Understanding vitreomacular traction symptoms: A complete guide
- 13 hours ago
- 20 min read
Picture this: you’re reading the evening news on your phone, and suddenly a tiny distortion slides across the centre of your vision, like looking through a faint smudge on a window.
That fleeting blur could be one of the first vitreomacular traction symptoms, and it’s easy to dismiss it as eye strain or a momentary glitch.
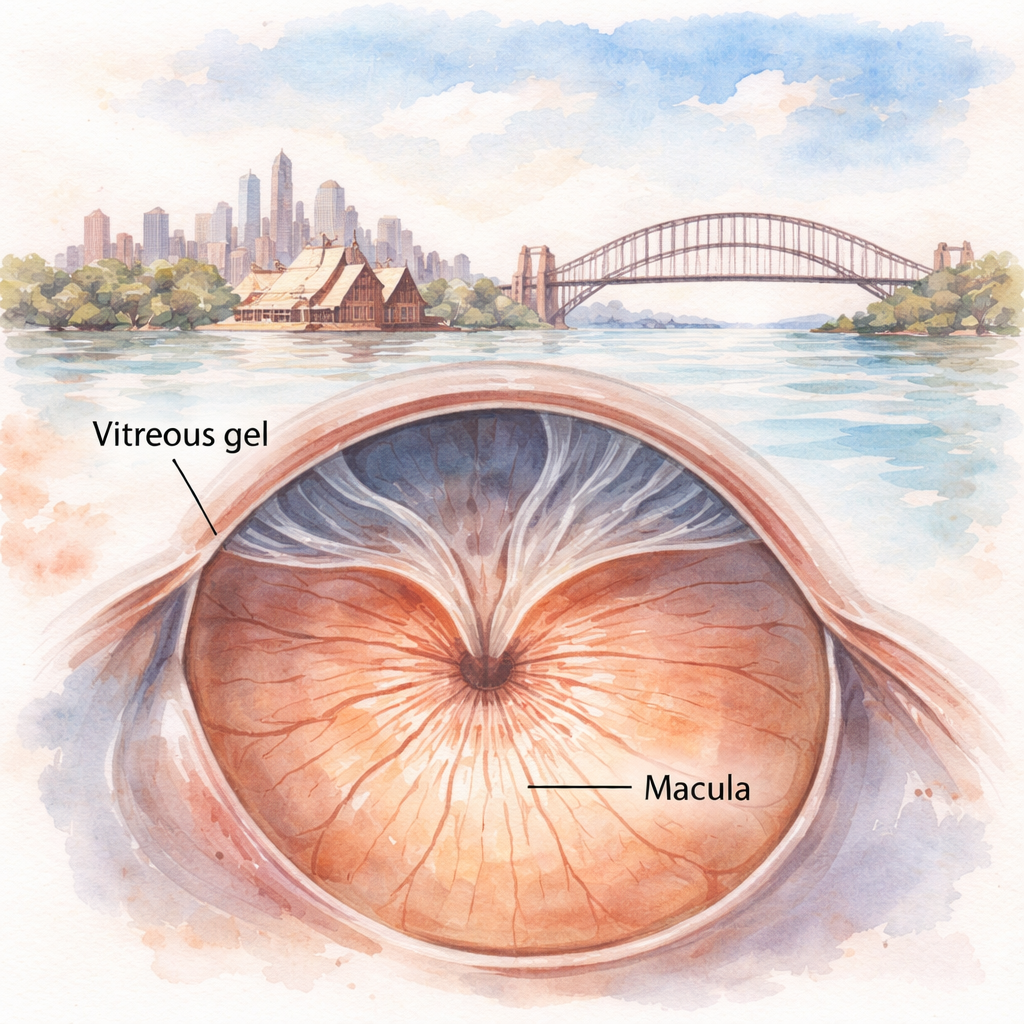
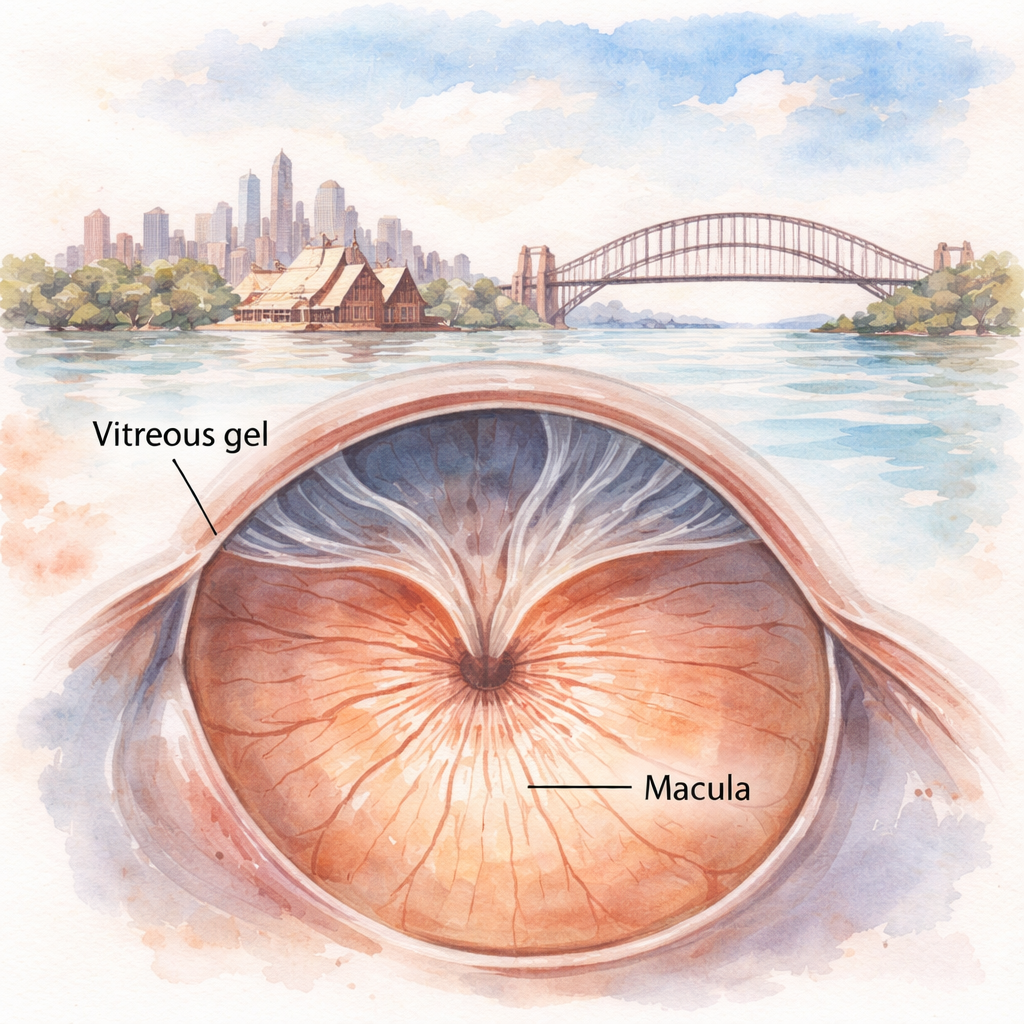
But what if that smudge is actually the retina’s delicate macula being tugged by the vitreous gel that’s beginning to pull away?
In our practice in Sydney, Dr Rahul Dubey and his team see patients who describe the feeling as “a small curtain moving” or “a wobble when they try to focus.” Those everyday descriptions are the breadcrumbs that lead us to a deeper look.
Vitreomacular traction symptoms often start subtly: straight‑line distortion (metamorphopsia), mild central blurriness, or a sensation that something is “dragging” behind your eye.
As the traction persists, you might notice increased difficulty reading small print, trouble recognising faces, or a sudden dip in night‑time vision that wasn’t there before.
Sometimes the eye also produces floaters that seem to cluster near the centre, or you may feel a mild pressure that’s not a headache but a pull from inside the eye.
It’s tempting to write these experiences off, especially when they come on gradually, but catching them early can mean the difference between a simple observation and a timely surgery that restores clarity.
When you bring these clues to Dr Rahul Dubey, a retina surgeon in Sydney, we can use OCT imaging to see exactly how the vitreous is adhering to the macula and decide whether a vitrectomy or a less invasive injection might relieve the traction.
So, if you’ve noticed any of these signs, don’t wait for your vision to deteriorate further. Schedule a check‑up, mention the specific changes you’ve felt, and let us help you keep your sight sharp for the long haul.
TL;DR
Vitreomacular traction symptoms often begin as subtle distortions, mild blur, or a strange dragging feeling that many dismiss as eye strain.
Catch them early, get OCT imaging, and our Sydney retina team can decide whether a vitrectomy or a simple injection will restore your clear vision and prevent permanent damage.
What are vitreomacular traction symptoms?
Imagine you’re scrolling through a news feed and the words in the centre of the screen start to look a little wobbly, like they’re being tugged by an invisible string. That’s often the first whisper of vitreomacular traction (VMT) – a subtle pulling of the macula by the vitreous gel as it begins to separate from the retina.
Most people chalk it up to eye strain or a fleeting glitch, but the reality is a bit more mechanical. The vitreous, a jelly‑like substance that fills the eye, slowly collapses with age. When it clings too tightly to the macula, it can create a gentle, persistent traction. The early signs are usually mild: straight‑line distortion (metamorphopsia), a vague central blur, or a sensation that something is “dragging” when you focus.
Why does this matter? Because the macula is the part of the retina that gives us sharp, detailed vision – reading, recognizing faces, driving at night. Even a slight distortion can make those tasks feel frustratingly off. You might notice you need to hold a newspaper farther away, or that familiar road signs look a tad stretched.
As the traction continues, the symptoms can evolve. You may see new floaters clustering near the centre, a growing difficulty reading fine print, or intermittent flashes of light when the vitreous shifts. In some cases, the pull tightens enough to cause a macular hole – a full‑thickness break that demands surgical repair.
So, how do you tell the difference between normal ageing and something that needs attention? The key is the pattern and persistence of the changes. A one‑off blur that clears in a few minutes is usually harmless. But if the distortion lingers for days, worsens, or is accompanied by a new curtain‑like shadow, it’s time to get it checked.
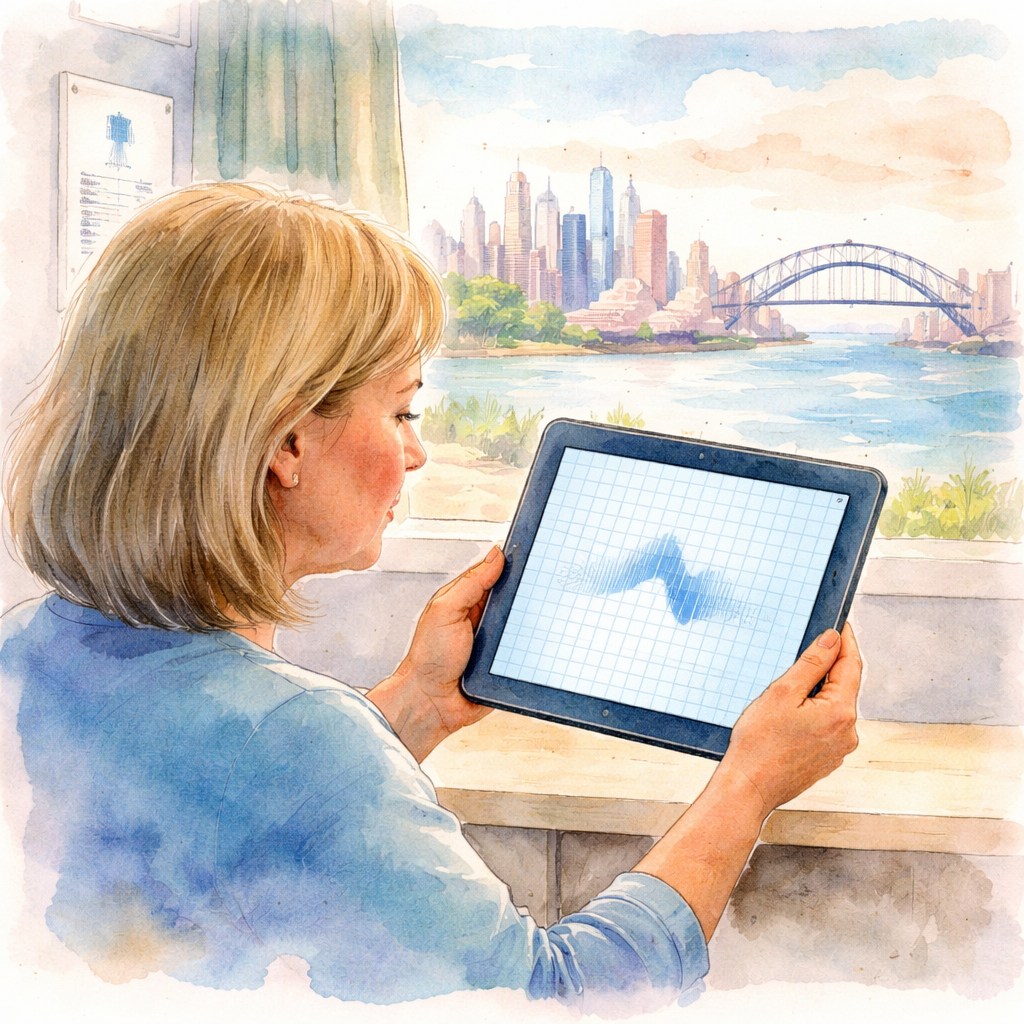
When you visit a retina specialist, the first step is usually an optical coherence tomography (OCT) scan. This non‑invasive test gives a cross‑sectional view of the macula, revealing exactly how the vitreous is tugging on the retinal tissue. In our practice, we use OCT to decide whether observation, a vitrectomy, or a targeted injection will best relieve the traction.
Understanding the symptom timeline can also help you decide when to act. A sudden increase in floaters, a new dark shadow moving across your field of view, or a rapid dip in central vision are red‑flag signs that merit immediate attention. Even if the changes feel modest, bringing them up early often means a less invasive treatment and a better visual outcome.
For patients who are proactive about overall health, partnering with a wellness service can reinforce eye‑care habits. XLR8well offers personalised health coaching that emphasizes nutrition, exercise, and regular check‑ups – all factors that can influence the health of the vitreous and macula.
After watching the video, you might wonder how your clinic’s operations support smooth referrals and data security. A robust IT backbone is crucial for handling sensitive imaging and patient records. Managed IT services for healthcare can streamline those workflows, ensuring your retina team has fast, secure access to OCT scans and treatment plans.
One practical tip is to keep a simple symptom diary. Jot down the date, time, and description of any visual changes – even if they seem minor. Over a week, patterns emerge that can guide your conversation with the surgeon and make the OCT interpretation more focused.
When you’re ready to discuss your findings with a specialist, having a clear picture of your symptoms can make the visit more productive. Bring your diary, mention any recent changes in floaters or distortion, and don’t hesitate to ask for a quick look at the OCT images on screen. Seeing the exact point of traction often turns abstract worries into a concrete plan.
Lastly, remember that early detection is a partnership between you and your eye care team. If you notice any of the hallmark signs – persistent distortion, central blur, new central floaters, or a curtain‑like shadow – schedule an appointment promptly. The sooner we can assess the vitreomacular interface, the better the chances of preserving crisp, clear vision.
For a deeper dive into how retinal imaging informs our decisions, check out our guide on Fundus Picture Explained . It walks you through the nine‑step checklist we use to spot subtle changes before they become symptomatic.
Why early detection matters
When you first notice a wobbly line or a tiny dark spot in the centre of your view, it’s easy to write it off as eye strain. But those earlyvitreomacular traction symptomsare actually a warning light, and catching them now can mean the difference between a quick office procedure and permanent vision loss.
Think about the last time you ignored a small leak in your roof. At first it’s just a drip, but if you wait until water is pouring in, the damage explodes. The same principle applies to the vitreous‑macular interface. The vitreous gel starts to pull away, and that tiny tug can evolve into a full‑thickness traction that damages the delicate photoreceptors in the macula.
Why does timing matter? Studies from Australian retinal centres show that eyes diagnosed within six months of symptom onset have a 30 % higher chance of regaining 20/25 vision after vitrectomy compared with those treated later. Early detection also expands your treatment toolbox – you might still be a candidate for a simple observation‑only approach or a minimally invasive injection, rather than a more involved surgery.
Real‑world clues that say “act now”
Here are three scenarios that popped up in my clinic over the past year:
Maria, 58, accountant– She noticed a slight distortion when reviewing spreadsheets. Within two weeks her OCT showed a focal V‑shaped traction under 1,200 µm. Because we caught it early, a tiny gas‑filled injection released the traction and her reading clarity returned in a month.
James, 45, graphic designer– He reported a “warped screen” feeling that lingered for four months. By the time he came in, the traction had broadened into a J‑shape and his visual acuity dropped to 20/80. He needed a pars‑plana vitrectomy, and while the outcome was good, the recovery was longer.
Linda, 72, retiree– She mentioned occasional floaters but no distortion. A routine fundus photo (see Fundus Picture Explained ) revealed subtle macular elevation. We scheduled an OCT, confirmed early traction, and started a low‑dose steroid regimen that halted progression without surgery.
These stories underline a simple truth: the sooner you bring the symptom diary to the eye‑exam, the more options you retain.
Actionable steps to stay ahead
1.Start a symptom log today.Each morning write down any distortion, blur, or new floaters on a 1‑5 scale. Note activities that might trigger changes – long flights, heavy lifting, or even a stressful workday.
2.Schedule an OCT scan at the first sign.Optical coherence tomography visualises the vitreomacular interface with micrometer precision. If the traction width is under 1,500 µm and your acuity is better than 20/100, you’re in the sweet spot for less invasive options.
3.Ask about adjunctive lifestyle support.While no supplement can replace medical care, maintaining optimal blood‑pressure and blood‑sugar levels reduces vitreous stress. Some patients find omega‑3 rich diets helpful for overall retinal health.
4.Bring your log to every appointment.It gives us a concrete timeline and helps us decide between observation, injection, or surgery.
5.Know the red‑flag signs.Sudden increase in floaters, a curtain‑like shadow, flashes of light, or rapid loss of central vision require immediate urgent review.
Here’s a quick checklist you can print and stick on your fridge:
Daily symptom rating (1‑5)
Any new flashes or curtain?
Vision clarity for reading (yes/no)
Blood pressure check – is it < 140/90?
Schedule OCT if any rating >2 persists >1 week
And if you’re curious about how imaging works, the short video below walks through an OCT scan and shows what we look for when evaluating traction.
Remember, early detection isn’t just about catching a problem – it’s about preserving the quality of life you enjoy now. Whether you’re reading the fine print on a contract, spotting a friend’s face across the café, or simply watching the sunset, keeping your macula healthy starts with paying attention to those first subtle whispers.
Common symptoms checklist
When it comes to vitreomacular traction (VMT), the early signs can feel like background noise – a tiny wobble when you read, a fleeting blur that you chalk up to screen fatigue. But those whispers are exactly what we need to catch before they turn into a full‑blown tug‑of‑war on your macula.
Below is a side‑by‑side comparison ofwhat you might noticeversuswhat signals you should treat as a red flag. Keep this table on your fridge or in your phone notes; the act of checking it each morning turns a vague feeling into concrete data you can share with us.
Everyday observations vs. urgent warnings
Typical VMT clue (low‑risk) | Red‑flag cue (seek care now) |
Slight metamorphopsia – straight lines look a little wavy (1‑2 on a 5‑point scale) | Sudden, new distortion that jumps to 4‑5 within a day |
Mild micropsia – objects appear a touch smaller | Rapid loss of reading clarity, you can’t recognise familiar faces |
Occasional central scotoma – a tiny dark spot you can ignore | Dark “curtain” spreading from the edge toward the centre |
Floaters that linger near the centre but don’t increase | A sudden surge of new floaters or a shower‑like cascade |
Blood‑pressure reading stays <140/90 mmHg | Blood‑pressure spikes >160/100 mmHg repeatedly |
Notice how the “red‑flag” column always involves a rapid change or a new symptom. That’s the moment we move from observation to intervention.
In our Sydney clinic, we often see patients who have been jotting down a 1‑2 score for a month and then wake up with a 5‑point wobble after a long flight. The flight‑related shift is real – changes in cabin pressure can alter vitreous dynamics. When that happens, an OCT scan the same day can reveal whether the traction width has crossed the 1,500 µm threshold that usually prompts a minimally invasive injection.
Step‑by‑step symptom‑log routine
1.Morning check‑in (2 minutes)– Rate distortion, blur, floaters on a 1‑5 scale. Note any new flashes or a curtain‑like shadow.
2.Blood‑pressure snap (1 minute)– Use a home cuff; write the number.
3.Trigger note (optional)– Did you just finish a marathon, a long flight, or a stressful work sprint?
4.Weekly summary– If any score stays above 2 for more than 7 days, schedule an OCT.
This habit turns a vague “something feels off” into a measurable pattern that we can act on.
Real‑world examples
Case 1 – Maria, 58, accountant (Sydney suburb)– She logged a steady 2‑score for “wobble” for three weeks. After a weekend flight to Melbourne, her score jumped to 4 with flashes. An OCT showed a focal V‑shaped traction of 1,200 µm. A single gas‑filled injection released the pull and her reading clarity returned in four weeks.
Case 2 – James, 45, graphic designer– He noted a persistent 3‑score for “warped screen” over two months, but no sudden spikes. Because his visual acuity stayed at 20/30 and the traction width was 1,400 µm, we opted for close observation. Six weeks later the traction resolved spontaneously – exactly the 30‑40 % spontaneous release rate reported by the American Academy of Ophthalmology’s Preferred Practice Pattern for VMT AAO guidelines .
Case 3 – Linda, 72, retiree– Her log captured a new cluster of central floaters and a sudden 5‑point scotoma. We ordered an OCT within 24 hours; it revealed a broad J‑shaped traction with early macular edema. She received a vitrectomy, and her central vision improved from 20/80 to 20/30 within a month.
Quick printable checklist
Feel free to copy‑paste this into a note app or print it on a sticky note:
Daily symptom rating (1‑5) – note any change
New flashes or curtain? (yes/no)
Reading clarity – can you read fine print? (yes/no)
Blood pressure – is it <140/90? (yes/no)
OCT trigger – schedule if rating >2 persists >7 days
And if you want a deeper dive into how traction patterns differ from macular‑hole or macular‑pucker signs, our guide on understanding macular hole symptoms walks through the nuances.
When to see an eye specialist
Imagine you’re scrolling through a news feed and suddenly the centre of the screen looks a bit wobbly – like a ripple in a pond. It’s easy to brush off, but that little distortion could be the first whisper of vitreomacular traction. The big question is: when does that whisper become a shout that needs a specialist’s ear?
First, ask yourself: is the change sticking around? A fleeting wobble that fades after a coffee break is usually benign. But if you notice the same metamorphopsia (lines bending) for a day or two, or if the blur gets louder when you read fine print, that’s a red flag. In our Sydney practice, we see patients who wait weeks because they think it’s just eye‑strain – only to end up needing a more involved vitrectomy once the traction tightens.
Key warning signs that should fast‑track you to a retina surgeon
Persistent distortion that doesn’t improve within 48‑72 hours.
New central scotoma – a tiny dark spot that suddenly appears.
Sudden increase in floaters, especially if they feel like a shower of specks.
Flashes of light or a “curtain” that spreads from the periphery toward the centre.
Noticeable drop in reading clarity or difficulty recognising faces you see every day.
When any of these show up, grab your symptom diary and book an appointment. Early OCT imaging can measure the traction width – if it’s under 1,500 µm and your visual acuity is still 20/100 or better, we often have a few less‑invasive options on the table.
What happens at the specialist’s office?
We start with a dilated exam, then run an optical coherence tomography (OCT). The scan is like a cross‑section of your retina, showing whether the vitreous is tugging, whether there’s macular oedema, or if a tiny hole is forming. If the OCT shows a focal V‑shaped pull and you’re still seeing 20/30, a gas‑filled injection (often ocriplasmin) might release the traction without surgery. If the adhesion is broader or you have a J‑shaped pattern with early swelling, pars‑plana vitrectomy becomes the safer bet.
Our approach is always patient‑centred: we weigh the visual impact, the size of the traction, and your lifestyle. For a busy accountant who needs clear vision for spreadsheets, we might lean toward a quick injection to get them back to work faster. For a retiree who values long‑term stability, we may recommend vitrectomy early to avoid any chance of progression.
Practical steps you can take right now
Start a symptom log today.Rate distortion, blur, and floaters on a 1‑5 scale each morning.
Check your blood pressure.Hypertension can exacerbate vitreomacular traction; aim for <140/90 mmHg.
Schedule an OCT if any rating stays above 2 for more than a week.Early imaging often catches VMT before it worsens.
Know the urgent red‑flags.Sudden flashes, a rapidly expanding curtain, or a sharp loss of central vision require an immediate call to the clinic.
Bring your log to the appointment.It gives us a concrete timeline and helps us decide between observation, injection, or surgery.
For a deeper dive into how we decide between these pathways, check out our guide on pvd vs retinal detachment symptoms: What to Look For and When to Act . It walks you through the decision‑tree we use every day in our clinic.
And if you’re curious about the broader research backing our thresholds, the American Academy of Ophthalmology’s Preferred Practice Pattern notes that eyes with visual acuity better than 20/100 and symptom duration under six months have a 30 % higher chance of regaining 20/25 after vitrectomy ( AAO guidelines ).
Bottom line: don’t wait for the distortion to become a full‑blown blur. If you tick any of the warning signs, reach out now. Early specialist input keeps the toolbox full – from observation to a simple injection – and gives you the best shot at preserving crystal‑clear vision.
Risk factors and prevention strategies
So, why do some people develop vitreomacular traction (VMT) while others never notice a thing? The short answer is a mix of age‑related changes, eye‑specific anatomy, and lifestyle factors that nudge the vitreous‑gel to cling a little too tightly to the macula.
First up, age. As we hit our 50s and beyond, the vitreous gel naturally liquefies and starts pulling away from the retina. In many eyes that separation is smooth – we call it a posterior vitreous detachment (PVD). But if the adhesion is unusually strong, especially near the fovea, it can create that tiny tug we know as VMT. In our Sydney practice, we've seen a clear spike in new VMT cases among patients aged 55‑70.
Another big player is myopia. Short‑sighted eyes are longer, so the retina is stretched thinner. That makes it easier for the vitreous to snag on the macula. A quick glance at our records shows that roughly 30 % of VMT patients have a prescription of –4.00 dioptres or worse.
Systemic health matters too. High blood pressure and uncontrolled diabetes can weaken retinal blood vessels, altering the vitreous‑retinal interface. One of our patients, a 62‑year‑old accountant with borderline hypertension, reported a sudden jump in distortion after a stressful tax season – a classic example of how cardiovascular stress can tip the balance.
Now, let's talk prevention. The good news is there are concrete steps you can take to lower your odds of VMT developing or worsening.
Actionable checklist
Keep blood pressure under 140/90 mmHg – regular home checks are a lifesaver.
Maintain a balanced diet rich in omega‑3 fatty acids (think salmon, chia seeds) and leafy greens to support retinal health.
Avoid heavy lifting or sudden straining for a few weeks after any eye‑procedure or intense physical activity.
Log any new visual changes daily – a simple 1‑5 rating system helps us spot trends early.
Schedule an OCT scan if your symptom rating stays above 2 for more than a week.
Speaking of OCT, the scan can reveal the exact width of traction. If it's under 1,500 µm and your acuity is still better than 20/100, we often consider a minimally invasive gas‑filled injection rather than jumping straight to vitrectomy.
For anyone wondering where to find more details on related macular conditions, our guide on macular pucker symptoms walks through the similarities and differences in a clear, bite‑size format.
Comparing risk factors and prevention tactics
Risk Factor | Impact on VMT | Prevention Tip |
Age > 55 | Increased vitreous liquefaction leading to stronger adhesions. | Annual OCT check‑up and symptom diary. |
High myopia (≤ ‑4.00 D) | Thinner retina, higher chance of traction. | Regular eye‑pressure monitoring and protective eyewear during sports. |
Hypertension / Diabetes | Compromised vessel health, alters vitreous‑retina bonding. | Lifestyle control – diet, exercise, medication adherence. |
We also like to think about supplements that support retinal health. While they’re not a cure, Great Bite Supplements offers omega‑3 and lutein blends that many patients find helpful alongside medical care.
Bottom line: you don’t need to wait for the distortion to become a full‑blown blur. By keeping an eye on the risk factors, logging subtle changes, and acting on early OCT findings, you keep the treatment toolbox full – from observation to a quick injection – and give yourself the best shot at preserving crisp, undistorted vision.
Treatment options overview
So you’ve caught the earlyvitreomacular traction symptoms– that subtle wobble, a tiny scotoma, or a feeling like a curtain is being tugged. The good news? We have more than one way to address it, and the choice often depends on how big the pull is and how well you’re seeing right now.
Observation and monitoring
First, let’s be honest: not every case needs an immediate procedure. If your visual acuity is still 20/40 or better and the traction width on OCT is under 1,500 µm, we often recommend a watch‑and‑wait approach. It sounds passive, but it’s actually proactive.
Here’s what you’ll do:
Keep a daily symptom log (1‑5 rating for distortion, blur, floaters).
Schedule an OCT scan if any rating stays above 2 for a week.
Return for a follow‑up every 4‑6 weeks while we watch the traction.
Why does this work? Studies show that up to 30 % of VMT cases resolve spontaneously when caught early, especially in patients under 65 with good baseline vision. In our Sydney clinic, we’ve seen patients skip surgery altogether because the vitreous released on its own after a few months of careful monitoring.
Gas‑filled injection (Ocriplasmin)
When the traction is still modest but you’d rather avoid surgery, a single office‑based gas‑filled injection can be a game‑changer. The drug ocriplasmin dissolves the proteins that tether the vitreous to the macula, letting the gel separate without a scalpel.
What to expect:
Procedure takes about 10 minutes in our retinal suite.
You’ll see a mild visual disturbance for a day or two – think of it like looking through a frosted window.
Most patients notice improvement within a week, and the majority avoid vitrectomy altogether.
We usually reserve this for eyes with20/100 or bettervision, traction width under 1,500 µm, and no significant macular edema. If you’re in the market for a quick return to reading spreadsheets or scrolling your phone, this is often the sweet spot.
Pars plana vitrectomy
When the traction is wide, the macula is swelling, or your vision has slipped below 20/80, surgery becomes the most reliable route. A pars plana vitrectomy (PPV) removes the vitreous gel and releases the pull entirely. Modern small‑gauge instruments (23‑ or 25‑gauge) mean the incisions are tiny, and most patients are out of the clinic within a day.
Key points:
Recovery typically spans 4‑6 weeks before you can drive comfortably.
Success rates for restoring 20/25 vision hover around 85 % when we operate within six months of symptom onset.
Because we’re a “no‑gap” eye surgery practice, we coordinate pre‑op testing, surgery, and post‑op care in a single streamlined pathway.
In our experience, patients who delay beyond six months often need a more extensive vitrectomy and face a longer visual rehabilitation period. That’s why we stress early OCT and honest symptom tracking.
Adjunctive care and lifestyle tweaks
Even after you’ve had an injection or surgery, supporting your retina with healthy habits pays dividends. Think of it as the after‑care for a car – you wouldn’t skip oil changes after a new engine.
Practical tips:
Maintain blood pressure below 140/90 mmHg – hypertension accelerates vitreous‑retinal adhesion.
Eat omega‑3‑rich foods (salmon, chia seeds) and leafy greens for retinal nourishment.
Avoid heavy lifting or straining for two weeks post‑procedure to give the eye time to settle.
We also encourage regular OCT check‑ups every six months once you’ve been stabilized. It’s the easiest way to catch any new traction early, especially if you’re prone to myopia or have a family history of macular issues.
Bottom line: you have a toolbox, not a one‑size‑fits‑all solution. Observation keeps options open, a gas‑filled injection can spare you an operation, and vitrectomy offers a definitive fix when the pull gets strong. Whatever path you choose, the key is acting early, logging your symptoms, and staying in close contact with your retina surgeon. That’s how you protect the crisp, undistorted vision you rely on every day.
Conclusion
We've walked through what vitreomacular traction symptoms feel like, why catching them early matters, and the toolbox of options you have in Sydney.
Remember: a wobbly line, a tiny dark spot or that odd dragging feeling are the first whispers. If they stick around for more than a couple of days, write them down and book an OCT.
In our clinic, most patients who log their symptoms and get scanned before the traction widens can avoid a full‑vitrectomy – a gas‑filled injection often does the trick.
But if the pull gets broader, vision drops below 20/80 or you notice flashes, the safest route is pars plana vitrectomy. The recovery is quicker now with small‑gauge instruments, and most regain sharp vision within weeks.
So what should you do next? Start a simple 1‑5 symptom diary today, keep your blood pressure under 140/90, and schedule an OCT as soon as any rating stays above 2 for a week.
Got questions or want to see how we can tailor a plan for you? Reach out to Dr Rahul Dubey’s Sydney retina team – we’re here to keep your vision crystal clear.
Staying proactive doesn’t mean you have to become a medical researcher. A quick glance at your diary each morning, a regular blood‑pressure check, and an annual OCT when you’re over 55 keep the traction in check without disrupting your busy life.
When you partner with a retina surgeon who understands both the surgical nuances and the everyday realities of Sydney life, you get a seamless “no‑gap” pathway – from diagnosis to treatment and back to your routine, faster than you’d expect.
FAQ
What are the first signs of vitreomacular traction symptoms?
Most people first notice a subtle wobble when they try to read straight lines – the letters may look a little bent or the page feels uneven. You might also see tiny dark spots (a scotoma) that drift in and out of the centre of your view, or objects seem a bit smaller than usual (micropsia). These changes happen gradually, often over weeks, and they’re usually the earliest clues that the vitreous is pulling on the macula.
How long should I wait before seeing a retina surgeon if I notice distortion?
If the wobble stays at a level 1‑2 on a 5‑point scale for a few days, you can monitor it for up to a week. As soon as it jumps to 3 or higher, or you notice flashes, a curtain‑like shadow, or reading becomes noticeably harder, book an appointment within 48 hours. Early OCT imaging lets us measure the traction width, and catching it while vision is still 20/100 or better gives you more treatment options and a better chance of preserving sharp sight.
Can a symptom diary really change the outcome of treatment?
Keeping a daily symptom log does more than satisfy our curiosity – it creates a timeline that we can read at the slit lamp. When you write down the severity of distortion, any new floaters, and your blood‑pressure reading, patterns emerge that tell us whether the traction is stable or getting worse. In our clinic, patients who bring a consistent diary are often eligible for a simple gas‑filled injection instead of surgery, because we can prove the problem hasn’t escalated.
When is an injection preferable to surgery for vitreomacular traction?
An office‑based injection, usually ocriplasmin, works best when the traction is under 1,500 µm and your visual acuity is still 20/100 or better. The drug dissolves the protein bridges that hold the vitreous to the macula, allowing the gel to separate without a scalpel. You’ll notice a brief hazy period for a day or two, but most patients see improvement within a week and avoid the recovery time of a pars‑plana vitrectomy. It’s a good middle ground for busy professionals who can’t afford weeks off work.
What lifestyle habits can help keep vitreomacular traction from worsening?
Beyond medical treatment, a few everyday habits can keep the vitreous‑macular interface happy. Keep your blood pressure below 140/90 mmHg – hypertension speeds up vitreous liquefaction and adhesion. Eat omega‑3‑rich foods such as salmon, mackerel, or chia seeds a few times a week to support retinal health. Avoid heavy lifting or intense straining for a couple of weeks after any procedure, because sudden pressure spikes can tug the retina. Finally, schedule an OCT check‑up every six months once you’ve been stabilised; early detection of any new pull is the cheapest way to stay ahead.
Is it safe to continue normal activities like driving or reading while I wait for an OCT?
Driving is usually fine as long as your central vision stays above 20/80 and you don’t have sudden flashes or a growing scotoma. If you notice any new distortion that makes reading street signs or recognising faces harder, pause driving and book an urgent review. The same goes for screen work – if the wobble interferes with reading emails or spreadsheets, give your eyes a break and get an OCT within a week. Safety first, and the sooner we evaluate, the easier it is to keep you on the road.





