What Does a Retina Specialist Do: A Practical Guide for Patients
- Dr Rahul Dubey
- Dec 6, 2025
- 16 min read
Ever stared at that fuzzy spot in your vision and thought, "what does a retina specialist do, and why should I care?" You’re not alone—most people only think of eye doctors when they need glasses.
But the retina is the light‑sensing film at the back of your eye, and when it misbehaves, everyday sights can turn into a blur. That’s where a retina specialist steps in, armed with microscopes, lasers, and a deep understanding of the eye’s wiring.
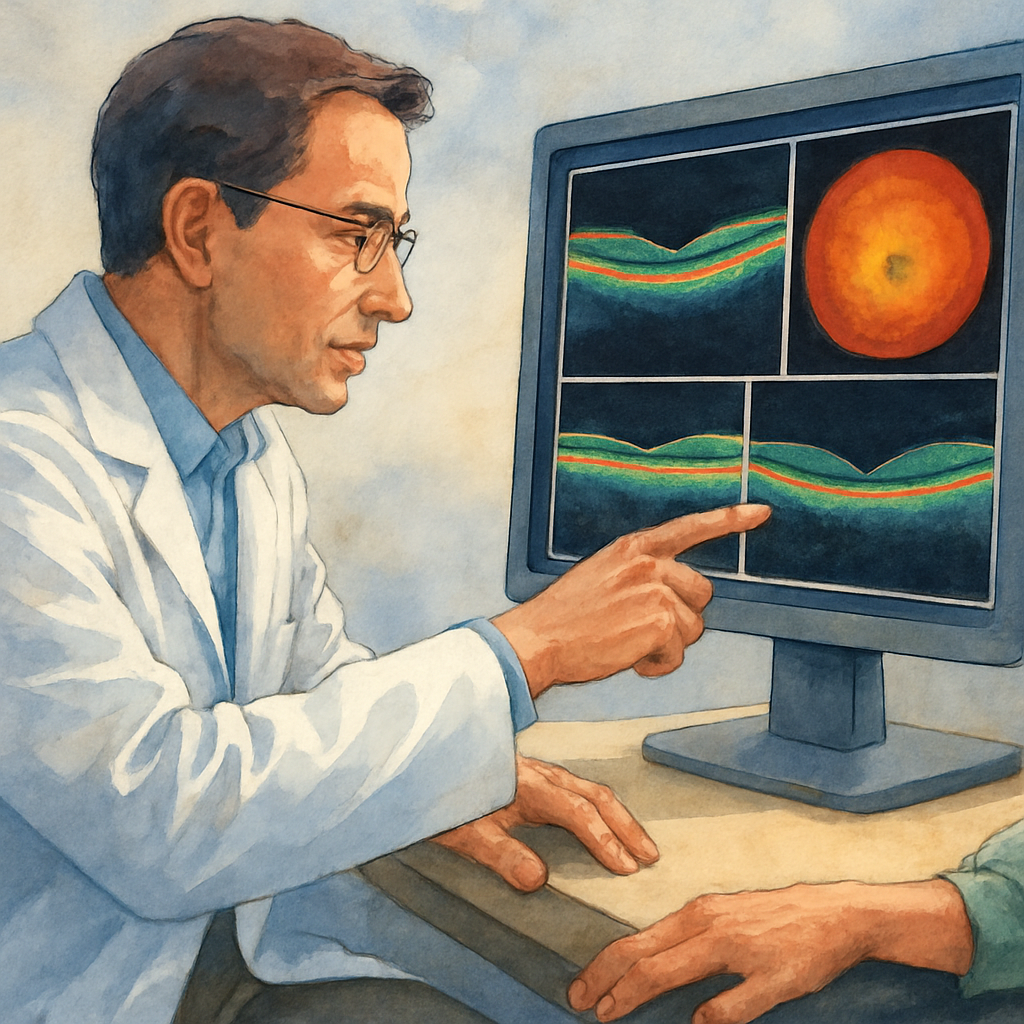
First, they diagnose. Using high‑resolution OCT scans, fluorescein angiography, and detailed eye exams, they pinpoint problems like macular degeneration, diabetic eye disease, or a retinal tear. Imagine a detective pulling out a magnifying glass to spot the tiniest clue—that’s the scan.
Next, they treat. Some issues need a simple laser burn to seal a leaking blood vessel; others require a tiny injection of medication right into the vitreous to halt vision loss. In more complex cases, they perform delicate surgeries—think of a microsurgeon repairing a torn film with instruments thinner than a human hair.
Because every retina is unique, a specialist also creates a personalized care plan. They’ll talk you through lifestyle tweaks, blood‑sugar control, or protective eyewear, tailoring advice to your age, health, and how your eyes are used daily.
So, what does a retina specialist do when you walk into the clinic? They listen to your story, run the right tests, interpret the images, and then recommend the least invasive option that gives you the best chance to keep seeing clearly.
And if you’re in Sydney, you’ll find a surgeon like Dr Rahul Dubey who blends cataract, macula, and retina expertise under one roof—making the whole process smoother, especially if you need a combined procedure.
Feeling a bit overwhelmed? That’s normal. The good news is that advances in imaging and minimally invasive techniques mean most patients recover quickly and get back to their favorite activities.
Ready to take the next step? Book a consultation, ask about the specific tests they’ll run, and make sure you understand the treatment options before any procedure.
Let’s dive in and explore the day‑to‑day work of a retina specialist, so you know exactly what to expect and can feel confident in your eye health journey.
TL;DR
A retina specialist diagnoses and treats conditions like macular degeneration, diabetic eye disease, and retinal tears using advanced imaging, laser therapy, injections, or microsurgery, then creates a personalized care plan for you. Quick recovery and clear vision are the goal, so you can resume again with daily life confidently easily.
Diagnosing Retinal Conditions
When you walk into a retina clinic, the first thing you might wonder is how the doctor can tell what’s wrong without opening your eye. The answer is a mix of careful listening, a detailed eye exam, and some high‑tech imaging that feels more like a crime‑scene investigation than a routine check‑up.
The first look – visual exam and history
Everything starts with a conversation. The specialist asks about the flickering lights you’ve seen, any sudden blind spots, or how long you’ve noticed blurry patches. That story guides the doctor’s eye‑exam, where they use a slit‑lamp and a special lens to peek at the retina’s surface. Small clues – a few red spots, a slight swelling, or a subtle change in the pigment – can point toward macular degeneration, diabetic eye disease, or a tiny tear.
Imaging tools that reveal hidden details
Next comes the tech. Optical coherence tomography, or OCT, gives a cross‑section picture of the retina, layer by layer, so the doctor can see fluid buildup or thinning that the naked eye can’t catch. Fluorescein angiography involves a quick dye injection that lights up blood vessels on a camera, highlighting leaks or blockages. These scans are fast, painless, and produce images you can watch on a screen in real time. If you want a deeper dive into how a retina specialist differs from a general ophthalmologist, check out Retina Specialist vs Ophthalmologist: Key Differences Explained for a clear comparison.
These images do more than just confirm a diagnosis; they help the doctor decide whether a laser, an injection, or surgery is the best next step. For example, a thin layer of fluid under the macula seen on OCT often means an anti‑VEGF injection will be recommended, while a well‑defined leak on angiography might be treated with targeted laser photocoagulation.
If you’re curious about how clinics attract patients who need these precise tests, many are turning to health‑marketing partners that specialize in the medical space. Healthier Lifestyle Solutions helps eye doctors get found online and connect with the right audience.
When a retinal tear is suspected – the role of B‑scan ultrasound
Sometimes the retina is clouded by cataract or vitreous haze, making direct view difficult. In those cases a B‑scan ultrasound sends sound waves through the eye to map the retina’s shape. The doctor can spot a tiny flap or a subtle detachment that would otherwise be hidden.
Understanding your insurance coverage early can save headaches later. A quick read of group health insurance options can show you which plans include retinal procedures and what out‑of‑pocket costs to expect.
All this data – your story, the exam findings, and the imaging results – comes together in a diagnosis that feels like a puzzle finally fitting together. The specialist then outlines a personalized plan, explaining why a particular test or treatment is chosen and what you can expect in recovery.
That video walks you through a typical OCT scan, showing how each layer lights up and why those patterns matter. Watching it can demystify the process and make the next appointment feel less intimidating.
Bottom line: diagnosing retinal conditions is a blend of listening, looking, and letting technology reveal what’s hidden. Once the diagnosis is clear, the treatment path becomes much easier to navigate, and you can move forward with confidence knowing exactly what’s happening inside your eye.
Performing Retinal Surgeries
When the retina is threatened, a surgeon’s toolbox suddenly looks a lot like a miniature workshop. You walk in expecting a quick fix, but what actually happens is a series of carefully timed steps that blend science, skill, and a bit of artistry.
Why surgery is often the last‑resort answer
Most retinal problems start with non‑invasive treatments – laser spots, anti‑VEGF injections, or cryotherapy. We only move to surgery when those measures can’t seal a tear, stop fluid buildup, or remove scar tissue. The goal is always to preserve the delicate layers of the retina while keeping your recovery as smooth as possible.
Think about it like fixing a tear in a silk scarf. You could stitch it, but the stitch itself might be visible. A retina surgeon tries to “stitch” the eye without leaving a scar that blocks light.
Three main surgical approaches
1. Pneumatic retinopexy– a tiny gas bubble is injected into the eye, pressing the detached retina back into place. A laser or cryotherapy then seals the break. It’s done in the clinic, no operating room needed.
Real‑world data show a mixed success rate. A 2024 Medscape report notes a single‑operation success of about 59 % across 16,668 cases, dropping to 54 % when the eye had prior cataract surgery according to the IRIS registry analysis . The numbers remind us that case selection matters – a more invasive procedure may be wiser for complex detachments.
2. Pars plana vitrectomy (PPV)– the surgeon removes the vitreous gel, clears any scar tissue, and uses tiny tools to repair the retina. It’s the go‑to for large tears, proliferative diabetic retinopathy, or when a retinal hole has formed.
At NJ Retina, surgeons describe PPV as “the workhorse of modern retinal surgery” because it lets them address multiple issues in one session according to their practice overview . The procedure typically lasts 45‑90 minutes, and most patients leave the OR the same day.
3. Scleral buckle– a silicone band is sewn around the outside of the eyeball, gently indenting the wall so the retina can re‑attach. It’s an older technique but still valuable for certain peripheral tears.
Because the buckle sits on the eye’s surface, you’ll notice a slight change in eye shape after surgery, but many patients appreciate that it avoids any intra‑ocular gas.
Step‑by‑step: What to expect on the day of surgery
Pre‑op briefing – you’ll review imaging (OCT, B‑scan) and the surgeon will explain which technique fits your case.
Anesthesia – most retinal surgeries use local anesthesia with a mild sedative; you stay awake and can talk to the team.
Procedure – the surgeon works under a microscope, using instruments finer than a human hair.
Immediate post‑op – a protective shield is placed over the eye, and you’ll get instructions on positioning (e.g., face‑down for gas bubbles).
Follow‑up – the first OCT or fundus photo is usually done within 24‑48 hours to confirm the retina stays attached.
Each of these steps is designed to keep you informed and comfortable. Ask your surgeon for a copy of the intra‑operative video or photos; seeing the tiny instruments in action can demystify the whole process.
Actionable checklist for your surgery day
Bring a list of all medications – especially blood thinners.
Arrange a driver; you’ll need someone to take you home after the brief recovery.
Wear comfortable clothing and avoid tight collars that could press on the eye.
Prepare a cool, dark room at home for the first 24 hours if you have a gas bubble.
And remember, you don’t have to navigate insurance alone. Many patients find it helpful to explore coverage options early. For a quick overview of group health plans that often include ophthalmic coverage, check out this guide on small business group health insurance options . It can save you surprise out‑of‑pocket costs later.
If you’re a clinic looking to attract more retinal patients, partnering with a health‑marketing agency that specializes in medical ads can boost visibility. The team at Health Stack Media helps eye doctors run targeted Facebook and TikTok campaigns, putting your surgical expertise in front of the right audience.
Finally, if you want a quick snapshot of everything Dr. Rahul Dubey offers – from cataract to complex retinal surgery – take a look at our Services | Dr Rahul Dubey page. It breaks down each procedure, recovery timeline, and what you can expect on the day of your operation.
Advanced Imaging and Technology
When you walk into a retina clinic today, the first thing you’ll notice isn’t a stack of lenses – it’s a wall of screens. Those monitors are feeding you data that a decade ago would have required a biopsy.
Let’s start with the workhorse: Optical Coherence Tomography (OCT). Think of OCT as an ultrasound that uses light instead of sound. It slices the retina layer‑by‑layer, giving you a cross‑section that looks like a topographic map of a mountain range. That map tells the doctor whether fluid is hiding under the macula, whether a thin spot is about to break, or if scar tissue is creeping in.
But OCT alone isn’t the whole story. OCT‑Angiography (OCT‑A) adds a blood‑flow overlay without any dye. It’s like watching traffic on a city street from a helicopter – you see where the cars (blood cells) are moving and where a jam (blocked vessel) is forming. In pediatric cases, OCT‑A is becoming the go‑to for spotting early retinopathy of prematurity, because you can detect abnormal vessels before they bleed.
Why multimodal matters
Imagine trying to solve a jigsaw puzzle with only the edge pieces. That’s what you get if you rely on a single imaging mode. Modern retina specialists combine OCT, OCT‑A, and sometimes fluorescein angiography (FA) to fill in the gaps. FA still has a role when you need to see leakage in real‑time – the dye lights up leaking vessels like neon signs.
Real‑world example: Maya, a 7‑year‑old born preterm, came in with subtle squinting. Her OCT showed a thin retinal layer, but OCT‑A revealed a tiny network of abnormal vessels that hadn’t yet leaked. The specialist started early laser therapy, and Maya avoided the vision loss that many preterm kids face.
Emerging tech you should know
Adaptive optics scanning laser ophthalmoscopy (AO‑SLO) is a mouthful, but the idea is simple – it corrects for the eye’s own imperfections, letting you see individual photoreceptors. Researchers at Duke’s Eye Center are using AO‑SLO to track how gene‑therapy injections reshape the retina over months. The same team also runs a yearly workshop on the newest pediatric retina advances, where they demo live intra‑operative videos and discuss how to avoid common pitfalls.
Another breakthrough is wide‑field imaging. Traditional fundus cameras capture about 30‑degree views; wide‑field systems grab up to 200 degrees, letting doctors spot peripheral tears that would otherwise be missed. In a recent series of 200 retinal detachments, the addition of wide‑field imaging increased early detection of peripheral breaks by 22%.
Actionable checklist for your next appointment
Ask your doctor which imaging modalities they’ll use and why – knowing the purpose helps you follow the plan.
Request a copy of the OCT or wide‑field photos; seeing the image makes the diagnosis less abstract.
If you have a child with a history of prematurity, ask whether OCT‑A is part of the screening protocol.
Bring a list of any recent visual changes, even fleeting ones like “spots that disappear in a second.”
Understanding the tech also helps you ask smarter questions. For instance, you might say, “I saw a fluid pocket on the OCT – does that mean I need an anti‑VEGF injection now, or can we monitor?” That shows you’re engaged and makes the conversation feel like a partnership.
And if you’re a retina surgeon yourself, the pressure to stay current is real. Burnout is a hidden cost of mastering ever‑more complex equipment. That’s why many clinicians turn to resources like e7D‑Wellness for evidence‑based wellbeing assessments and practical strategies to keep the burnout clock at bay.
Finally, for patients dealing with diabetes‑related changes, a deeper dive into how imaging guides treatment can be found on the Diabetic Eye Disease page. Knowing what each scan reveals empowers you to make informed choices about injections, laser sessions, or lifestyle tweaks.
Bottom line: advanced imaging isn’t a gimmick; it’s the compass that steers every decision in modern retina care. The more you understand the maps, the better you’ll navigate your own eye health journey.
Managing Chronic Eye Diseases
Living with a chronic eye condition feels a bit like trying to keep a garden alive during a drought—you keep checking, watering, and hoping nothing wilts. The good news is that a retina specialist knows exactly which tools to use to keep your vision thriving.
First, you need to know what you’re up against. The most common long‑term foes are diabetic retinopathy, age‑related macular degeneration (AMD), chronic macular edema, and retinal vein occlusions. Each one follows its own rhythm, but they all share one thing: they need ongoing, personalized monitoring.
Why does monitoring matter? Because the retina can change subtly day by day. A tiny rise in fluid on an OCT scan might be the first hint that a treatment tweak is needed. Skipping appointments is like ignoring a leaky pipe—you’ll only end up with a flood later.
Retina specialists lean on a toolbox of imaging: high‑resolution OCT for layer‑by‑layer snapshots, OCT‑A for blood‑flow maps, and regular visual‑acuity charts to catch functional shifts. Together they create a live dashboard of your eye health.
Here’s a quick visual guide to what you’ll see in a typical follow‑up:
After you watch the video, you’ll notice the specialist walks you through each image, pointing out the tiny red dots that signal fluid or new vessels. That conversation is where you become a partner in care, not just a passive patient.
Let’s compare two of the big players. Diabetic retinopathy often starts with micro‑aneurysms that leak fluid. Early on, the specialist may recommend tight blood‑sugar control and a series of anti‑VEGF injections if macular edema appears. AMD, on the other hand, usually shows drusen buildup and can progress to neovascular (wet) AMD, where the treatment shifts to monthly injections of a different medication and possibly lifestyle tweaks like AREDS2 supplements.
Disease | Monitoring Frequency | Typical Treatment Path |
Diabetic Retinopathy | Every 3‑6 months (or sooner if changes) | Laser photocoagulation → anti‑VEGF injections if edema develops |
Age‑Related Macular Degeneration (AMD) | Every 4‑6 months for dry, monthly for wet | AREDS2 supplements → anti‑VEGF injections for neovascular AMD |
Chronic Macular Edema | Every 1‑2 months | Anti‑VEGF or steroid injections, consider focal laser |
The table above gives you a snapshot of how often you’ll be seen and what the usual steps look like. Think of it as a cheat sheet you can keep on your phone.
Practical tip: always bring a list of any new visual quirks—like “spots that disappear after a second” or “new glare at night.” Write them down before your visit. The specialist can cross‑reference those notes with the OCT images, making the decision‑making faster and more precise.
If you’re wondering how AMD fits into the bigger picture, check out the detailed guide on Age Related Macular Degeneration | Dr Rahul Dubey . It breaks down the stages, lifestyle tweaks, and why regular imaging matters.
Bottom line: managing chronic eye disease is a marathon, not a sprint. By staying on top of imaging, keeping open communication, and following the specialist’s tailored plan, you give your retina the best chance to stay healthy for years to come.
When to See a Retina Specialist: Referral Criteria
Imagine you’re scrolling through photos on your phone and suddenly a dark patch drifts across the screen. Your heart skips a beat because you know that’s not normal. That moment is the cue to ask yourself, "Do I need a retina specialist?"
The short answer: yes, when the warning signs go beyond what an optometrist can manage. A retina specialist has the tools—high‑resolution OCT, laser, and microsurgical expertise—to catch problems before they steal more vision.
Red‑flag symptoms that demand a referral
We’ve all heard about flashes and floaters, but they’re more than just annoying specks. New or increasing floaters, especially with flashes of light, often signal a posterior vitreous detachment that can lead to a retinal tear. According to Desert Retina Consultants , sudden blurry spots or a dimming area of vision may indicate a macular hole or early detachment—conditions that need urgent specialist attention.
Other tell‑tale signs include:
Sudden loss of central vision (you can’t read a street sign clearly).
Persistent dark shadows that don’t go away with blinking.
Unexplained distortion—straight lines look wavy.
Rapid increase in eye pain combined with redness.
When any of these pop up, schedule a retina consult within 24‑48 hours. Delays can turn a treatable issue into permanent vision loss.
Medical conditions that automatically trigger a referral
If you have diabetes, you’re already on the radar. Diabetic retinopathy progresses silently, and regular retinal imaging is the only way to spot micro‑aneurysms before they bleed.
Age‑related macular degeneration (AMD) is another silent thief. Even if you’re not yet in the “wet” stage, a specialist can monitor drusen growth and recommend AREDS2 supplements or early anti‑VEGF therapy.
People with a history of eye trauma, high myopia, or previous retinal surgeries also fall into the high‑risk bucket. In those cases, a retina specialist should be part of your routine eye‑care team.
How the referral process works
Typically, your optometrist will note the symptom, run a quick fundus photo, and then send a referral note. They’ll include any recent visual changes you’ve logged, your systemic health info (blood pressure, blood sugar), and any imaging they already have.
When the retina specialist receives the referral, they’ll prioritize you based on urgency. You’ll often get an OCT or wide‑field scan within a few days, and the doctor will explain the findings in plain language.
One practical tip: bring a written list of the exact date you first noticed each symptom. It helps the specialist map the progression and decide whether immediate treatment or close monitoring is best.
When a specialist says “watch and wait”
Not every red flag means surgery. Sometimes the retina looks stable, and the doctor will schedule more frequent OCTs—maybe every 1‑2 months—to keep an eye on subtle fluid changes. That’s why the phrase “monitor closely” feels reassuring rather than vague.
In other cases, a single anti‑VEGF injection can halt fluid buildup before it harms the macula. The key is that a retina specialist knows exactly which intervention matches your specific pattern.
For a deeper dive into when surgery becomes necessary, check out our guide on macular hole treatment options . It walks through the decision‑tree that many patients face.
So, what’s the bottom line? If you notice any sudden visual change, have a high‑risk medical condition, or your regular eye doctor flags a retinal concern, treat it like a fire alarm—call a retina specialist right away.
Conclusion
If you’ve stuck with us this far, you now have a clear picture of what does a retina specialist do—from spotting the tiniest fluid pocket on an OCT to deciding whether a single anti‑VEGF injection or a microsurgical repair is right for you.
That knowledge matters because vision loss rarely announces itself with a warning label. The moment you notice a flash, a new floaters, or a shadow in the center of your view, a retina specialist can turn a potential emergency into a manageable treatment plan.
In short, the specialist combines high‑resolution imaging, precise laser or injection therapy, and, when needed, delicate surgery to protect the delicate layers of your retina. They also give you a personalized monitoring schedule so you stay ahead of any subtle changes.
So, what’s the next step for you?
Write down the exact date you first saw any new visual change, gather your medical history, and bring that list to your next eye appointment. Ask your doctor which imaging tests will be used and why—you’ll feel more in control.
When you’re ready to move from “maybe” to “I’m taking action,” reach out to a retina specialist in Sydney. Dr Rahul Dubey’s clinic offers comprehensive evaluations, same‑day OCT imaging, and a clear plan tailored to your lifestyle.
Remember, treating a retinal warning early is the fastest route to keeping your world in focus. Let’s make sure your eyes get the expert care they deserve.
FAQ
What does a retina specialist do during my first appointment?
During that first visit the doctor will ask you to describe every visual change—flashes, new floaters, blurry spots. Then they’ll dilate your eyes and capture high‑resolution images like OCT and fundus photos. Those pictures let the specialist pinpoint the exact layer of the retina that’s affected and explain the next steps in plain language, so you know exactly what’s happening.
How can I tell if I need to see a retina specialist right away?
If you notice sudden flashes, a curtain‑like shadow, or a rapid loss of central vision, treat it like a fire alarm. Those symptoms often signal a retinal tear or detachment, which requires urgent evaluation. Even if the change feels mild, write down when it started and call the clinic within 24‑48 hours—early care can save the sight you love.
What imaging tests will the retina specialist use and why?
Most specialists combine at least two scans. OCT gives a cross‑section view of fluid or thinning, while OCT‑Angiography maps blood flow without dye. In some cases they add fluorescein angiography to highlight leaking vessels. Each test fills a different puzzle piece, helping the doctor decide whether you need laser, an injection, or just close monitoring.
Are laser treatments and injections safe, and what should I expect?
Both procedures are performed in‑office with numbing drops, so you stay awake and can talk to the team. A laser feels like a quick zap—no pain beyond a brief sting. Injections involve a tiny needle placed into the vitreous; most patients feel a slight pressure but recover within minutes. Expect a brief recovery plan, like avoiding heavy lifting for a day.
When is surgery necessary and what does recovery look like?
Surgery becomes the option when a tear won’t seal with laser or fluid keeps building despite injections. Techniques like pars plana vitrectomy or pneumatic retinopexy restore the retina’s position. You’ll likely go home the same day, wear an eye shield, and follow a positioning schedule—often face‑down for a few days if a gas bubble is used. Vision improves gradually over weeks.
How often should I schedule follow‑up visits for a chronic condition?
Frequency depends on the disease. Diabetic retinopathy usually calls for checks every three to six months, while wet AMD often needs monthly visits to monitor fluid on OCT. Your specialist will set a personalized calendar and remind you to bring any new visual quirks—like spots that appear and vanish—so adjustments can be made before vision slips.
What can I do at home to support my retina health between appointments?
Control systemic factors: keep blood sugar and blood pressure in range, quit smoking, and protect your eyes from UV light with sunglasses. Eat leafy greens, fish rich in omega‑3s, and stay hydrated. If you notice any new flashes or floaters, write them down immediately and call your clinic—early reporting often prevents bigger problems.






Comments