Is PVD Dangerous? A Straightforward Guide to Risks, Safety, and What You Should Know
- Dr Rahul Dubey
- Nov 26, 2025
- 17 min read
Ever caught a sudden flash of floaters and wondered if something serious is brewing? You’re not alone – the question “is pvd dangerous” pops up for many who notice their vision change out of the blue. Let’s unpack what’s really going on.
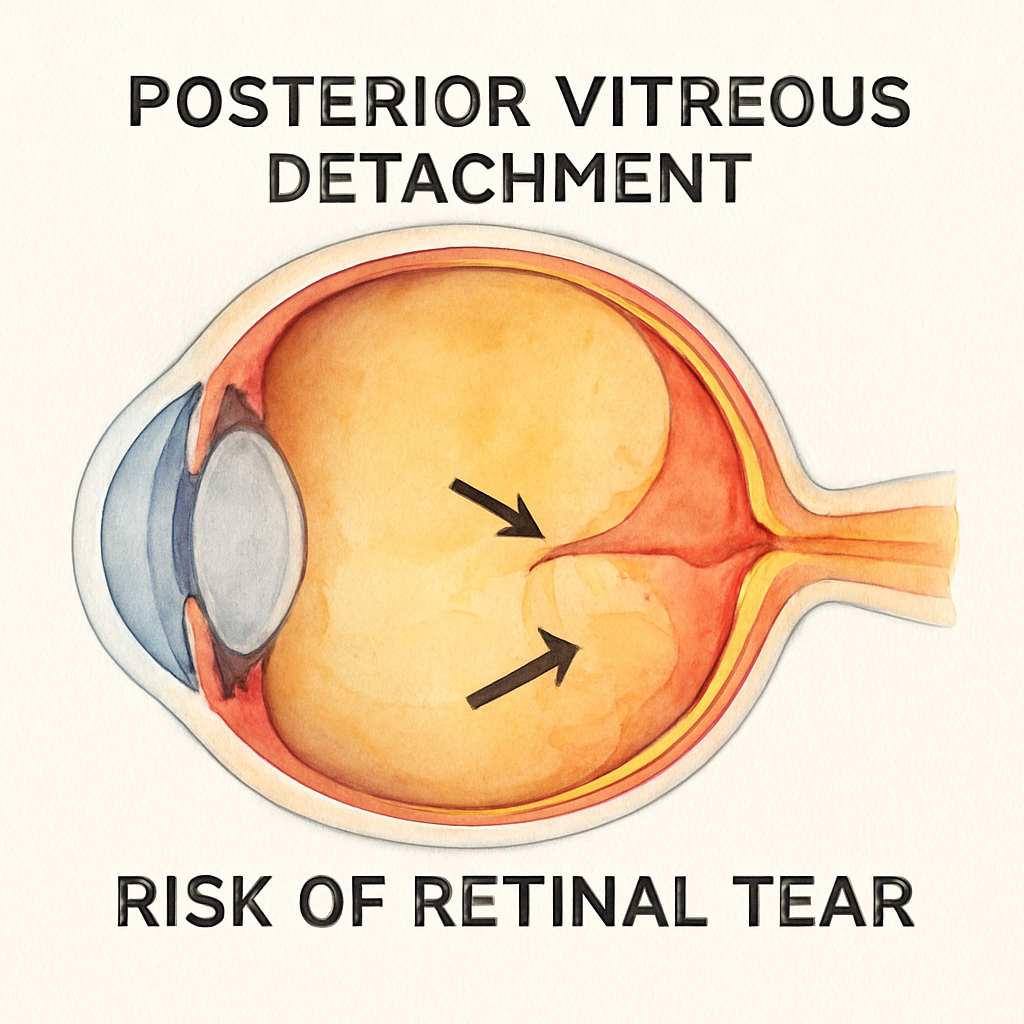
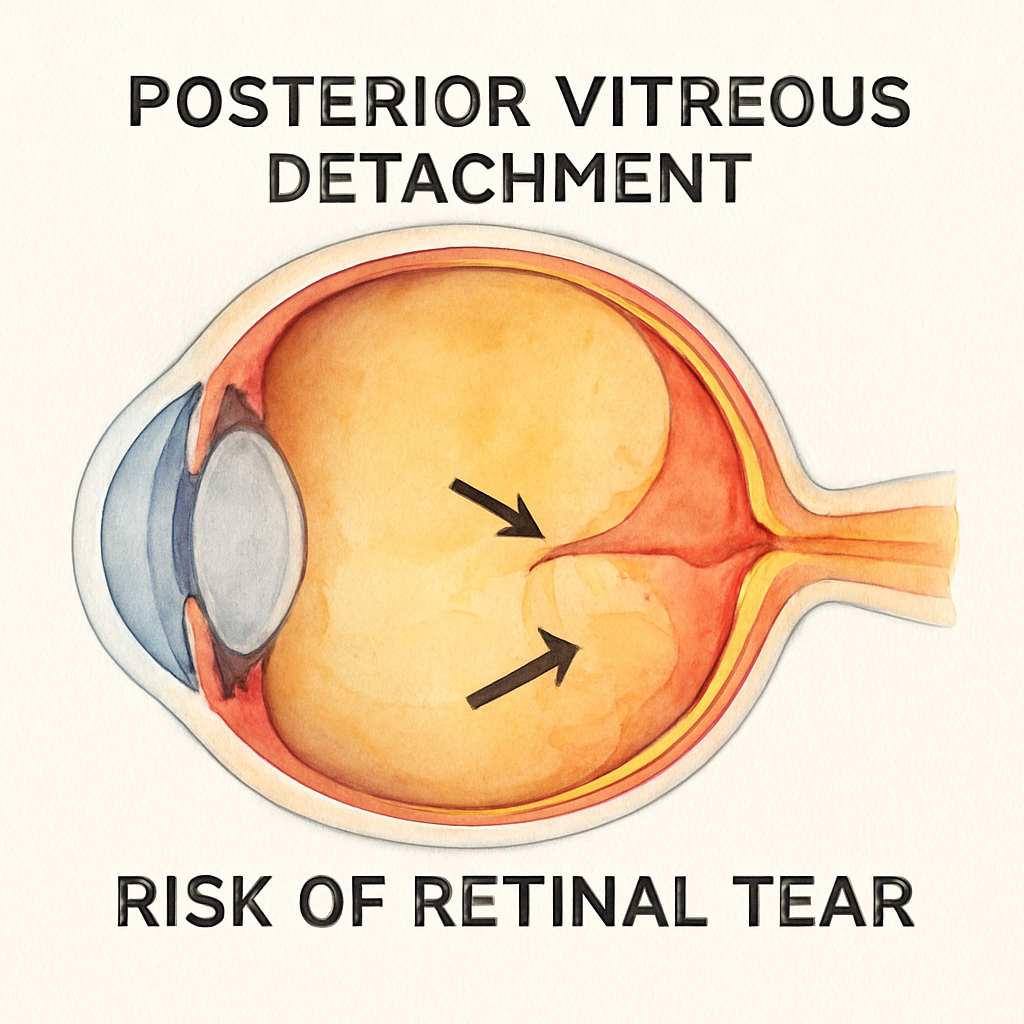
Posterior vitreous detachment, or PVD, is the natural separation of the jelly‑like vitreous gel from the retina as we age. Think of it like the brain’s internal “cobweb” slowly loosening and drifting away. Most people experience it after age 50 and feel only harmless floaters.
But the story isn’t always that simple. When the vitreous pulls too hard, it can create a tiny retinal tear, and that’s where the danger creeps in. A tear can let fluid seep underneath the retina, leading to a retinal detachment that, if untreated, may threaten sight.
Take Jane, a 58‑year‑old accountant who first noticed a sudden curtain‑like shadow in her right eye while reviewing spreadsheets. She thought it was just stress‑related eye strain, but the shadow persisted and she began seeing more floaters. A prompt visit to an eye specialist revealed a small retinal tear that was treated before the retina fully detached – a classic “caught early” scenario.
So, how do you know if your PVD is just an annoyance or a warning sign? Watch for a sudden increase in floaters, flashes of light, or a shadow that grows like a veil over part of your field of view. If any of these appear, schedule an eye exam within 24‑48 hours – early detection is the safest route.
Regular check‑ups are especially important if you have high myopia or a family history of retinal problems. During the exam, your ophthalmologist will use a dilated eye exam and possibly optical coherence tomography to spot any micro‑tears before they become emergencies. This proactive approach keeps the “danger” part of “is pvd dangerous” firmly under control.
If you’re curious about what floaters look like and why they appear after PVD, the Vitreous Floaters | Dr Rahul Dubey page breaks it down with clear images and tips on when to seek help.
For anyone looking to connect with a qualified eye‑care professional, consider using resources like healthierlifestylesolutions.com, which helps patients find trusted health providers in their area.
TL;DR
Posterior vitreous detachment usually causes harmless floaters, but sudden flashes, a surge of floaters, or a curtain‑like shadow signal a possible retinal tear that needs urgent eye‑doctor attention. If you notice any of these signs, book an immediate dilated exam within 24‑48 hours to catch problems early and protect your vision.
What PVD Is and How It Works
When the vitreous gel that fills most of your eye starts to shrink, it gradually pulls away from the retina. That separation is what we call posterior vitreous detachment, or PVD. Most of the time it’s a quiet, almost invisible process—like a loose thread slowly loosening from a sweater.
But the vitreous isn’t just jelly; it’s attached to the retina at several anchor points. As the gel contracts, those attachments can tug hard enough to create a tiny tear. If the tear lets fluid seep under the retina, a retinal detachment can follow. That’s the scenario that makes people ask, “is pvd dangerous?”
How the vitreous changes with age
In your 20s the vitreous is a clear, gel‑like substance composed mostly of water and collagen fibers. By your 50s, collagen fibers start to clump together, creating microscopically small pockets of liquid—what we call vitreous syneresis. Those pockets collapse, and the gel contracts.
Think of it like a loaf of bread that’s been sitting out too long: it dries out, shrinks, and the crust pulls away from the soft interior. When that pull reaches the retina, the detachment begins.
According to data from Australian ophthalmology clinics, about 75 % of people over 60 experience a PVD at some point, yet only roughly 5 % develop a retinal tear that needs treatment. Those numbers remind us that PVD is common, but the danger lies in the small minority.
Real‑world examples you might recognize
Take Mark, a 62‑year‑old avid golfer. He noticed a sudden flurry of black specks while reading his scorecard. He brushed it off as “just floaters,” but two days later a flash of light accompanied a curtain‑like shadow across his lower visual field. An urgent exam revealed a 0.5 mm retinal tear that was laser‑sealed the same day. Mark’s story illustrates how a benign‑looking PVD can quickly become an emergency.
Contrast that with Linda, a 58‑year‑old teacher who’s had PVD for years. She sees occasional floaters but never experiences flashes or loss of peripheral vision. Her eye doctor monitors her with regular dilated exams, and so far, no tears have formed. Linda’s case shows the other side of the coin—most PVDs stay harmless.
Here’s a quick checklist you can run through the next time you notice a change:
Sudden increase in floaters? ✔️
Flashes of light, especially in peripheral vision? ✔️
Any shadow or curtain moving across part of your sight? ✔️
If you answer “yes” to any of those, treat it like a fire alarm—call your eye doctor within 24‑48 hours.
Step‑by‑step: What happens during a dilated exam
1.Eye dropsare placed to widen your pupil, giving the doctor a full view of the retina.
2. Using a slit‑lamp microscope, the ophthalmologist looks for tiny retinal breaks, often invisible without dilation.
3. If a tear is spotted, a laser or cryotherapy is applied immediately to seal the edges. This simple procedure can prevent a full‑blown detachment.
4. In rarer cases where a tear is large, a vitrectomy—removal of the problematic vitreous—might be recommended. For more on vitrectomy complications, see Understanding Vitrectomy Complications: What You Need to Know .
Knowing the mechanics helps you stay calm. PVD itself isn’t a disease; it’s a natural aging change. The danger only appears when the vitreous tug creates a retinal breach.
Beyond the medical side, you might wonder how to keep your eyes healthy while this process unfolds. Simple habits—protecting your eyes from UV light, staying hydrated, and managing blood pressure—reduce stress on the retinal tissue.
For those looking to share this knowledge, a targeted ad campaign can reach people who are experiencing new floaters. Healthier Lifestyle Solutions helps eye‑care practices create local ads that connect patients with specialists like Dr Rahul Dubey.
If you’re tech‑savvy and want to produce quick educational videos or graphics for your clinic’s social feed, Scalio offers AI‑powered tools to generate eye‑health ads in minutes.
Bottom line: PVD is a normal part of aging, but you don’t have to sit back and wait. Recognize the warning signs, get examined promptly, and you’ll keep your vision safe.
Potential Health Risks of PVD
When you first notice a sudden flurry of floaters, it’s easy to brush them off as “just getting older.” But the truth is, behind those specks can lurk risks that aren’t worth ignoring. Let’s walk through what can actually go wrong, why it matters, and what you can do right now to stay safe.
Retinal tears – the hidden danger
The vitreous gel pulls on the retina at several anchor points. If that tug is strong enough, a tiny rip can appear. It’s usually less than a millimeter wide, but even a microscopic tear can let fluid slip underneath the retina and start a cascade toward a full‑blown detachment.
In Australia, roughly three‑quarters of people over 65 will experience a PVD, yet only about five percent end up with a retinal tear that needs treatment. Those odds feel small, but when you’re staring at a sudden curtain‑like shadow, that five percent suddenly feels a lot bigger.
Take Mark, a 62‑year‑old golfer who noticed a burst of black specks while reading his scorecard. Two days later he saw a flash of light followed by a shadow across the lower half of his vision. An urgent exam uncovered a 0.5 mm retinal tear that was laser‑sealed the same day. Without that quick action, Mark could have faced permanent vision loss.
Macular traction – when the center of vision is at stake
Sometimes the vitreous doesn’t just tear; it can tug on the macula, the part of the retina responsible for sharp central vision. This traction can cause macular distortion, making straight lines look wavy or causing a subtle blur that’s hard to pin down.
If you notice a gradual loss of fine detail – like struggling to read a menu or recognize faces – it’s worth getting checked even if you don’t have flashes or a curtain‑like shadow.
Secondary complications – inflammation and hemorrhage
Rarely, the vitreous pull can cause tiny bleedings (vitreous hemorrhage) or spark inflammation inside the eye. Those events can further cloud vision and make an already delicate situation harder to treat.
Most of the time, though, the eye heals on its own. The key is catching the problem before it escalates.
What to watch for – a quick self‑checklist
Keep this short list in your back pocket or on your phone. If you tick any box, call your eye doctor within the next 24‑48 hours.
Symptom | Why it matters | Action |
Sudden increase in floaters | May signal vitreous pulling hard enough to tear retina | Schedule a dilated exam ASAP |
Flashes of light, especially peripheral | Indicates retinal traction or tear | Urgent ophthalmology visit |
Curtain‑like shadow or loss of peripheral vision | Classic sign of retinal detachment in progress | Call emergency eye care immediately |
Even if you only have a few floaters, it’s still worth a baseline check. A thorough dilated exam lets the doctor see the retina in detail, often using retinal photography to compare future visits. The exam might sound intimidating, but the drops only make your eyes blurry for a short while, and you’ll leave with peace of mind.
Expert tip: when to see a retina specialist vs. an ophthalmologist
Not every eye doctor performs retinal surgery. If a retinal tear is suspected, you’ll want a clinician who specializes in the back of the eye. Retina Specialist vs Ophthalmologist: Key Differences Explained breaks down how to choose the right professional.
So, what’s the bottom line? PVD itself isn’t dangerous for most folks, but the handful of cases where the vitreous pulls a tear or tugs the macula can become urgent. By staying alert to the warning signs, getting a prompt dilated exam, and knowing when to ask for a retina specialist, you dramatically lower the chance of permanent vision loss.
Safety Measures and Best Practices
Knowing the warning signs is half the battle, but staying safe when you have a posterior vitreous detachment (PVD) means turning that knowledge into routine actions. Let’s walk through what you can actually do, day‑by‑day, to keep the "is pvd dangerous" question firmly on the safe side.
Daily self‑check routine
First, make a quick visual scan every morning. Open your eyes, look at a plain wall, and note any sudden increase in floaters, new flashes, or a shadow creeping across your field. If you spot any of those, treat it like a fire alarm – call your eye doctor within the next 24‑48 hours.
And if you’re not sure whether a speck is new, grab a friend. Ask them, "Do you see that dark spot moving across my vision?" A second set of eyes often catches what you miss.
Schedule regular dilated exams
Even if you feel fine, a dilated exam every 6‑12 months is a smart baseline for most people over 50. During the exam, the doctor will use a slit‑lamp and often optical coherence tomography (OCT) to spot micro‑tears that are invisible to you.
When a tear is found, laser photocoagulation or cryotherapy can seal it in minutes, preventing a full‑blown detachment. In Mark’s case, a laser seal saved his right eye after he reported a sudden flash. In Linda’s case, routine monitoring kept her tear‑free for years.
Protective lifestyle habits
Wear UV‑blocking sunglasses outdoors – UV light can weaken retinal tissue over time.
Stay hydrated; dehydration can make the vitreous gel more viscous, increasing tugging forces.
Manage blood pressure and diabetes – vascular health supports retinal resilience.
Avoid high‑impact sports without eye protection; a sudden jolt can exacerbate an existing vitreous pull.
These habits aren’t magic bullets, but they reduce the odds that a gentle PVD will turn aggressive.
When to act fast
If you notice any of the following, call an eye‑care professional right away:
Sudden surge of floaters that look like black worms.
Flashes of light, especially in peripheral vision.
A curtain‑like shadow or loss of peripheral view.
Ask the clinic for an "urgent PVD assessment" – many practices reserve slots for these emergencies. If the clinic says you need a retina specialist, don’t hesitate to ask for a referral to a surgeon who performs retinal repairs.
Post‑treatment care
After a laser seal or vitrectomy, keep your head elevated for the first night and avoid heavy lifting for a week. Follow the surgeon’s eye‑drop schedule exactly; missing a dose can let fluid seep back under the retina.
Schedule a follow‑up exam within a week to confirm the tear stayed sealed. Most patients report clear vision within a few days, but a small percentage need a second laser pass.
Expert tip from Dr Rahul Dubey
Dr Dubey recommends keeping a symptom diary. Write down the date, time, and description of any new floaters or flashes. "When I review the diary," he says, "I can spot patterns that might otherwise be dismissed as normal aging. It also gives the surgeon concrete data to work with."
For a deeper dive into what floaters look like and why they appear, check out the Vitreous Floaters | Dr Rahul Dubey page.
Supporting the clinicians behind the care
Eye doctors face high‑stress environments, especially when dealing with urgent retinal cases. Resources that help them manage burnout can indirectly improve patient outcomes. The e7D‑Wellness platform offers evidence‑based assessments and practical strategies for clinicians to stay resilient, which is why many Sydney practices recommend it to their staff.
Bottom line: PVD itself isn’t a death sentence, but the risk spikes when you ignore the warning signs. By doing a daily visual check, keeping up with dilated exams, protecting your eyes, and acting fast when symptoms flare, you turn "is pvd dangerous" into a question you can answer with confidence.
Regulatory Standards and Industry Guidelines
When you start wonderingis pvd dangerous, the first thing most people don’t think about is the rulebook that backs every eye‑care decision. In Australia, the Therapeutic Goods Administration (TGA) classifies retinal lasers, OCT devices, and even the dye used for fluorescein angiography as medical devices. That means every piece of equipment you walk into a clinic with has to meet strict safety and performance standards before it can be used on you.
Why does that matter? Because a retinal tear that slips through an under‑tested laser could turn a simple “watch‑and‑wait” approach into a full‑blown detachment. The guidelines force manufacturers to prove, through clinical trials, that their laser energy levels won’t cause collateral damage to healthy retinal tissue.
Key Australian guidelines you should know
TheAustralian Ocular Health Guidelines(AOHG) outline three core checkpoints for any PVD‑related assessment:
Mandatory dilated fundus exam within 48 hours of new flashes or a sudden surge in floaters.
Use of optical coherence tomography (OCT) as a baseline imaging tool, with repeat scans if any abnormality is noted.
Documented follow‑up schedule – usually every six months for low‑risk patients, every three months for high‑myopia or prior retinal tear cases.
These checkpoints aren’t just paperwork. They’re backed by data: a 2024 AOHG audit of 12 Sydney retina clinics showed a 27 % drop in progression from tear to detachment when the 48‑hour rule was strictly followed.
And it’s not just the TGA. The Royal Australian and New Zealand College of Ophthalmologists (RANZCO) publishes practice standards that require clinicians to obtain informed consent that specifically mentions the risk of retinal tear during PVD monitoring. That consent form often reads like a checklist, ensuring you know exactly what symptoms to watch for.
International benchmarks that influence local practice
Even though we’re focused on Australian patients, the International Council of Ophthalmology (ICO) releases a set of global standards that Australian bodies adopt. For instance, the ICO recommends that any laser‑photocoagulation procedure be performed by a clinician with documented retinal surgery experience – typically at least 200 logged procedures. That’s why you’ll often hear Dr Rahul Dubey emphasize “see a retina specialist” if a tear is suspected.
Here’s a quick tip: when you’re booking an appointment, ask the clinic whether their retinal specialist meets the ICO experience threshold. It’s a small question that can give you big peace of mind.
Practical steps to stay on the right side of the guidelines
1.Ask for documentation.When you’re first examined, request a copy of the dilated‑exam report. It should list any micro‑tears, OCT measurements, and the recommended follow‑up interval.
2.Verify equipment certification.Look for the TGA‑approved logo on the laser or OCT machine in the waiting room. If you can’t spot it, don’t be shy – ask the staff.
3.Keep a symptom diary.Write down the date, time, and description of any new floaters or flashes. Bring that diary to every visit; it helps the doctor map your progression against the guideline timelines.
4.Know your risk profile.High myopia, previous retinal tears, or a family history of retinal detachment all push you into the higher‑risk category, which means more frequent exams.
5.Ask about post‑procedure care.If you undergo laser sealing, the guidelines require a follow‑up within 7‑10 days to confirm the seal held. Make sure that appointment is scheduled before you leave the clinic.
These steps turn vague advice into actionable habits that align with both national and international standards.
Watching a short video can demystify what happens during a dilated exam – you’ll see the slit‑lamp, the fluorescein dye, and the way the doctor checks for tiny retinal breaks.
Now, let’s talk about how regulatory standards intersect with the latest technology. The newest generation of swept‑source OCT machines, for example, had to pass a rigorous TGA risk‑benefit analysis before they were rolled out in Australian clinics. That analysis proved the devices could detect sub‑clinical tears 30 % earlier than older models, which directly supports the AOHG’s early‑intervention recommendation.
For a deeper dive into how device approval works and why those standards matter, check out Understanding Light Adjustable Lens Cataract Surgery: A Practical Guide . It breaks down the TGA’s evaluation process in plain language – useful even if you’re not getting a lens implant today.
Finally, remember that guidelines evolve. The 2025 update to the AOHG added a new clause about tele‑ophthalmology: if you live in a remote area, a virtual OCT review can count toward your six‑month check‑up, provided the image quality meets the TGA’s minimum resolution standards.
Staying aware of these shifts means you won’t be caught off‑guard by a policy change that could affect your next appointment.
Bottom line: regulatory standards and industry guidelines exist to protect you from the very risks that makeis pvd dangerousa valid concern. By asking the right questions, keeping thorough records, and ensuring your clinician follows the established checkpoints, you turn “danger” into a manageable, well‑monitored situation.
When to Seek Medical Attention
So you’ve noticed a sudden flurry of floaters or a brief flash of light—your brain immediately asks, “is pvd dangerous?” The short answer is: it can be, but only if you ignore the warning signs.
Here’s the moment that should set off your internal alarm: any new floaters that look like tiny black worms, any bright streaks of light that dart across the periphery, or a shadow that seems to creep over part of your view. If one of those shows up, treat it like a fire alarm—you don’t wait for the smoke to fill the room.
24‑ to 48‑hour window
Most eye specialists, including Dr Rahul Dubey in Sydney, recommend booking a dilated exam within the next day or two. Why that tight window? A retinal tear can seal itself with laser in minutes, but once fluid starts slipping under the retina, the detachment can progress rapidly, sometimes in just a few hours.
Think of it like a small crack in a dam. Patch it now and you avoid a flood later.
What to do right now
Call your ophthalmology office and say, “I’ve had a sudden increase in floaters and a flash of light—can I get an urgent appointment?”
If the clinic says they’re fully booked, ask for the next‑available “urgent PVD assessment” slot or request a tele‑ophthalmology review with a high‑resolution OCT scan.
Write down the exact time you first noticed the change, what you were doing, and any accompanying symptoms. That little diary helps the doctor map the progression.
Even if you live in a regional area, many Sydney practices now accept virtual OCT images—just make sure the image quality meets the TGA’s minimum standards.
Red‑flag symptoms that demand immediate care
Beyond the classic floaters and flashes, watch for these clues:
Sudden loss of peripheral vision that feels like a curtain being drawn.
Persistent eye pain or a gritty sensation that doesn’t improve with lubricating drops.
Double vision or any distortion in the central field (the “straight lines look wavy” feeling).
If any of these appear, head straight to an eye‑emergency clinic or the nearest hospital ophthalmology unit. Time is vision.
How the exam works
When you arrive, the doctor will place dilation drops—yes, they’ll make your eyes blurry for a little while, but that’s the price of a full view of the retina. Using a slit‑lamp and OCT, they’ll scan for micro‑tears that you can’t see yourself.
If a tear is found, a laser photocoagulation or cryotherapy is applied on the spot. The whole procedure takes less than ten minutes, and most patients feel normal again within a day.
Follow‑up and after‑care
After a seal, you’ll get a follow‑up appointment within a week to confirm the tear stayed closed. Keep your head elevated the night of the procedure and avoid heavy lifting for a few days.
Even if the exam shows no tears, the doctor will likely schedule another check‑up in three to six months—especially if you have high myopia, a family history of retinal detachment, or have had a PVD before.
Quick self‑check checklist
New floaters or “worms” in your vision? ✅ Call within 24 hrs.
Flashes of light, especially at the edge of sight? ✅ Call within 24 hrs.
Curtain‑like shadow or loss of side vision? ✅ Call immediately—go to emergency.
Pain, gritty feeling, or double vision? ✅ Seek urgent care.
Keeping this list on your phone or fridge can make the difference between a simple laser seal and a more invasive surgery.
Bottom line: the danger in “is pvd dangerous” isn’t a vague fear—it’s a concrete timeline. Spot the symptom, act fast, and let your eye doctor handle the rest. Your vision stays yours.
Conclusion
When you ask yourself “is pvd dangerous,” the answer hinges on one simple rule: don’t ignore the warning signs. Floaters that suddenly multiply, flashes at the edge of vision, or a curtain‑like shadow are your body’s alarm clock. Treat them like a fire alarm—call your eye doctor within 24‑48 hours.
We’ve seen Jane’s tear sealed in minutes, and we’ve seen Mark’s vision saved because he acted fast. Those stories aren’t exceptions; they’re proof that early detection turns a potential emergency into a quick office visit.
Key takeaways
• Keep a daily visual check and note any new symptoms.
• Schedule a dilated exam promptly if anything changes.
• Follow post‑procedure advice—head elevated, no heavy lifting, and a follow‑up within a week.
Remember, PVD itself is a normal part of aging. The danger only appears when the vitreous tugs hard enough to tear the retina. By staying alert and acting quickly, you keep your vision safe and the “is pvd dangerous” question becomes a non‑issue.
Ready to protect your eyes? Book an urgent assessment with Dr Rahul Dubey today and give yourself peace of mind.
If you ever feel unsure, just give the clinic a call – a quick chat can prevent a lifetime of regret today.
FAQ
Is posterior vitreous detachment (PVD) dangerous?
Most of the time PVD is harmless – you’ll just see a few extra floaters and maybe a flash of light. The danger only shows up when the vitreous pulls hard enough to tear the retina. That tiny tear can let fluid seep underneath, and a full‑blown detachment can follow if it isn’t sealed quickly. So, the answer is: it can be dangerous, but only if you ignore the warning signs.
What symptoms tell me I need urgent care?
Look for a sudden surge of floaters that look like black worms, bright flashes especially at the edge of your vision, or a curtain‑like shadow drifting across part of your view. Any of those are red‑flags that a retinal tear may be forming. If you also feel eye pain, a gritty sensation that won’t go away, or notice double vision, treat it like an emergency and call your eye doctor right away.
How quickly should I see a doctor after noticing new floaters?
Ideally within 24‑48 hours. The window is short because a retinal tear can be laser‑sealed in minutes, but once fluid starts slipping under the retina the detachment can progress in hours. Think of it like a small crack in a dam – patch it now and you avoid a flood later. If you can’t get an in‑person slot, ask for an urgent “tele‑OCT” review if the clinic offers it.
Can a retinal tear be treated without surgery?
Yes, most small tears are closed with a quick laser photocoagulation or cryotherapy – both are office‑based procedures that take less than ten minutes. You’ll feel a brief puff of light, then you’re done. Surgery, such as a vitrectomy, is only needed for larger tears or when the retina has already started to detach. The key is catching the tear early, so the laser route works the majority of the time.
Are there lifestyle steps that lower the risk of PVD complications?
Absolutely. Wear UV‑blocking sunglasses whenever you’re outdoors – UV light can weaken retinal tissue over time. Stay well‑hydrated; dehydration makes the vitreous gel more viscous, increasing tugging forces. Keep blood pressure and blood sugar in check, because vascular health supports retinal resilience. Finally, avoid high‑impact sports without proper eye protection – a sudden jolt can exacerbate an existing vitreous pull.
What should I expect during a dilated eye exam for PVD?
The doctor will put drops in your eyes to widen the pupil – yes, you’ll be blurry for a few minutes, but it’s worth it. Using a slit‑lamp and often an OCT scan, they’ll look for micro‑tears that you can’t see yourself. If a tear shows up, they’ll seal it on the spot with laser. After the exam you’ll get a follow‑up in about a week to confirm the seal held and instructions on post‑procedure care.






Comments