Understanding epiretinal membrane causes and what they mean for your eye health
- Dr Rahul Dubey
- 2 days ago
- 14 min read
Ever walked into a room and suddenly realized your vision is a little fuzzier, like looking through a cheap screen protector? That's often the first whisper of an epiretinal membrane forming, and most people don't even know why it happens.
One of the biggest culprits is age‑related changes in the vitreous gel that fills the eye. As we get older, that gel can shrink and pull away from the retina, creating tiny tears where scar tissue can grow on the macula. Think of it like a loose wallpaper edge that starts to bubble and stick to the wall behind it.
But age isn’t the only player. Diabetes, especially when it’s not well‑controlled, can damage the tiny blood vessels in the retina. Those damaged vessels leak fluid, and the healing process often leaves behind a thin sheet of membrane. I’ve seen patients in their 40s with early‑onset diabetes develop this kind of membrane after just a few years of elevated blood sugar.
Trauma is another surprise factor. A mild blow to the eye—say from a racquet sport—might not break anything visibly, yet the shock can set off inflammation that eventually leads to scar tissue. For example, a marathon runner who slipped on a wet trail reported a gradual loss of central vision months later, and an exam revealed an epiretinal membrane likely sparked by the impact.
Inflammatory eye conditions like uveitis also tip the scales. When the eye’s immune system is on high alert, cytokines encourage fibroblasts to lay down collagen right on the retinal surface. A recent case I handled involved a patient with chronic uveitis who, after years of steroid drops, developed a membrane that blurred his reading.
Genetics can’t be ignored either. Some families seem to inherit a predisposition for abnormal vitreoretinal adhesion, meaning the membrane can appear even without the usual risk factors. If you have a close relative with macular pucker, keep an eye on your own vision changes.
Finally, lifestyle factors like smoking amplify oxidative stress, which accelerates cellular aging in the retina. Cutting back on cigarettes and boosting antioxidant intake—think leafy greens and omega‑3s—can slow down that scar‑forming process.
Understanding these causes helps you spot red flags early. If you notice distortion or a new “gray spot” in your central view, schedule a check‑up. Early detection means we can discuss monitoring or, if needed, a vitrectomy to remove the membrane before it steals your sight. For a deeper dive into what an epiretinal membrane looks like and how we treat it, check out our epiretinal membrane overview page.
TL;DR
If you’ve noticed a blurry spot or wavy lines, it’s often the result of an epiretinal membrane sparked by aging, diabetes, eye injury, inflammation, genetics, or smoking. Understanding these epiretinal membrane causes helps you catch problems early and discuss monitoring or surgery with your retina specialist right now for you.
Understanding Epiretinal Membrane Formation
Ever wonder why a tiny speck of blur suddenly shows up in the middle of your view? That moment often marks the early stage of an epiretinal membrane forming on the macula. The membrane is essentially a thin sheet of scar tissue that grows right on the surface of your retina, and it can turn everyday reading into a frustrating puzzle.
So, what actually triggers that scar tissue? The short answer is a mix of age‑related changes, metabolic stress, and occasional injuries. But let’s break it down because each cause tells us something about how we might slow the process.
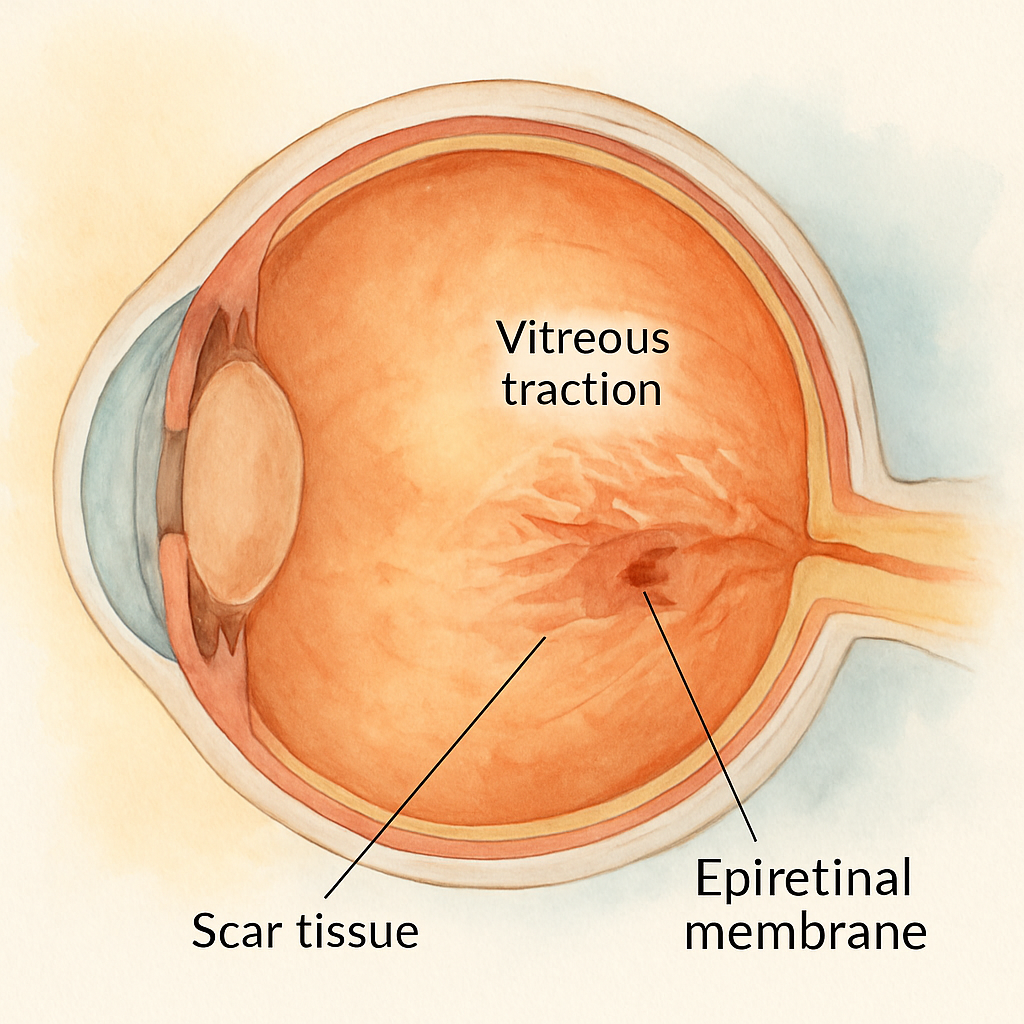
Age‑related vitreous traction
As we age, the gelatinous vitreous inside the eye starts to shrink and pull away from the retina. When that happens, tiny micro‑tears appear at the junction where the vitreous meets the macula. Those micro‑tears become a landing pad for fibroblasts, the cells that lay down collagen. Over months, that collagen builds up into a membrane you can actually feel as distortion.
Think of it like wallpaper that starts to bubble at the edges – the bubble is the membrane, and the wall is your retina. If you’ve been watching the clock tick past 60, this is probably the most common driver of epiretinal membrane causes.
Diabetes and vascular leakage
High blood sugar does more than just affect your kidneys; it also damages the tiny blood vessels that feed the retina. When those vessels leak, the eye’s repair crew rushes in, and the scar tissue they leave behind can turn into an epiretinal membrane. In my practice, patients with uncontrolled diabetes often develop a membrane a few years after their diagnosis.
Managing your A1C isn’t just about avoiding neuropathy – it’s a direct line to keeping your macula clear.
Inflammation from trauma or disease
A blunt knock to the eye, even something as mild as a racquet‑ball bounce, can set off a cascade of inflammation. Cytokines released during that response tell fibroblasts to start building a protective layer, which unfortunately becomes a membrane over time.
Chronic inflammatory eye conditions like uveitis act the same way. The immune system is essentially over‑reacting, and the side‑effect is scar tissue on the macula.
One patient I saw after a minor sports injury described the feeling as “looking through a dirty windshield” – that’s the membrane in action.
Genetics and lifestyle factors
Some families seem to inherit a predisposition for abnormal vitreoretinal adhesion. If your sibling or parent has a macular pucker, keep a closer eye on your own vision changes.
And then there’s smoking. The oxidative stress from cigarettes accelerates cellular aging in the retina, nudging the membrane formation timeline forward. Cutting back can buy you precious years of clarity.
For a concise overview of what the membrane looks like and how it’s treated, check out Epiretinal Membrane | Dr Rahul Dubey – it breaks down the anatomy in plain language.
Now, you might be asking, “Can anything I do at home help slow this down?” Absolutely. A diet rich in antioxidants – leafy greens, omega‑3 fish, and even certain herbs – supports retinal health. If you’re curious about natural options, 5BestNaturalRemedies.com curates supplements and plant‑based remedies that many patients find useful as adjuncts.
Staying well‑hydrated also matters. The vitreous is mostly water, and proper hydration helps maintain its gel‑like consistency, potentially reducing the tug‑on‑retina effect. Want a handy tool? this water‑intake calculator app makes it easy to track daily ounces.
Below is a quick visual guide that sums up the main triggers and what you can do about each.
Seeing the process in motion can demystify why your vision feels “off.” The video walks through how the membrane forms step‑by‑step, so you can spot the early signs before they become permanent.
Finally, keep this checklist handy during your next eye exam:
Notice any new wavy lines or a gray spot in the center of your view.
Ask your retina specialist about vitreous traction and membrane risk.
Review your blood sugar control and smoking habits.
Consider adding antioxidant‑rich foods or natural supplements.
Stay hydrated and track your water intake.
By understanding the why behind epiretinal membrane causes, you empower yourself to catch it early and discuss options – from careful monitoring to vitrectomy – with your doctor.
Common Causes of Epiretinal Membranes
When you first notice a wavy line on a page, the instinct is to blame fatigue or a stray hair in your eye. But for many of us the culprit is an epiretinal membrane silently forming on the macula. Understanding the why behind that sheet of scar tissue is the first step toward catching it early.
Age‑related vitreous changes sit at the top of the list. As we get older the gel‑like vitreous liquefies and eventually pulls away from the retina – a process called posterior vitreous detachment (PVD). The tiny tug creates micro‑tears in the internal limiting membrane, letting glial cells migrate onto the surface and lay down a thin collagenous sheet. Studies show that roughly 4 % of people in their 50s have an epiretinal membrane, and the figure climbs to about 12 % in those over 75 years according to the NCBI review .
Diabetes is the next big driver. High blood sugar damages the tiny retinal capillaries, causing chronic low‑grade leakage and inflammation. Those inflamed areas act like construction sites where fibro‑cells set up shop and stitch a membrane onto the macula. I’ve seen a 48‑year‑old accountant with poorly controlled Type 2 diabetes develop a noticeable pucker after just three years of elevated HbA1c, and the distortion was enough to miss an important client meeting.
Even a seemingly harmless eye bump can trigger the cascade. A racquet‑ball impact that bruises the eye may not break the globe, but the shock wave can jostle the vitreous enough to start the PVD‑induced tearing. One of my patients, an avid tennis player, felt a “floaty” shadow months after a match and later received an OCT confirming an ERM linked to that single hit.
Inflammatory eye diseases such as uveitis also lay the groundwork. The immune response releases cytokines that coax retinal glial cells into a myofibroblast phenotype, which then produce the collagen‑rich sheet. A chronic uveitis case I treated required long‑term steroid drops; after two years the patient’s reading became shaky because a membrane had formed.
Genetics can tip the balance, too. Families with a history of macular pucker often inherit a tendency for abnormal vitreoretinal adhesion. If a sibling has been diagnosed with an epiretinal membrane, it’s worth scheduling a baseline OCT even if you feel fine – early detection can spare you future frustration.
Lifestyle habits, especially smoking, accelerate oxidative stress in retinal cells. The chemicals in cigarette smoke speed up cellular aging, making the vitreous more prone to premature detachment and membrane formation. Quitting smoking not only benefits your lungs, it also gives your retina a breather. For anyone ready to kick the habit, resources like Addictik offer laser‑assisted auriculotherapy that many find effective.
Putting all these pieces together, you can create a personal risk checklist:
Age‑related vitreous detachment.
Uncontrolled diabetes or diabetic eye disease.
Recent eye trauma or blunt impact.
Chronic inflammation such as uveitis.
Family history of macular pucker.
Smoking or heavy oxidative stress.
Here’s a quick three‑step routine you can start today:
Write down any new distortion, wavy lines, or double vision in a simple vision diary.
Ask your eye doctor for an OCT scan if you’re over 50, have diabetes, or have had an eye injury.
Perform a weekly Amsler‑grid check or use M‑CHARTS to quantify metamorphopsia.
Finally, remember that not every membrane needs surgery. If your vision remains stable and metamorphopsia is mild, regular monitoring with an Amsler grid or M‑CHARTS can keep you informed. When you do need a professional opinion, the detailed guide on macular pucker symptoms walks you through what to expect during an eye exam.
Risk Factors and Demographic Trends
Ever caught yourself squinting at a screen and wondering why the letters seem to wobble? That uneasy feeling often points straight to the underlyingepiretinal membrane causes. Before we dive into treatment options, let’s unpack who’s most likely to develop this sneaky scar tissue and why.
Age tops the list. The older you get, the more the vitreous gel shrinks and pulls away from the retina, creating microscopic tears that let glial cells settle on the macula. In a population‑based study of over 4,000 Chinese adults, researchers found the overall prevalence of epiretinal membranes to be just 2.2 % per eye, but the odds climbed steadily with each additional year of life according to the Beijing Eye Study . In other words, if you’re in your 70s, you’re several times more likely to see a membrane form than when you were in your 40s.
Hyperopia (farsightedness) and higher education levels also showed a statistically significant link in that same study. It’s not that reading textbooks makes your retina scar, but the correlation hints at subtle optical or lifestyle factors that we still don’t fully understand.
Diabetes is another heavyweight. Persistent high blood‑sugar damages the tiny retinal vessels, fuels chronic inflammation, and sets the stage for fibro‑cellular growth. If you’re managing diabetes, you’ll want to explore Diabetic Eye Disease resources to keep your retina in check.
But the story doesn’t end with age and sugar. A recent 2024 comparative study of intravitreal therapies showed that eyes treated with a dexamethasone implant (DEX) developed secondary epiretinal membranes at a rate four times higher than those receiving aflibercept injections as reported in a Springer article . The mechanical stress of the implant and its biodegradable matrix may trigger abnormal vitreous traction, turning an otherwise routine injection into a membrane‑forming event.
Trauma, even a mild knock from a tennis ball, can jolt the vitreous enough to start the same cascade. Inflammation from uveitis or recurring eye infections adds another layer of risk – cytokines essentially “call in the construction crew” that lays down collagen on the macular surface.
Genetics play a sneaky role, too. If a sibling or parent has been diagnosed with a macular pucker, you’re statistically more likely to develop one yourself. Family history should be a red flag on your personal risk checklist.
And let’s not forget lifestyle. Smoking cranks up oxidative stress, accelerating cellular aging in the retina. Quitting isn’t just good for your lungs; it gives your macula a chance to breathe.
So, what can you do right now?
Take a few minutes each week to run an Amsler‑grid or M‑CHARTS test. Jot down any new wavy lines, double vision, or loss of detail. Pair that diary with an OCT scan if you’re over 50, have diabetes, or have experienced eye trauma.
Risk Factor | Why It Matters | Actionable Tip |
Age (≥60) | Vitreous liquefaction and posterior vitreous detachment increase membrane formation. | Schedule an OCT baseline and annual check‑ups. |
Diabetes | Micro‑vascular damage and chronic inflammation foster fibro‑cellular growth. | Control HbA1c < 7 % and monitor retinal health quarterly. |
Intravitreal DEX implant | Mechanical stress and biodegradable matrix may trigger abnormal vitreous traction. | Discuss anti‑VEGF alternatives with your retina specialist. |
Bottom line: knowing theepiretinal membrane causeslets you stay a step ahead. Write down your risk factors, keep an eye‑tracking routine, and bring these notes to your next appointment. Early detection often means a simple monitoring plan instead of surgery.
Preventive Measures and Early Detection
Ever caught yourself squinting at a screen and wondering why straight lines look wavy? That moment is a clue that your retina might be sending a warning sign. The good news is you can catch most epiretinal membrane causes before they turn into a full‑blown visual nuisance.
First, think of your eye like a garden. If you water it regularly, pull out weeds, and keep an eye on pests, the plants stay healthy. The same principle applies to your macula: regular check‑ups, lifestyle tweaks, and simple home tests keep the membrane from gaining traction.
Make a vision‑diary your new habit
Grab a notebook or a notes app and jot down any new distortion – wavy lines, double vision, or trouble reading a menu. Write the date, what you were doing, and how bad it felt on a 1‑10 scale. Over weeks you’ll see patterns, and that diary becomes a powerful conversation starter with your retina specialist.
Pair the diary with an Amsler‑grid or M‑CHARTS test at home. Spend two minutes once a week, and if you notice any new blips, schedule an OCT scan right away. Early imaging can reveal a thin membrane before it thickens enough to blur your world.
Control the big risk drivers
Age, diabetes, and smoking are the heavy hitters behind epiretinal membrane causes. If you’re over 60, aim for an OCT baseline and then an annual scan. For diabetics, keeping HbA1c below 7 % isn’t just about blood sugar – it’s a direct line to protecting the delicate retinal vessels that, when damaged, seed scar tissue.
And if you light up, consider this: nicotine accelerates oxidative stress, which ages retinal cells faster. Quitting can feel like a mountain, but even cutting back a few cigarettes a day can slow the scar‑forming clock.
Got a history of eye trauma or recent intravitreal injections? Bring those details to your appointment. Your doctor may adjust the follow‑up schedule or suggest anti‑VEGF alternatives to reduce mechanical stress on the vitreous.
Leverage professional monitoring
Regular visits to a retina specialist are non‑negotiable once you have risk factors. The specialists will use optical coherence tomography (OCT) to map the macula in microns. If the membrane shows signs of contraction, they’ll discuss timing for vitrectomy – a surgery that works best before permanent damage sets in.
According to the Elman Retina Group’s guidance on treatment timing , intervening early often leads to better visual recovery, because the macula hasn’t been stretched for long.
But surgery isn’t the only path. If your vision remains stable and distortion is mild, continued observation with Amsler‑grid checks can keep you in the driver’s seat. Many patients stay symptom‑free for years with just vigilant monitoring.
Nutrition and hydration tricks
Think of antioxidants as the sunscreen for your retina. Leafy greens, oily fish, and a handful of nuts supply lutein, zeaxanthin, and omega‑3s that combat oxidative stress. Stay hydrated – the vitreous gel needs water to stay supple, and dehydration can speed up liquefaction.
Finally, don’t forget to ask about any new research or clinical trials. Your doctor might have access to emerging therapies that target the cellular pathways behind membrane formation.
Putting it all together, a proactive plan looks like this:
Start a vision‑diary and do a weekly Amsler‑grid test.
Schedule an OCT baseline if you’re 60+, diabetic, or have trauma history.
Control blood sugar, quit smoking, and eat retina‑friendly foods.
Discuss any changes with your retina specialist promptly.
Remember, early detection is a partnership between you and your eye doctor. The more data you bring – dates, symptoms, lifestyle changes – the better they can tailor a plan that may keep surgery off the table.
For a quick refresher on what epiretinal membranes are and why they form, check out our Vitreous floaters information page – it breaks down the anatomy in plain language.
Conclusion
We've walked through the many epiretinal membrane causes, from the inevitable aging of the vitreous to diabetes, trauma, inflammation, genetics, and even smoking.
If any of those rings a bell in your own story, you already have a foothold for action.
The simplest step is to start a vision‑diary today—jot down when lines wobble, what you were doing, and how bad it feels. Pair that with a weekly Amsler‑grid or M‑CHARTS check, and you’ll have concrete data to bring to your retina surgeon.
Schedule an OCT baseline if you’re over 60, diabetic, or have had an eye injury—early imaging catches a thin membrane before it pulls your vision out of focus.
Control the big drivers: keep blood sugar steady, quit smoking, stay hydrated, and load up on leafy greens and omega‑3 rich fish. Those habits are like sunscreen for your retina.
Remember, early detection is a partnership. The more details you share, the better your surgeon can tailor a plan that might keep surgery off the table.
So, what’s the next move? Grab a notebook, run your first Amsler‑grid today, and call Dr. Rahul Dubey’s office to discuss an OCT baseline if you fit the risk profile. Your eyes deserve that proactive check‑in.
FAQ
What are the most common epiretinal membrane causes?
Age‑related vitreous changes sit at the top of the list. As the gel inside your eye shrinks, it pulls away from the retina and creates tiny tears where scar tissue can grow. Diabetes is the next big driver – high blood sugar damages tiny vessels, sparks inflammation and invites fibro‑cells to settle on the macula. Even a mild eye bump or chronic uveitis can set the same cascade in motion.
How does diabetes increase the risk of an epiretinal membrane?
When blood sugar stays high, the tiny capillaries in the retina leak fluid and become inflamed. That inflammation acts like a construction site, calling in glial and fibro‑cells that lay down a thin collagen sheet on the macula. Over months that sheet tightens, pulling on the retina and creating the wavy lines you might notice while reading.
Can a simple eye injury really lead to a membrane?
Absolutely. A blunt knock – say from a tennis ball or a stray branch – doesn’t have to break the eye to cause trouble. The shock can jostle the vitreous enough to start a posterior‑vitreous‑detachment. Those tiny tears let cells migrate onto the retinal surface, and a membrane can form weeks or months later, often without you realizing anything happened at the time.
Is smoking really a factor, or just a myth?
Smoking adds oxidative stress that ages retinal cells faster. The chemicals in cigarette smoke accelerate the breakdown of the vitreous gel, making the detachment process happen sooner. Faster vitreous aging means more opportunities for those tiny tears and, ultimately, a higher chance that a membrane will develop. Quitting even a few cigarettes a day can slow that clock.
What role does genetics play in developing an epiretinal membrane?
If a parent or sibling has been diagnosed with a macular pucker, you’re more likely to see one yourself. Certain families inherit a tendency for the vitreous to cling tighter to the retina, so when it finally detaches, the tearing is more extensive. That extra tearing gives cells a better foothold to build a membrane. Keeping an eye‑diary and getting a baseline OCT scan can catch early changes before they bother your vision.
When should I see a retina specialist about possible membrane symptoms?
If you notice straight lines looking wavy, double vision, or a new gray spot in the center of your view, schedule an appointment right away. Bring your vision‑diary, any recent Amsler‑grid results, and a note about risk factors like age, diabetes or recent eye trauma. An OCT scan will show whether a thin membrane is forming, and early monitoring can often keep surgery off the table.






Comments