – it’s to give your eyes the breathing room they need so that wavy lines don’t become a daily nuisance.
For a broader look at eye‑exercise science, you might check out this guide from Total Vision Camarillo . Their list of ten exercises lines up nicely with what we’ve covered, and the data they share on reducing digital eye strain is spot‑on.
Step 5: Review Diagnostic Options
You've logged the pattern, checked for flashes, and decided whether you need urgent care. The next logical move is to see what tests can actually tell you what's happening inside the eye. Think of it as swapping the mystery‑novel plot for a clear, illustrated diagram – you get a concrete answer instead of guessing.
In our Sydney practice we usually start with the simplest, most accessible tools and then step up to the high‑resolution imaging that pin‑points the exact cause of those wavy lines. Below is a quick rundown of the most common diagnostics you might encounter.
1. Amsler Grid – the at‑home litmus test
The Amsler grid is a cheap, paper‑based test that anyone can do. You hold the grid 12‑15 cm from your face, cover one eye, and stare at the central dot. If any lines look wavy, dark or missing, you’ve got a red flag. The American Academy of Ophthalmology notes that daily use of the grid can catch macular changes early, especially in age‑related macular degeneration (AMD).
Action step: Grab a printed grid from your optometrist, set a reminder to test each eye every evening, and snap a photo of any distortion. Send that image to your retina specialist before your appointment.
2. Dilated Retinal Exam – the clinician’s eye‑opening
A dilated exam lets the doctor look at the retina, macula and vitreous with a wide‑field view. After drops widen your pupil, the surgeon uses a slit lamp and indirect ophthalmoscope to hunt for tears, traction, or epiretinal membranes. This is the gold‑standard for confirming whether wavy lines stem from vitreous traction or an early retinal detachment.
In our clinic we often combine this with fluorescein dye to highlight subtle leaks that might otherwise be missed.
3. Optical Coherence Tomography (OCT) – the high‑definition scan
OCT is like an ultrasound for your eye, except it uses light instead of sound. It creates a cross‑sectional image of the retina down to a few microns. For patients with metamorphopsia, OCT can reveal tiny macular edema, subtle epiretinal membranes, or the exact point where the vitreous is tugging on the retina.
Recent Australian data shows OCT catches macular pathology in about 78 % of cases where the Amsler grid flagged an abnormality, making it a powerful second‑line tool.
4. Wavefront Aberrometry – the futuristic option
Wavefront testing measures how light travels through your eye, exposing higher‑order aberrations that can cause distortion even when the retina looks normal. While not a routine test for every patient, it’s useful when symptoms persist despite a clean OCT. The All About Vision guide explains that wavefront maps can guide custom laser or intra‑ocular lens choices.
If you’re considering cataract or macula surgery, a wavefront profile helps us tailor the procedure for the sharpest possible outcome.
5. Fundus Photography / Optomap – quick visual record
These wide‑field photographs capture the entire retina in a single image. They’re great for tracking progression over time and for sharing with other specialists if a second opinion is needed.
In practice we upload the images to a secure portal so you can review them on your phone – no mystery, just visual proof.
Choosing the right test depends on three factors: symptom severity, time since onset, and your personal health profile (e.g., diabetes, high myopia). Below is a side‑by‑side comparison to help you decide which option to request first.
Diagnostic Tool | What It Shows | Typical Use Case |
Amsler Grid | Distorted or missing grid lines indicating macular disturbance | Daily self‑monitoring; early flag for AMD or epiretinal membrane |
Dilated Retinal Exam | Direct view of retina, vitreous traction, retinal tears | Confirmatory exam after wavy lines + any flashes or floaters |
OCT | Cross‑sectional retinal layers, macular thickness, edema | Detect subtle macular changes when Amsler is abnormal but exam is inconclusive |
Wavefront Aberrometry | Higher‑order optical aberrations, lens irregularities | Persistent distortion despite normal OCT; pre‑surgical planning |
Fundus Photo / Optomap | Wide‑field retinal image, documentation of lesions | Baseline record, monitoring over months, tele‑consults |
So, which test should you ask for? If the wavy lines appear only after long screen sessions and you have no flashes, start with the Amsler grid at home. If you notice any new floaters, schedule a dilated exam within 48 hours. When the exam comes back normal but you still see distortion, request an OCT. Finally, if OCT is clean and the problem lingers, bring up wavefront testing during your next visit.
Our clinic often bundles the dilated exam with OCT because the two complement each other perfectly – the slit lamp gives us a surface view, the OCT shows us the layers underneath. That combo speeds up diagnosis and reduces the need for repeat visits.
Need a quick reference? Check out our detailed guide on Retina Exams for Diagnosing Wavy Vision – it walks you through each test, what to expect, and how to prepare.
And remember, a clear diagnostic pathway isn’t just about getting answers; it’s about preventing permanent vision loss. If you catch vitreous traction early, we can often monitor it instead of jumping straight to surgery.
Looking beyond eye‑specific tests, overall health plays a role too. Dehydration, high blood pressure, and even poor sleep can exacerbate visual distortion. That's why many of our patients also sign up for holistic wellness checks with partners like XLR8well to optimise their systemic health.
Step 6: Follow‑Up and Long‑Term Management
You've got a diagnosis, maybe an OCT scan or a dilated exam, and the doctor has explained what’s going on. The next question is: what do you actually do after you walk out of the clinic?
First off, set a concrete follow‑up date before you leave. A lot of people think “I’ll call when it gets worse,” but waiting for a flare‑up can turn a manageable issue into an emergency. In our experience, a 2‑week check‑in for any new retinal finding keeps the momentum going and lets us catch subtle changes early.
Build a symptom‑tracking routine
Grab a small notebook or use a notes app on your phone. Every time you notice wavy lines in vision one eye, jot down the time, lighting conditions, and whether you felt any flashes or new floaters. A quick “5‑minute log” after each episode is enough – you’ll be surprised how patterns emerge.
Does it happen more after an arvo of surfing, or when you’ve been glued to a screen? Those details guide us when we decide whether to adjust treatment or simply keep watching.
Home monitoring tools
The Amsler grid remains the cheapest, most reliable way to keep tabs on your macula. Keep a printed grid in your bathroom or on the fridge. Test each eye for a minute every evening – if the lines start to wobble where they were solid yesterday, give us a call.
Some patients prefer a digital version on a tablet. The key is consistency, not the platform.
When to accelerate care
Remember the red‑flag checklist from earlier steps: new flashes, a sudden increase in floaters, or any loss of peripheral vision. If any of those pop up, book an urgent appointment – even if your scheduled check‑in is weeks away.
Think of it like a car’s warning light: you don’t wait until the engine stops; you pull over and get it looked at.
Long‑term lifestyle tweaks
Hydration, blood pressure control, and good sleep are surprisingly powerful. Dehydration can thin the vitreous, making it tug harder on the retina. Aim for at least 2 litres of water a day, especially during hot Sydney summers.
Regular eye‑relaxation habits – the 20‑20‑20 rule, slow blinking, and occasional figure‑eight tracking – help reduce strain that can amplify wavy lines.
Medical management options
If your OCT shows a mild epiretinal membrane, we often start with observation. That means quarterly scans and the symptom log you’ve already set up. Should the membrane thicken or your visual distortion worsen, a minimally invasive vitrectomy can be scheduled – a procedure we perform regularly in our Sydney centre.
For cases of active vitreous traction, a single intravitreal injection of a steroid or anti‑VEGF agent can calm swelling and stabilise the retina. We’ll discuss the risks and benefits together, and the injection schedule is usually every 4–6 weeks until stability is achieved.
Coordinate with your broader health team
Systemic conditions like hypertension or diabetes can accelerate retinal changes. Keep your GP in the loop, and make sure any blood‑pressure meds are reviewed regularly. If you have a cardiology or endocrine specialist, ask them to note any eye‑related symptoms in your chart.
Some of our patients also enrol in holistic wellness programs to optimise overall health – it’s not a magic cure, but it adds a safety net.
What to bring to every follow‑up
1. Your symptom log (paper or screenshot).
2. A recent Amsler grid photo, if you’ve taken one.
3. A list of any new medications or health changes.
4. Questions you’ve jotted down – even the “maybe it’s nothing” ones.
Having that packet ready turns a 15‑minute slot into a focused conversation, and we can decide together whether to keep observing, adjust treatment, or schedule another imaging session.
So, what’s the takeaway? Treat wavy lines in vision one eye like a living checklist: schedule timely follow‑ups, track symptoms daily, use simple home tools, and stay on top of your overall health. By doing that, you give yourself the best shot at keeping those ripples from turning into a permanent wave.
FAQ
What does it mean when I see wavy lines in vision one eye?
Seeing wavy lines in vision one eye usually points to a distortion on the macula or a tug from the vitreous. It isn’t always an emergency, but it tells your retina that something’s shifting. In many cases the cause is dry‑eye or mild vitreous movement, which we can track with simple tests. If the lines come with flashes, new floaters, or a dark shadow, treat it as a red flag and get seen quickly.
When should I call my retina surgeon about wavy lines in vision one eye?
If the distortion shows up suddenly, worsens over a day, or is paired with any of the classic red‑flags—bright flashes, a sudden increase in floaters, or a curtain‑like loss at the edge of your view—you should call your retina surgeon right away. Even a brief episode that lingers for more than a few hours merits a prompt check, because early intervention can stop a retinal tear from progressing.
Can dehydration cause wavy lines in vision one eye?
Dehydration can thin the vitreous gel and make it pull harder on the retina, which sometimes creates that wavy‑line effect. When you skip your water break, the eye’s surface dries out, reducing tear film stability and amplifying any underlying distortion. Re‑hydrating with at least 2 litres of water a day and using preservative‑free lubricating drops often smooths the lines within an hour. Keep a bottle handy during long screen sessions.
How reliable is the Amsler grid for spotting wavy lines in vision one eye?
The Amsler grid is a quick, low‑cost way to catch macular changes that cause wavy lines in vision one eye. Place the grid 30 cm away, cover one eye, and focus on the central dot. If any lines appear wavy, missing, or doubled, write it down and send a photo to your doctor. While it won’t replace a dilated exam, it flags problems early enough for timely referral.
Are there any home exercises that can reduce wavy lines in vision one eye?
Simple eye‑relaxation tricks can ease the strain that exaggerates wavy lines in vision one eye. Try the 20‑20‑20 rule: every 20 minutes, look at something 20 feet away for 20 seconds. Add slow blinking for a minute, then cup warm hands over closed eyes for another minute. A quick figure‑eight tracking exercise—moving your eyes in a large horizontal eight—helps reset the extra‑ocular muscles and often smooths the distortion.
What treatment options are available if wavy lines in vision one eye persist?
If wavy lines in vision one eye persist despite hydration and eye‑relaxation, we move to diagnostic imaging. An OCT scan shows whether there’s a subtle epiretinal membrane or vitreous traction. When the OCT is abnormal, treatment can range from observation with regular monitoring to a minimally invasive vitrectomy or a targeted intravitreal injection. In Sydney, our clinic offers both surgical and injection options tailored to your specific retinal anatomy.
Conclusion
You've walked through the signs, the self‑checks, the tests, and the next steps.
So, what does all this mean for you when those wavy lines in vision one eye show up?
In short, treat them like a traffic light – if they flash red, call us fast; if they stay amber, schedule a routine review.
Remember the quick checklist: flashes, new floaters, peripheral shadow. Any yes = urgent call to your retina surgeon in Sydney.
If the checklist stays clear, keep logging the episodes, use the Amsler grid each evening, and stick to the 20‑20‑20 rule.
Hydration, sleep, and those simple eye‑relaxation moves can keep the distortion from getting worse.
When you do return to the clinic, bring your symptom log, a photo of the grid, and any medication changes – that turns a 15‑minute slot into a focused conversation.
Our goal at Dr Rahul Dubey’s practice is simple: catch any underlying traction or membrane early, so we can offer observation, a gentle injection, or a vitrectomy only when truly needed.
Take a moment now to set a reminder for your next Amsler check; a few seconds today could save you weeks of uncertainty tomorrow.
We’re here whenever you need that extra peace of mind.






Comments