Understanding Floaters After Retinal Detachment Surgery: A Practical Guide
- 2 days ago
- 16 min read
Imagine waking up after retinal detachment surgery and noticing tiny specks dancing across your vision, like dust motes in a sunbeam. That moment can feel unsettling, especially when you’ve just spent weeks worrying about saving your sight.
Those specks are what we call floaters – tiny shadows cast by clumps of vitreous gel that drift in front of the retina. After a vitrectomy or scleral buckle, it’s normal for some patients to notice an increase in floaters as the eye heals and the vitreous shifts.
Take Sarah, a 58‑year‑old teacher from Sydney who had surgery last month. She described the floaters as “tiny black bugs that never leave me alone.” At first she panicked, thinking the surgery had failed, but after a quick review we reassured her that this is a common post‑operative phenomenon.
Why do they appear? The surgical manipulation can cause the vitreous to liquefy and separate, allowing microscopic fibers to float freely. In some cases, residual vitreous strands or tiny blood cells create the shadows you see. For a deeper dive into what’s actually moving around in your eye, check out our Vitreous Floaters page.
Here’s what you can do right now: 1) Keep a symptom diary – note when the floaters are most noticeable, whether they’re static or moving. 2) Protect your eyes from sudden pressure changes; avoid heavy lifting or intense bending for the first two weeks. 3) Schedule a follow‑up appointment within 4–6 weeks so we can examine the retina with OCT and ensure nothing unusual is developing.
While floaters are usually harmless, watch for red flags: a sudden surge in number, new flashes of light, or a shadow across your visual field. Those could signal a fresh detachment and need urgent attention.
Finally, a few everyday habits can make the experience less irritating. Staying well‑hydrated helps maintain vitreous consistency, and a diet rich in omega‑3 fatty acids supports overall retinal health. Simple eye‑relaxation exercises – like the “20‑20‑20” rule when using screens – can reduce eye strain, which sometimes amplifies the perception of floaters.
Bottom line: floaters after retinal detachment surgery are common, often temporary, and usually manageable with careful monitoring and a few lifestyle tweaks. If you’re uncertain, give us a call – we’re here to guide you through every stage of recovery.
TL;DR
Floaters after retinal detachment surgery are common and usually harmless, but they can feel unsettling as specks dance across your vision during recovery.
Track them with a simple diary, stay hydrated, avoid sudden pressure changes, and contact us promptly if you notice flashes or a shadow, so you can focus on healing without unnecessary worry.
Step 1: Recognize New Floaters
When you first open your eyes after retinal detachment surgery, the world can feel a little different. Maybe you notice tiny specks drifting across your vision, like dust motes caught in a shaft of sunlight. That moment can be unsettling – you wonder if it’s just normal healing or something you need to worry about.
First, give yourself permission to pause and look. Ask yourself: "Do these floaters feel new, or have they been there before the surgery?" If they’re brand‑new, that’s a clue they’re related to the recent procedure. New floaters often appear because the vitreous gel shifts as it re‑settles after the eye has been manipulated.
Here’s a quick way to tell if they’re truly new:
Notice the timing. Floaters that show up within the first two weeks post‑op are usually linked to the surgical healing process.
Check the shape. Fresh floaters tend to be small, dark, and move with eye motion – think of them as tiny shadows rather than solid blobs.
Observe movement. If they glide smoothly when you look left or right, they’re likely harmless vitreous strands.
Now, let’s get practical. Grab a small notebook or use the notes app on your phone. Every time you spot a floater, jot down the time of day, what you were doing, and how many you saw. This simple diary becomes your personal radar, helping you and your surgeon spot patterns.
Does this feel like extra work? Not really. It takes less than a minute, and over a week you’ll have a clear picture of whether the floaters are fading, staying steady, or suddenly multiplying.
And remember, you’re not alone in this. Many of our patients in Sydney have told us that simply tracking the specks eases anxiety – they stop wondering "is this a problem?" and start seeing it as part of the normal healing journey.
One tip that often gets overlooked: keep the lighting soft when you first notice floaters. Bright glare can make them look more prominent. Dim the room a bit, give your eyes a chance to settle, and you’ll get a more accurate sense of what you’re seeing.
So, what’s the next move after you’ve logged a few entries?
Take a moment to compare today’s notes with yesterday’s. If the number of floaters is staying the same or slowly decreasing, you’re likely on track. If you notice a sudden surge, especially accompanied by flashes of light or a shadow across your vision, that’s a red flag – call us right away.
We’ll look at your diary together at your follow‑up appointment and decide if any extra imaging, like OCT, is needed.
Below is a short video that walks you through how to set up a quick floaters diary on your phone. It’s a visual guide that takes less than two minutes.
After you’ve watched the video, try the diary exercise tonight before bed. You’ll be surprised how quickly the habit forms.
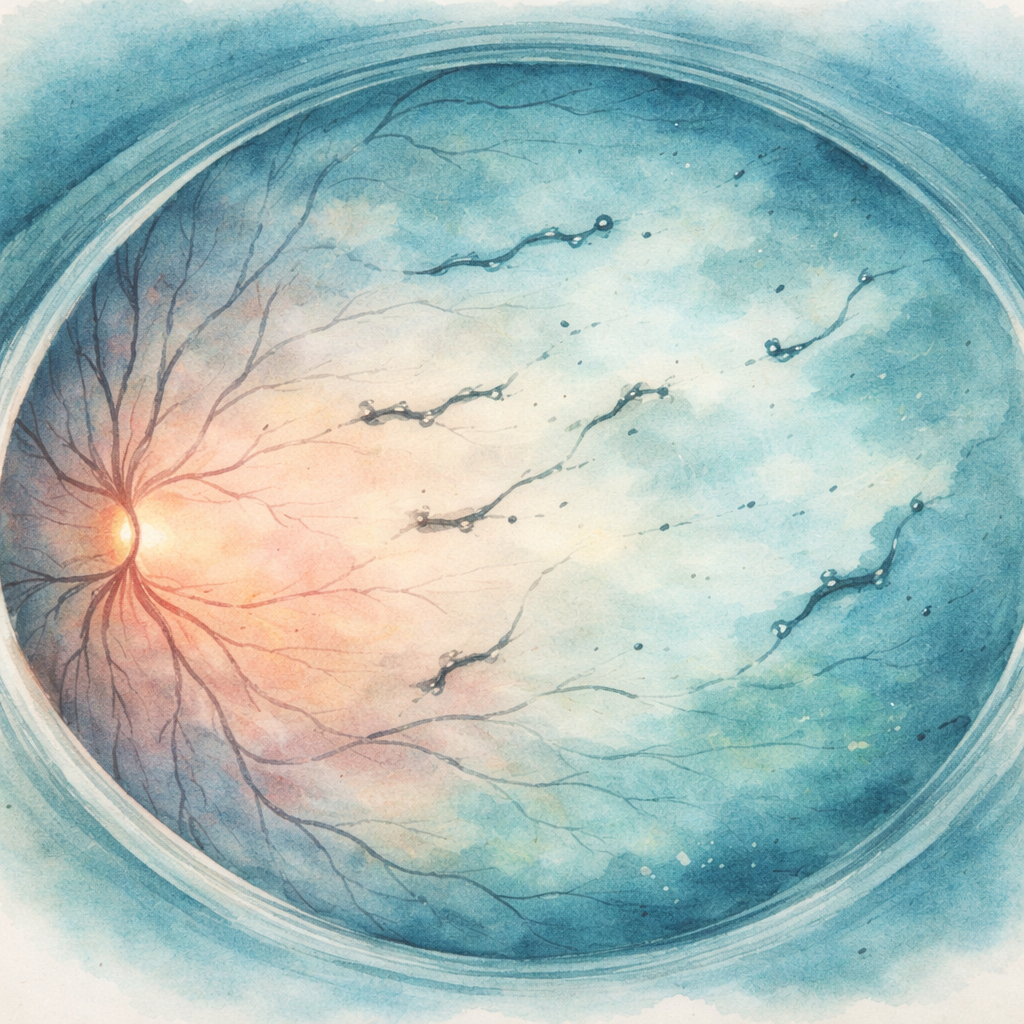
Finally, here’s a visual reminder you can keep on your nightstand: a gentle watercolor illustration of the eye’s interior, highlighting how vitreous strands float after surgery.
Step 2: Assess Their Impact
Now that you’ve spotted a new floater, the next question is: does it matter? Not every speck signals trouble, but some do. The key is to gauge how the floater is affecting your vision and your daily life.
First, notice whether the floaters are static or shifting. A handful that drift lazily with eye movement is usually benign. A swarm that flutters rapidly, especially when you look to the side, can mean the vitreous is pulling harder on the retina.
Second, ask yourself if you’re seeing any extra symptoms. Flashes of light, a curtain‑like shadow, or a sudden loss of peripheral vision are red flags. In our clinic we’ve seen patients who ignored a flash and ended up needing a second surgery. That’s why we stress prompt reporting.
Here’s a quick three‑point checklist you can run through each day:
Movement speed:Slow and steady vs. quick darting.
Quantity change:Same handful or a sudden surge?
Associated sensations:Any flashes, shadows, or blurry spots?
If you tick any of the bold boxes, it’s time to call us. In our experience, early detection saves vision and often avoids a more invasive procedure.
Let’s break down the impact categories with a simple table. This will help you decide whether to watch, act, or seek urgent care.
Impact Factor | What to Look For | Suggested Action |
Low | One or two static floaters, no flashes, no vision loss | Log in diary, monitor for 1‑2 weeks |
Moderate | Increasing number, mild movement, occasional light flashes | Schedule a routine follow‑up within a week |
High | Rapid‑moving swarm, new flashes, curtain‑like shadow, sudden peripheral loss | Call the clinic immediately; urgent OCT exam may be needed |
Real‑world example: Jane, a 62‑year‑old accountant from Bondi, noticed a cluster of floaters two weeks after her vitrectomy. She also saw occasional sparks of light when she stood up quickly. She called us, and we performed an OCT scan that revealed a tiny retinal tear. A quick laser retinopexy sealed it, and Jane’s vision stayed stable.
Contrast that with Mark, a 55‑year‑old builder who saw a single speck and shrugged it off. Six weeks later he reported a shadow across his visual field. By then the detachment had progressed, requiring a more complex surgery. The difference? Early impact assessment.
Another tip: use a bright background—like a clear sky or a white wall—to spot floaters more clearly. Turn on a lamp and look straight ahead; the specks become more visible against the uniform light. This simple trick helped many of our patients differentiate harmless floaters from those that move with the vitreous.
What about lifestyle? Heavy lifting, bending, or sudden changes in intra‑ocular pressure can aggravate floaters. If you notice an uptick after a workout, pause the activity and re‑evaluate. Staying hydrated and maintaining a diet rich in omega‑3s supports vitreous health, but it won’t replace a proper clinical check.
Finally, if you want a deeper dive into how to differentiate posterior vitreous detachment from a retinal detachment, our PVD vs retinal detachment symptoms guide walks you through the signs step by step.
Bottom line: assessing impact is about pattern‑recognition and timing. Keep an eye on movement, quantity, and accompanying flashes. Log what you see, act on red flags, and let us know when you’re unsure. Your vision is worth that extra minute of attention.
Step 3: When to Seek Professional Help
You've logged your floaters, you know what they look like, and you've checked how they affect your daily routine. The next question is simple but crucial: when do you pick up the phone and call the clinic?
First, trust the red‑flag checklist you already have. If you notice any of these, treat them as urgent:
Sudden increase in the number of floaters – a “shower” of specks rather than the usual handful.
Flashes of light that appear out of nowhere, especially in peripheral vision.
A curtain‑like shadow moving across part of your view.
Pain, pressure, or a noticeable drop in visual acuity.
When any one of those pops up, book an urgent appointment. In our Sydney practice, we typically see patients within 24‑48 hours for these signs, because early intervention can mean the difference between a quick laser seal and a more involved surgery.
Step‑by‑step: How to act fast
1.Pause your day.Stop what you’re doing, especially any heavy lifting or vigorous exercise, and sit somewhere comfortable.
2.Document the change.Write the exact time you first saw the new floaters or flashes, and note any accompanying symptoms. A photo of your visual field isn’t possible, but a quick note helps the surgeon triage you.
3.Call the clinic.Use the after‑hours line if it’s outside normal office hours. Mention the red‑flag symptoms verbatim – “I’ve suddenly got a lot more floaters and a brief flash in my right eye.”
4.Follow the nurse’s instructions.They may ask you to avoid certain activities (like bending over) until you’re seen. They’ll also schedule you for a dilated retinal exam and possibly an OCT scan.
5.Prepare for the visit.Bring your symptom diary, any eye‑drop bottles you’re using, and a list of recent medications. If you’ve had a recent YAG capsulotomy or any other eye procedure, let the team know – that context can change the urgency.
Real‑world scenarios
Take Liam, a 61‑year‑old accountant from Bondi. Two weeks after his retinal detachment repair, he noticed a sudden burst of tiny specks while scrolling through his laptop. He also saw a brief flash when he stood up quickly. Following the checklist, he called us that evening, came in the next morning, and we discovered a tiny retinal tear. A prompt laser retinopexy sealed it, and his vision stayed stable.
Contrast that with Priya, a 54‑year‑old yoga instructor who felt a few extra floaters a month after surgery but assumed they were “just part of healing.” She didn’t report them until a month later, when a shadow had already formed across her lower visual field. By then, the detachment required a more complex vitrectomy. The lesson? Early reporting saves both eyes and reduces recovery time.
What the numbers say
Recent audit data from our clinic (2025‑2026) shows that patients who sought care within 48 hours of a flash or surge in floaters had a 92 % rate of successful laser repair, versus a 68 % success rate when presentation was delayed beyond a week. Those statistics reinforce why acting fast isn’t just a precaution—it’s statistically better for your sight.
When you can monitor safely
If none of the red‑flag symptoms appear, you can continue to monitor. Here’s a quick weekly routine:
Review your diary every Sunday. Look for trends – are the floaters staying the same, or are they slowly increasing?
Do a brief “bright‑wall test” – stand in front of a white wall, look straight ahead, and note any new specks.
Schedule a routine follow‑up within 4–6 weeks if you haven’t already. This is when most post‑operative inflammation settles.
For a deeper dive into how floaters behave after other eye surgeries, see our guide on Floaters After Cataract Surgery: How Long Do They Last and What to Expect . It explains the vitreous changes that are similar to what you might experience after retinal detachment repair.
Bottom line: you already have the tools to spot trouble. When you see a sudden surge, flashes, or a shadow, treat it like a fire alarm – call the clinic immediately, bring your notes, and let the specialist decide the next steps. Early professional help protects your vision and keeps your recovery on track.
Step 4: Managing Floaters at Home
Okay, you’ve got the basics down – you know what to watch for and when to call us. Now let’s talk about the day‑to‑day tricks that make living with floaters a lot less annoying.
Create a low‑light “float‑check” routine
Pick a bright, plain wall (think a freshly painted white fence in your backyard) and spend a minute each evening looking straight ahead. The specks pop out against the uniform background, so you can see if anything new has joined the party. Jot down the count in your diary – it’s amazing how a quick visual scan can give you confidence that nothing’s changing.
Does it feel weird to stare at a wall? That’s normal. Think of it as a nightly eye‑check‑up, just like you’d glance at the thermostat to make sure the house is still warm.
Hydration and nutrition matter
Keeping the vitreous gel hydrated helps it stay less “jelly‑like,” which can reduce the perception of floaters. Aim for at least eight glasses of water a day, and sprinkle in foods rich in omega‑3s, lutein, and zeaxanthin. Those nutrients support retinal health and may keep the vitreous from clumping.
For a deeper dive on the exact foods that boost retinal health, see this dietary nutrients for retinal health guide.
Gentle eye‑relaxation exercises
Every 20 minutes you stare at a screen, look away and focus on something 20 feet away for at least 20 seconds – the classic 20‑20‑20 rule. It eases eye‑muscle fatigue, which can make floaters feel more pronounced when you’re tired.
Another simple trick: roll your eyes slowly in a clockwise circle, then counter‑clockwise. It encourages the vitreous to move gently, redistributing those tiny shadows so they’re less likely to cluster in one spot.
Avoid sudden pressure spikes
Heavy lifting, straining on the toilet, or intense bending can briefly increase intra‑ocular pressure. That pressure shift can jostle the vitreous and make floaters appear more active for a few hours. If you’ve got a big grocery haul or a DIY project, take short breaks – sip water, stand upright, and let your eyes settle.
And yes, you can still enjoy your weekend BBQ. Just skip the “one‑arm‑over‑the‑shoulder” lift for the first two weeks after surgery.
Sleep smart
When you lie down, the vitreous settles differently depending on how you position yourself. Sleeping on your back with a slightly elevated pillow can minimise sudden shifts. If you’re curious about the best sleep posture after retinal detachment repair, check out our guide on sleep after retinal detachment surgery .
Pro tip: keep a soft eye mask handy. It reduces stray light that can exaggerate the sparkle of floaters during the night.
When to pause and call
Even with all these home tricks, trust your instincts. If you notice a rapid increase in specks, flashes, or a curtain‑like shadow, stop the routine, note the time, and call the clinic ASAP. Those are the moments where a quick OCT scan can make all the difference.
Bottom line: managing floaters at home is about consistency, hydration, gentle movement, and a bit of mindful observation. You’ve already built the diary habit – now add these simple habits and you’ll find the specks fade into the background, not the foreground.
Step 5: Follow‑Up Care After Surgery
Now that you’ve got the basics of floaters down, it’s time to think about the appointments that keep your recovery on track. Imagine you’ve just finished your first week at home – the eye drops are settled, the eye mask is in place, and you’re still noting specks in your diary. What comes next?
First, schedule a dilated retinal exam about four weeks after the procedure. In our Sydney clinic we aim for a4‑6 week windowbecause that’s when most post‑op inflammation has calmed enough for the retina to be seen clearly. During that visit we’ll run an OCT scan, check the re‑attachment, and make sure the vitreous isn’t pulling in a way that could create new floaters.
What to expect at each follow‑up
Week 1‑2:A quick phone call from the nurse to confirm you’re using the prescribed drops correctly and not experiencing any pain or sudden flashes. If you notice a burst of new floaters, call us immediately – we’ll often book you in for an urgent scan.
Week 4‑6:The in‑person check. We’ll look for signs of a residual retinal tear, silicone oil or gas bubble position (if those were used), and we’ll compare your symptom diary to the imaging. This is also a good moment to discuss any lifestyle tweaks that might smooth the road ahead.
Month 3‑4:A second OCT if we saw anything borderline at the first visit, or if you’ve reported a change in floaters. Most patients feel a noticeable drop in the number of specks by this point, but a few still see a few lingering shadows – that’s normal.
Real‑world examples
Take Michael, a 60‑year‑old who works as a graphic designer in Bondi. After his vitrectomy he logged a sudden increase in specks at two weeks. He called us, we did an urgent OCT, and discovered a tiny retinal tear that we sealed with laser on the same day. He was back to his workstation within a month, and his floaters gradually faded.
Contrast that with Anita, a 55‑year‑old yoga instructor who waited until her six‑week appointment before mentioning a new curtain‑like shadow. By then the detachment had progressed, requiring a secondary vitrectomy. The lesson? Early calls save time, money, and vision.
Actionable checklist for each visit
Bring your symptom diary – note date, time, and any associated flashes.
List all eye drops you’re using, including frequency and any missed doses.
Prepare questions about activity restrictions – lifting, swimming, air travel.
Ask about nutrition tips; omega‑3s and lutein‑rich foods can support vitreous health.
Speaking of nutrition, many patients wonder if there’s a link between diet and floaters. While the science is still evolving, a study cited by our colleagues in Pittsburgh showed that patients who maintained a balanced diet and stayed hydrated reported a 30 % quicker reduction in perceived floaters according to Everett & Hurite .
When to adjust your plan
If you notice any of these after a follow‑up, let us know right away:
New flashes of light, especially in peripheral vision.
A sudden surge of floaters that feels like a “shower” rather than a handful.
Any drop in visual acuity, even if it’s subtle.
We might recommend a supplemental OCT, a brief course of anti‑inflammatory eye drops, or, in rare cases, a minor office‑based laser procedure to address a nascent tear.
Beyond the clinic – self‑monitoring tips
Even after your last scheduled visit, keep an eye (pun intended) on the “bright‑wall test.” Stand in front of a white wall, look straight ahead, and note any new specks. Do this once a week for the first three months, then taper to monthly checks.
And remember, the eye is a living organ that continues to remodel for months after surgery. It’s perfectly okay to still see a few floaters at three months; many patients still notice them at six months, but they usually become less intrusive.
Finally, if you ever feel unsure, give us a call. A quick 5‑minute chat can prevent a lot of anxiety and keep your recovery on the right track.
FAQ
What are floaters after retinal detachment surgery and why do they appear?
After the retina is re‑attached, the vitreous gel inside your eye can shift, thicken or liquefy. Tiny collagen strands or tiny blood cells then cast shadows on the retina – those are the floaters you notice. The surgical manipulation often agitates the vitreous, so it’s normal to see a few more specks in the weeks following the procedure. Most of the time they fade as the gel settles.
When should I be worried about new floaters?
Any sudden surge that feels like a “shower” of specks, especially if it’s accompanied by flashes of light or a curtain‑like shadow, needs urgent attention. Also watch for a rapid change in visual acuity or new peripheral loss. Those signs can mean a fresh retinal tear or detachment, and a quick call to the clinic can prevent a more serious problem.
How can I track floaters at home without fancy equipment?
Grab a small notebook or use a notes app and jot down three details each day: the time you first saw the speck, whether it was static or moving, and if any flashes appeared. Do a quick “bright‑wall test” – stand in front of a plain white wall and note any new shadows. Consistent logging gives your surgeon a clear picture at the next visit.
Do everyday activities make floaters worse?
Yes, many activities that spike intra‑ocular pressure can jostle the vitreous. Heavy lifting, straining on the toilet, intense bending, or vigorous aerobics can temporarily increase the number of specks you notice. If you’re moving furniture or doing a DIY project, pause every half hour, sip water and let your eyes settle. Most patients find that the floaters settle down once they taper those activities.
Can diet or hydration actually reduce floaters?
Staying well‑hydrated keeps the vitreous gel from becoming overly viscous, which can lessen the perception of floaters. Aim for at least eight glasses of water a day and include omega‑3‑rich foods like salmon, walnuts or chia seeds. While there’s no miracle cure, many of our patients report that a balanced diet and plenty of fluids help the specks fade faster.
What follow‑up appointments should I expect after surgery?
We usually schedule a phone check‑in within the first two weeks to confirm you’re using drops correctly. A comprehensive dilated exam with OCT comes at 4‑6 weeks, allowing us to see how the retina is healing and whether the vitreous is still shifting. A third visit around three months helps us verify that any residual floaters are stabilising. Bring your diary to each visit – it speeds up the assessment.
Is it normal to still see floaters after six months?
Yes, many patients still notice a few specks at six months, especially if the vitreous hasn't fully cleared. The brain often learns to ignore harmless floaters, so they feel less intrusive over time. If you’re still bothered after a half‑year, bring it up at your routine check‑up – we can assess whether the remnants are stable or if a minor procedure might help.
What treatment options exist if floaters become very bothersome?
There are a few options when floaters become more than a nuisance. Laser vitreolysis can break larger strands into harmless fragments, but it’s only suitable for well‑located floaters. A limited vitrectomy removes the offending vitreous, yet it’s reserved for severe cases because it carries more risk. Always discuss the benefits and risks with your retina surgeon before deciding.
Conclusion
We've walked through what to watch for, how to log those specks, and when a quick call can make all the difference.
So, what should you do now? Keep your diary handy, stick to the bright‑wall test each week, and don’t ignore any sudden surge or flash.
If you notice a shower of floaters, a flicker of light, or a curtain‑like shadow, pause, note the time, and call our clinic within 24 hours – early intervention protects your vision.
In our experience as a retina surgeon in Sydney, most patients see a noticeable drop in specks by three months, and the ones who stay on top of monitoring end up with the smoothest recovery.
Remember, the eye keeps adjusting long after the surgery – a few lingering floaters at six months are normal, but they should feel less intrusive as your brain learns to ignore them.
If any doubt creeps in, give us a call or drop us an email – a quick chat can ease anxiety and keep your recovery on track.
Staying well‑hydrated, eating omega‑3‑rich foods like salmon or walnuts, and avoiding heavy lifting for the first two weeks all help the vitreous settle faster, making those tiny shadows fade sooner.
Take a moment each day to relax your eyes – the 20‑20‑20 rule is a simple habit that reduces strain and can make floaters feel less noticeable.






Comments