Vitreous Hemorrhage Causes: What Triggers This Eye Condition and How to Respond
- Dr Rahul Dubey
- Nov 28
- 16 min read
Imagine waking up one morning and noticing dark specks drifting across your vision, like tiny dust motes in a sunbeam. For many, that's the first sign of a vitreous hemorrhage, and it can feel terrifying because you don't know what's causing it.
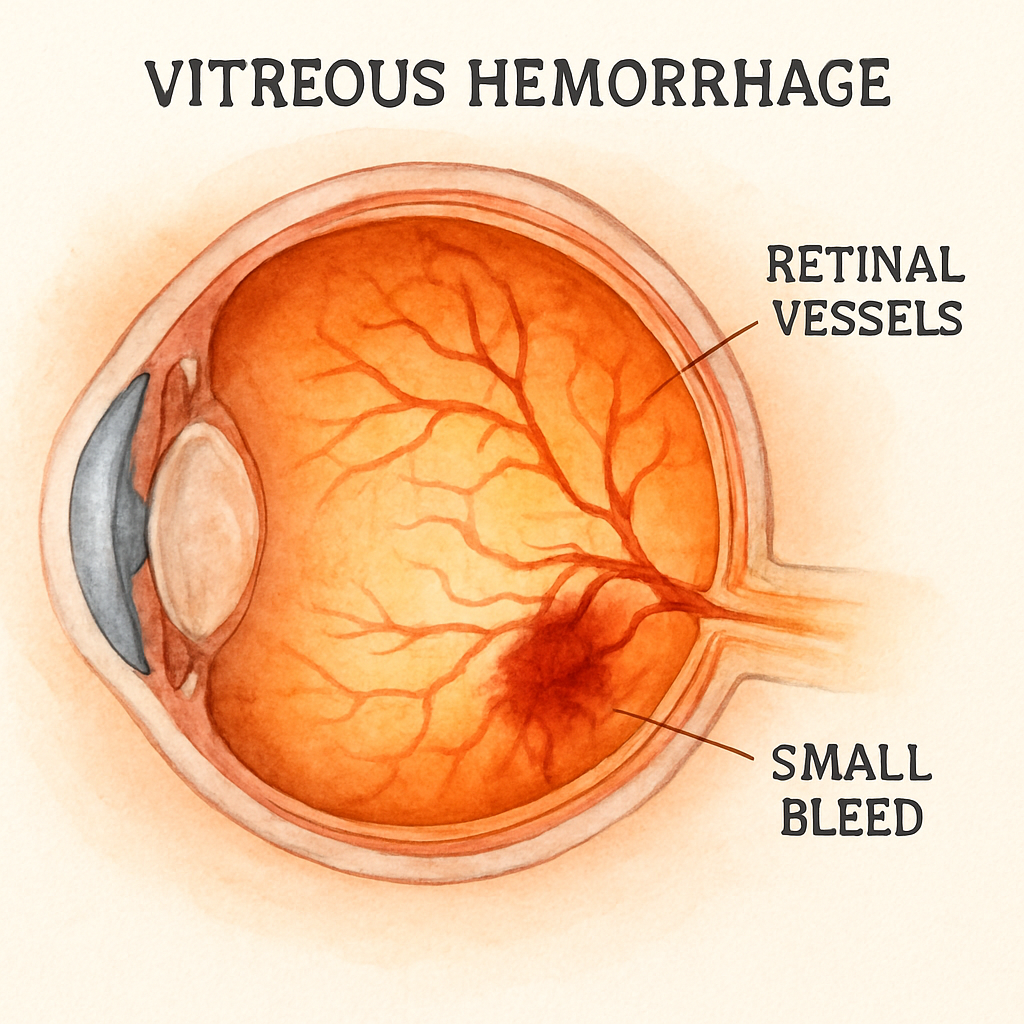
Vitreous hemorrhage occurs when blood leaks into the clear gel that fills the back of the eye. The most common culprits are retinal tears that happen as the vitreous pulls away from the retina, a process known as posterior vitreous detachment. When the tug is strong enough to tear a retinal blood vessel, blood seeps into the vitreous cavity. In my practice, I've seen a 55‑year‑old runner who felt a sudden "curtain" over his vision after a vigorous jog; an exam revealed a small retinal tear that had bled.
Another frequent cause is proliferative diabetic retinopathy. High blood sugar damages tiny retinal vessels, making them fragile and prone to leaking. A patient with long‑standing diabetes once described spotting red floaters that grew denser over days, eventually blurring her reading. A fluorescein angiogram confirmed new vessels had burst, flooding the vitreous with blood.
Trauma is also a big player. Even a seemingly minor blunt impact—like being hit by a stray baseball—can rupture retinal vessels. I recall a teenager who was hit in the eye during a soccer match; an ultrasound showed a modest hemorrhage that cleared after a short observation period, but the incident highlighted how quickly injury can translate into bleeding.
Less common, but still important, are retinal vein occlusions. When a retinal vein becomes blocked, pressure builds up behind the blockage and can cause hemorrhage into the vitreous. For a deeper look at how vein occlusions relate to vitreous bleeding, check out this detailed guide on Vitreous Floaters | Dr Rahul Dubey .
So, what can you do if you suspect a vitreous hemorrhage? First, stop any activity that could worsen the situation—avoid heavy lifting or strenuous exercise. Second, schedule an urgent appointment with a retina specialist; early intervention can prevent permanent vision loss. Third, keep a list of your medical conditions handy, especially diabetes or hypertension, as these increase risk.
Managing the emotional stress of an unexpected eye problem is just as crucial as the medical treatment. Healthcare professionals often face burnout when dealing with urgent retinal cases. Resources like e7D-Wellness offer evidence‑based strategies to support clinician wellbeing during stressful periods.
By recognizing the warning signs and understanding the typical causes—retinal tears, diabetic retinopathy, trauma, and vein occlusions—you empower yourself to seek prompt care and protect your sight.
TL;DR
Vitreous hemorrhage causes range from retinal tears and diabetic retinopathy to trauma and vein occlusions, each capable of quickly clouding vision.
Recognize symptoms early, stop strenuous activity, and see a retina specialist promptly to protect your sight.
Early detection and proper care can prevent permanent damage and preserve vision effectively.
Understanding Vitreous Hemorrhage
When you first notice a curtain of red floaters, it’s natural to wonder what’s actually happening inside your eye. The short answer? Blood has leaked into the clear gel that fills the back of the eye – the vitreous. That’s what we call a vitreous hemorrhage, and the causes fall into three broad families: abnormal vessels, ruptured normal vessels, and blood spilling over from a nearby source.
Abnormal Vessels – When New Blood Vessels Go Rogue
Diseases that force the retina to grow new, fragile vessels are the biggest culprits. Diabetes is the classic example. High blood sugar weakens tiny retinal capillaries, and the eye responds by sprouting neovascular tissue that lacks proper wall integrity. When these newborn vessels break, blood pours straight into the vitreous.
Retinal vein occlusions work the same way. A blocked vein raises pressure, prompting the retina to generate new vessels that are prone to bleeding. Even less common conditions like sickle‑cell retinopathy or ocular ischemic syndrome follow the same pattern – ischemia sparks VEGF, VEGF drives leaky vessels, and the leak becomes a hemorrhage.
One of my patients, a 62‑year‑old with poorly controlled diabetes, woke up to a sudden clouding of vision. A quick exam revealed a proliferative diabetic retinopathy with active neovascularization. The blood was coming from those very new vessels.
Ruptured Normal Vessels – The Pull of Posterior Vitreous Detachment
Even perfectly healthy vessels can burst when they’re tugged too hard. As we age, the vitreous gel begins to liquefy and pulls away from the retina – a process called posterior vitreous detachment (PVD). The strongest attachments are at the vitreous base, the optic nerve head, and the retinal vasculature. When traction hits a retinal vessel at one of those spots, the wall can snap.
Think about it like a rubber band snapping back after being stretched. In an acute PVD, the risk of a concurrent retinal tear jumps to 70‑95 %. That tear can let blood escape into the vitreous.
Last winter, a 48‑year‑old avid cyclist felt a sharp “pop” while descending a hill and then saw a cascade of red specks. An ultrasound confirmed a small retinal tear with associated hemorrhage – classic PVD‑related bleeding.
Blood from Adjacent Sources – When the Neighbour Joins the Party
Sometimes the blood isn’t coming from the retina at all. It can seep in from a macroaneurysm, a choroidal neovascular membrane, or even a tumor. These sources break through the internal limiting membrane and spill directly into the vitreous cavity.
A 70‑year‑old woman with age‑related macular degeneration developed a sudden dense hemorrhage. Imaging showed a ruptured choroidal neovascular lesion that bled into the vitreous – a perfect illustration of “blood from an adjacent source.”
Practical Steps When You Suspect a Hemorrhage
1.Stop what you’re doing.Heavy lifting, intense exercise, or any activity that raises intra‑ocular pressure can worsen bleeding.
2.Elevate your head.Sleeping with the head of the bed slightly raised helps the blood settle inferiorly, giving the doctor a clearer view of the retina.
3.Schedule an urgent retinal evaluation.An eye‑care professional will use indirect ophthalmoscopy, B‑scan ultrasound, and sometimes OCT to pinpoint the source.
4.Manage systemic risk factors.Tight glucose control for diabetics, blood‑pressure management, and smoking cessation all reduce the chance of recurrence.
5.Know the treatment options.If a retinal tear is found, laser photocoagulation or cryotherapy can seal it. For neovascular causes, pan‑retinal photocoagulation or anti‑VEGF injections are the go‑to therapies. When bleeding won’t clear on its own, a pars‑plana vitrectomy may be required.
While you’re waiting for your appointment, you might find it helpful to read more about floaters and how they relate to vitreous bleeding. The Vitreous Floaters | Dr Rahul Dubey page breaks down the symptom checklist and why early detection matters.
For surgeons, having the right equipment can make a difference in both diagnosis and treatment. Modern imaging tools and vitrectomy systems are often supplied by specialists like Medart , which partners with eye clinics to keep the latest technology on hand.
Bottom line: vitreous hemorrhage is rarely an isolated event. Understanding whether the bleed stems from abnormal neovascular growth, a mechanical tear, or an adjacent lesion guides the treatment plan and helps you get back to clear vision faster.
Common Medical Causes
When you finally pin down why blood is drifting in the vitreous, the treatment path becomes a lot clearer. Below we break down the most frequent medical culprits, sprinkle in real‑world stories, and give you concrete next steps.
Abnormal New Vessels – When Growth Goes Rogue
High blood sugar can turn tiny retinal capillaries into fragile, leaky sprouts. In proliferative Diabetic Eye Disease , these newborn vessels burst easily, dumping blood straight into the vitreous gel. I remember a 62‑year‑old who woke up with a curtain‑like haze; a fluorescein angiogram revealed a swarm of neovascular loops that had just ruptured.
Retinal vein occlusion follows a similar pattern. A blocked vein builds pressure, forces the retina to grow new vessels, and those vessels tend to bleed. One patient, a 58‑year‑old accountant, noticed sudden floaters after a stressful week; the exam showed a branch retinal vein occlusion with active bleeding.
Sickle‑cell retinopathy is less common but works the same way – sickled cells clog tiny vessels, the eye responds by sprouting weak new ones, and the next thing you know you’re seeing red specks.
Ruptured Normal Vessels – The Pull of Posterior Vitreous Detachment
As we age, the vitreous gel liquefies and tugs away from the retina. The strongest attachment points are the optic disc and retinal vessels. When that pull snaps a healthy vessel, blood spills into the vitreous.
Picture a cyclist descending a steep hill. Last winter, a 48‑year‑old avid rider felt a sudden “pop” and then a cascade of red dots. An ultrasound confirmed a small retinal tear with adjacent hemorrhage – classic PVD‑related bleeding.
Even a seemingly harmless eye‑rub can generate enough traction to tear a vessel in a myopic eye. A teenage soccer player once came in after a hard ball hit his eye; a quick exam showed a peripheral tear with a tiny bleed that cleared in two weeks.
Blood from Adjacent Sources – When the Neighborhood Joins the Party
Macroaneurysms are balloon‑like dilations of retinal arteries that can burst and leak into the vitreous. A 70‑year‑old with hypertension developed a sudden dense hemorrhage; imaging pinpointed a ruptured macroaneurysm as the source.
Choroidal neovascular membranes, common in age‑related macular degeneration, can also break through the internal limiting membrane and pour blood forward. One patient described the moment as “watching a fireworks display inside my eye.” The bleed cleared only after a series of anti‑VEGF injections.
Rarely, intra‑ocular tumors such as retinoblastoma or metastatic lesions erode nearby vessels, leading to a vitreous bleed. While uncommon, it’s a reminder to consider systemic oncology history when the bleed is unexplained.
Practical Steps When You Suspect a Hemorrhage
1. Stop strenuous activity.Heavy lifting, intense cardio, or even vigorous eye rubbing can worsen the bleed.
2. Elevate your head.Sleeping with the head of the bed raised a few inches encourages blood to settle inferiorly, giving your doctor a clearer view.
3. Get an urgent retinal evaluation.An eye‑care professional will use indirect ophthalmoscopy, B‑scan ultrasound, and possibly OCT to locate the source.
4. Manage systemic risk factors.Tight glucose control, blood‑pressure management, and quitting smoking dramatically lower the chance of recurrence.
5. Know the treatment options.Retinal tears often seal with laser photocoagulation or cryotherapy. Neovascular sources respond to pan‑retinal laser or anti‑VEGF injections. Persistent bleeding may require pars‑plana vitrectomy.
Keeping a symptom diary—note when the floaters appear, any recent injuries, and changes in systemic health—helps your specialist tailor the right plan.
For a deeper dive into how systemic diseases influence eye health, check out the resources from Harvey Bruce Blinds, Shutters & Interiors , which surprisingly offers a well‑written overview of patient lifestyle factors that impact ocular outcomes.
Trauma‑Related Causes
Ever felt a sudden jolt to your eye and thought, “That was just a bump, nothing serious”? Too often that feeling masks a hidden bleed inside the vitreous.
Blunt trauma is the most common culprit. A stray baseball, a hard fist, or even a vigorous eye‑rub can transmit enough force to rupture tiny retinal vessels. When the vitreous shifts, it can pull on the retina, tearing blood vessels and spilling blood into the gel.
Penetrating injuries are rarer but far more devastating. A shard of glass or a metal fragment that actually pierces the globe creates a direct pathway for blood to flood the vitreous chamber.
What about indirect trauma? Think of a high‑speed car accident where the head snaps forward. The rapid deceleration can cause a coup‑contrecoup effect inside the eye, leading to a choroidal rupture or a retinal tear that bleeds.
Sports enthusiasts hear this story a lot: a soccer player gets hit by a ball, feels a “pop” behind the eye, and later notices red floaters swirling around. In many cases the bleed clears on its own, but sometimes the damage is enough to require laser or surgery.
One of my patients, a 34‑year‑old cyclist, collided with a car door. He reported immediate vision “cloudiness” and a painful ache. An OCT scan revealed a small macular hole caused by the impact. If left untreated, that hole could lead to permanent central vision loss. You can read more about macular holes and how trauma can trigger them macular hole .
Orbital fractures add another layer of risk. When the bony socket breaks, bone fragments can lacerate retinal vessels from the outside, creating a vitreous hemorrhage that often accompanies other eye injuries.
So, how do you know when a traumatic bleed needs urgent attention? Ask yourself:
Did the vision become suddenly darker or “curtain‑like”?
Is there pain, flashing lights, or a noticeable loss of peripheral vision?
Did the injury involve a high‑speed impact or a penetrating object?
If you answer “yes” to any of those, you’re in the “see a retina specialist now” zone.
Here’s a quick checklist you can keep in your phone or on a sticky note:
Stop any activity that raises intra‑ocular pressure – no heavy lifting, no vigorous eye rubbing.
Apply a cold compress to the eyelid (never directly on the eye) to reduce swelling.
Elevate your head while you rest; this helps the blood settle inferiorly and gives the doctor a clearer view.
Schedule an urgent retinal exam – an indirect ophthalmoscopy or B‑scan will pinpoint the bleed.
Bring a list of recent injuries, medications, and any pre‑existing eye conditions.
Most traumatic vitreous hemorrhages clear on their own within a few weeks, especially if the source vessel is small. However, persistent bleeding, a large macular hole, or a retinal detachment will likely need laser photocoagulation, cryotherapy, or pars‑plana vitrectomy.
And remember, your eye isn’t an isolated organ. A head injury can also affect the optic nerve, so watch for double vision, numbness, or headaches that linger beyond the initial impact.
Below is a short video that walks through the anatomy of a blunt eye injury and shows what to look for during an exam.
Take a moment to pause, breathe, and assess your symptoms. If anything feels off, don’t wait – the sooner you get professional care, the better your chances of preserving clear vision.
Risk Factors & Statistics Comparison
You've just woken up to a curtain of red floaters and wonder why your eye decided to throw a party. That uneasy feeling is the first clue that a vitreous hemorrhage is brewing, and the cause behind it can tell you a lot about what to do next. Let's break down the biggest risk factors and see how they stack up against each other.
Broadly, the triggers fall into three buckets: age‑related changes that tug at the retina, systemic diseases that weaken blood vessels, and direct trauma that punches a hole in the eye’s delicate plumbing. Each bucket carries its own odds, warning signs, and follow‑up steps.
Age‑Related Posterior Vitreous Detachment (PVD)
When you hit your late 50s or early 60s, the vitreous gel starts to liquefy and pulls away from the retina. That pull can snap the strongest attachments, especially around the optic disc, leading to a tiny retinal tear and a bleed. In most non‑traumatic cases, PVD‑related tears are the single most common source – think of them as the “default” culprit unless you have another red flag.
Diabetes and Other Neovascular Disorders
High blood sugar turns retinal capillaries into fragile spaghetti; when they sprout new, leaky vessels, any little rupture dumps blood straight into the vitreous. Proliferative diabetic retinopathy alone accounts for a sizable slice of hemorrhages in patients with longstanding diabetes. The same mechanism powers retinal vein occlusions and sickle‑cell retinopathy, so any systemic vascular disease raises your odds. For a deeper dive into how retinal vein occlusions fit into the bigger picture, check out the detailed guide on Vitreous Floaters | Dr Rahul Dubey .
Direct Ocular Trauma
A blunt kick, a stray baseball, or even a hard eye‑rub can transmit enough force to rupture retinal vessels. Unlike the slow pull of PVD, trauma produces an abrupt bleed that often comes with pain, swelling, or a visible bruise. If the impact was high‑speed—think car‑door or a penetrating object—the risk of a large, persistent hemorrhage jumps dramatically.
Macroaneurysm and Choroidal Neovascular Lesions
These are the “quiet neighbors” that break open without warning. A hypertensive retinal macroaneurysm may burst during a blood‑pressure spike, while a choroidal neovascular membrane associated with age‑related macular degeneration can leak directly into the vitreous. Though less common, they tend to produce a denser, often unilateral bleed.
Risk Factor | Typical Scenario | Relative Frequency |
Posterior Vitreous Detachment | Gradual vision change in 55‑70‑year‑olds, sudden floaters | High |
Diabetic/Neovascular Retinopathy | Long‑standing diabetes, new vessels on exam | Moderate‑High |
Ocular Trauma | Blunt impact, sports injury, or penetration | Moderate |
Macroaneurysm / CNV | Hypertension spike or AMD‑related leak | Low‑Moderate |
What does this mean for you? First, note your age and any systemic conditions—those are the biggest clues. Second, ask yourself if you’ve had a recent bump or a blood‑pressure surge. Third, keep a simple log: date of symptom onset, any injury, and your current meds. Bring that list to your retina specialist; it helps the doctor pinpoint the most likely cause and decide whether you need laser, anti‑VEGF injections, or a vitrectomy.
Bottom line: understanding which risk factor is driving your bleed lets you act with confidence. If you spot any red‑flag scenario—especially pain, rapid vision loss, or a recent blow—don’t wait. Schedule an urgent retinal exam and let the data guide the treatment plan.
When to Seek Care and Treatment Options
You've just noticed those red specks drifting across your vision. It feels unsettling, and you start wondering: do I need to call my doctor right now, or can I wait?
First, trust your gut. If you experience sudden vision loss, a painful eye, or a “curtain” that blocks part of your view, treat it like an emergency. Those symptoms often signal a bleed that could worsen without prompt care.
Red‑flag symptoms that demand immediate attention
• Rapid loss of visual acuity (you can’t read a street sign you used to see).
• New flashes of light or a growing shadow in the peripheral vision.
• Eye pain, swelling, or a headache that won't quit.
• Any recent eye trauma, even a seemingly minor bump.
If any of these pop up, call your retina specialist right away or head to the nearest emergency department. Delaying can increase the risk of retinal detachment or permanent vision loss.
How to decide which treatment path fits your situation
When you finally see the specialist, they’ll decide between observation, laser/cryotherapy, anti‑VEGF injections, or pars‑plana vitrectomy. The choice hinges on three factors:
1.Bleed source.A retinal tear usually gets laser sealed; neovascular bleeding often needs anti‑VEGF.
2.Bleed volume.Small, self‑limiting hemorrhages may clear on their own, while dense blood that blocks the visual axis often needs surgery.
3.Underlying health.Diabetes, hypertension, or blood‑thinning meds influence both the cause and the safest intervention.
According to a 2024 review of intra‑ocular hemorrhage cases, retinal tears accounted for 22.4% of vitreous hemorrhage presentations, while diabetic retinopathy made up 34.1% . Those numbers illustrate why pinpointing the cause matters.
Step‑by‑step checklist before your appointment
1.Write down the timeline.Note when the floaters started, any recent injuries, and whether you felt pain or flashes.
2.List your meds.Include blood thinners, aspirin, steroids, and any recent changes.
3.Gather systemic info.Blood‑pressure readings, recent HbA1c results, or any clotting disorders.
4.Prepare visual aids.If you can, take a quick photo of what you see (a phone camera works) to show the doctor.
Bring this cheat sheet to the office. It saves time and helps the retina surgeon map out the most likely cause faster.
What to expect during the visit
The doctor will likely start with indirect ophthalmoscopy and a B‑scan ultrasound if the view is hazy. Optical coherence tomography (OCT) may follow to locate the bleed precisely. If the retina is still attached, they might recommend a short course of observation with head elevation and activity restriction.
When the bleed is persistent, anti‑VEGF injections can shrink new vessels within days. For a tear, laser photocoagulation or cryotherapy seals the break in minutes. If the blood won’t clear or is threatening the macula, pars‑plana vitrectomy removes the vitreous gel and the clot, restoring a clear visual path.
After treatment, expect a follow‑up schedule: weekly checks for the first month, then monthly until the eye stabilizes. Keep your eye elevated while sleeping and avoid heavy lifting, vigorous coughing, or straining for at least two weeks.
And remember, you’re not alone in this. Your retinal surgeon in Sydney—Dr Rahul Dubey—has extensive experience with vitrectomy and macular injections, so you’re in capable hands.
Bottom line: don’t play roulette with your sight. If you notice rapid changes, pain, or a dramatic increase in floaters, act now. A quick call, a clear symptom log, and timely treatment can mean the difference between a temporary nuisance and lasting vision loss.
Conclusion
We've walked through the most common vitreous hemorrhage causes – from a sneaky retinal tear after a posterior vitreous detachment to diabetic neovascular bleeding, trauma, and even macroaneurysms.
So, what does that mean for you? It means you now have a mental checklist: age‑related pull, systemic disease, or an eye injury. Spotting which bucket your situation falls into lets you act fast and get the right treatment.
Remember, early detection is the game‑changer. A quick log of when floaters appeared, any recent bump, and your health numbers can turn a vague worry into a clear conversation with your retina surgeon.
And here's a practical tip: keep your head slightly elevated while you sleep for the first two weeks and steer clear of heavy lifting or intense coughing. Those simple steps buy your eye time to clear minor bleeds.
Ultimately, you control the outcome by staying alert, logging symptoms, and seeking a specialist the moment red specks multiply or vision darken.
If you’re in Sydney and need a trusted retina surgeon, Dr Rahul Dubey is ready to evaluate your case and tailor a plan that fits your lifestyle.
Take action today; the sooner you address the cause, the better your chances of preserving clear vision.
FAQ
What are the most common vitreous hemorrhage causes?
Most people find that a posterior vitreous detachment that tears a retinal vessel tops the list. It’s especially common after age 55 when the gel inside the eye starts to liquefy and pull away. Diabetes‑related neovascular growth is a close second, because those new vessels break easily. Trauma—whether a sports blow or a hard eye‑rub—also shows up frequently, and less often you’ll see macroaneurysms or choroidal lesions spilling blood into the vitreous.
How can I tell if a bleed is from a retinal tear versus diabetic eye disease?
If a retinal tear is the culprit, you’ll often notice a sudden “pop” sensation followed by a cascade of red specks, sometimes with a brief flash of light. The bleed usually settles lower in the eye, so central vision may stay relatively clear at first. Diabetic bleeding tends to produce a denser, more uniform cloud that builds up over days, and you might already have a history of fluctuating blood‑sugar levels or previous eye exams showing new vessels.
Is it possible for a vitreous hemorrhage to clear on its own?
Yes, many small bleeds dissolve without surgery. The eye’s natural cleaning system gradually moves the blood to the lower vitreous, where it can be reabsorbed. Keeping your head slightly elevated while you sleep helps the blood settle away from the central vision, giving your retina a better chance to heal. If the hemorrhage persists beyond a few weeks or blocks your view, your surgeon may suggest a vitrectomy to remove the clot.
What should I do immediately after noticing sudden floaters?
First, stop any activity that raises intra‑ocular pressure—no heavy lifting, intense cardio, or vigorous eye‑rubbing. Then, elevate your head by propping up pillows so the blood drifts down. Write down when the floaters started, any recent injuries, and your current medications. Bring that list to your next retina appointment; it helps the doctor pinpoint the cause faster and decide whether you need laser, injections, or surgery.
Can blood‑thinners increase the risk of a vitreous hemorrhage?
Blood‑thinners definitely tip the balance. Even a minor retinal tear that might have sealed on its own can keep bleeding when you’re on anticoagulants or aspirin. If you’re prescribed these meds, let your eye doctor know right away. They may adjust the dosage temporarily or monitor you more closely with imaging to catch any bleed before it gets too large.
Do lifestyle changes lower my chances of getting a vitreous hemorrhage?
Managing systemic health makes a big difference. Tight glucose control for diabetics, regular blood‑pressure checks, and quitting smoking all reduce the stress on retinal vessels. Staying active—but avoiding sudden, high‑impact sports—keeps the vitreous from jerking too hard. And remember to keep those regular eye exams; catching a tiny tear or early neovascular growth can prevent a full‑blown hemorrhage.
When is surgery the right choice for a vitreous hemorrhage?
Surgery becomes necessary when the blood won’t clear on its own, when it covers the macula (the central part of your vision), or when a retinal detachment is identified. A pars‑plana vitrectomy removes the cloudy gel and lets the surgeon repair any tears or seal leaking vessels. Your surgeon will discuss the risks and benefits, but in most cases the procedure restores vision quickly and prevents long‑term damage.




Comments