Comprehensive Guide to BRVO Treatment Options and Recovery
- Dr Rahul Dubey
- 4 days ago
- 16 min read
Ever looked at a blurry spot in your vision and wondered if it’s something you just have to live with?
That moment of panic—when you realize you might have a branch retinal vein occlusion (BRVO) and the doctor mentions "treatment"—can feel like standing at the edge of a cliff. You’re scared, you want answers, and you need a plan that actually works.
Let’s be honest: BRVO isn’t just a fancy term for eye trouble. It’s a blockage in one of the retinal veins that can cause swelling, bleeding, and, if left unchecked, permanent vision loss. The good news? Modern brvo treatment options have come a long way, and you don’t have to accept a dimmer world.
So, what does "brvo treatment" really mean for you? Think of it as a toolbox. On one side you have anti‑VEGF injections that calm the leaky vessels and reduce macular edema. On the other, laser photocoagulation that seals off the problematic vein. Sometimes a combination works best, and your retinal surgeon will tailor the approach to your specific blockage.
Imagine walking into Dr. Rahul Dubey’s clinic in Sydney. You sit down, share the story of the sudden dark spot, and he explains that a quick injection can often restore clarity within weeks. It’s not a miracle cure, but it’s a proven method that millions of patients rely on.
But here’s the kicker: timing matters. The sooner you start brvo treatment, the better the chance of preserving your central vision. Delaying can let swelling harden into scar tissue, making recovery harder.
Now you might be asking, "Will I need surgery?" Most patients avoid invasive surgery; they just need a few office visits for injections or a laser session. And even if you do need a vitrectomy, advances in micro‑incision techniques keep recovery short.
Ready to take the next step? Start by scheduling a comprehensive retinal exam. Bring a list of your symptoms, any recent health changes, and an open mind. From there, your doctor can map out a brvo treatment plan that aims to protect what matters most—your sight.
TL;DR
If you’ve noticed a dark spot or blurry vision, brvo treatment can halt swelling, restore clarity, and protect your central sight.
Act quickly: schedule a retinal exam, discuss anti‑VEGF injections or laser options with Dr. Rahul Dubey, and follow up as soon as possible to keep your vision sharp now.
Step 1: Understanding BRVO and Its Causes
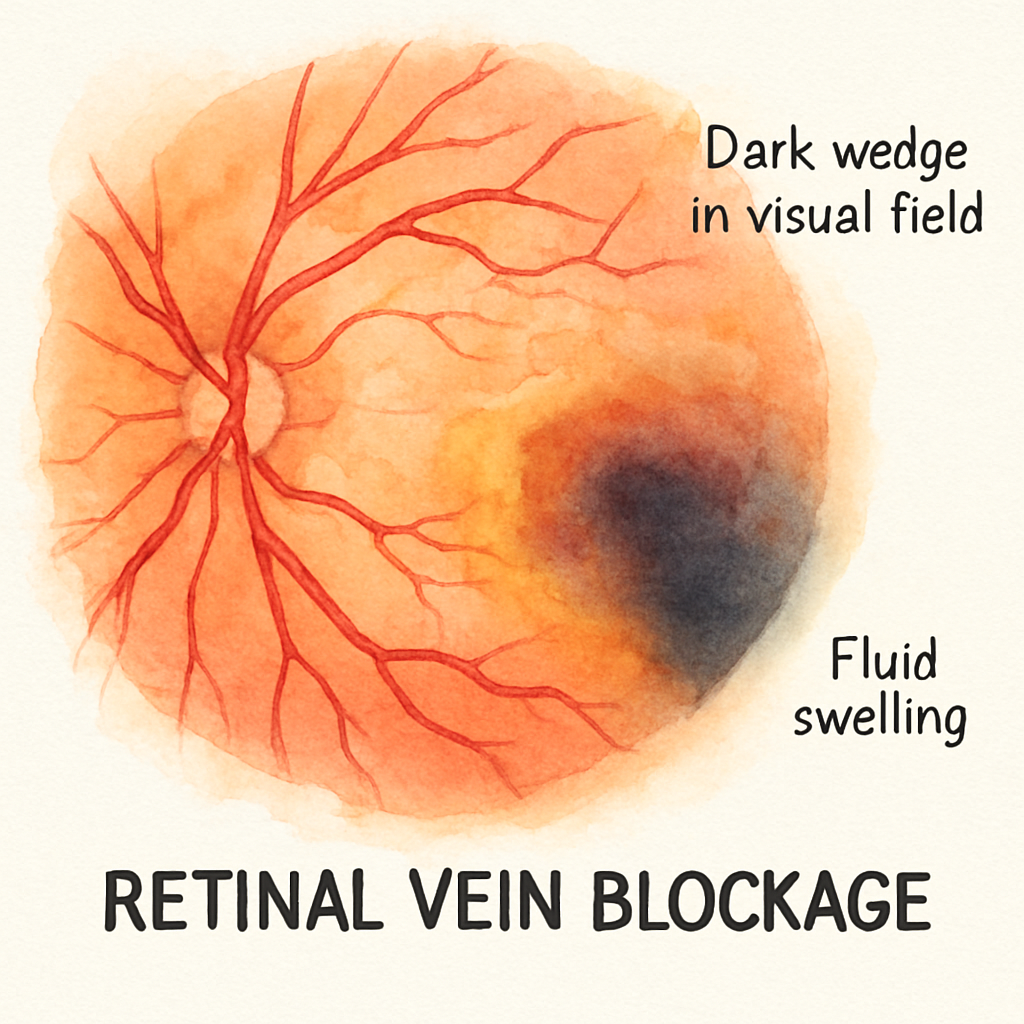
Imagine you’re scrolling through photos on your phone and suddenly a dark wedge appears in the corner of your vision. Your brain screams, “What’s wrong?” That moment is often the first clue that a branch retinal vein occlusion (BRVO) is taking hold.
What is BRVO?
BRVO happens when a smaller branch of the retinal vein gets blocked, usually by a clot. The blockage forces blood to pool behind it, causing fluid to leak into the retina. That fluid is what makes the blurry or shadowy spot you notice.
It’s not a full‑blown retinal vein occlusion, which would affect the entire eye, but it can still steal central vision if left unchecked.
Common Causes and Risk Factors
Most of the time the root cause is something you already live with: high blood pressure, diabetes, or high cholesterol. These conditions make the blood vessels stiff and prone to clotting.
Age is another player – the older you get, the more likely the tiny veins have narrowed over time. Smoking, obesity, and a sedentary lifestyle add fuel to the fire.
Even a sudden spike in blood pressure – say, after a stressful work meeting – can trigger a blockage in a vulnerable vein.
Real‑World Examples
Take Sarah, a 58‑year‑old teacher from Sydney. She managed her hypertension with medication, but she skipped her annual eye check‑up for two years. One morning she woke up seeing a half‑moon shadow in her right eye. After an urgent retinal exam, Dr. Rahul Dubey diagnosed a BRVO in the superior temporal branch. Within weeks of anti‑VEGF injections, the swelling receded and Sarah’s vision sharpened.
Then there’s Mark, 45, who’s otherwise fit but smokes a pack a day. He noticed a “floaty” curtain in his left eye after a marathon. The cause? A clot formed in a retinal branch, likely spurred by the temporary rise in blood pressure during the race. Mark’s case shows that even athletes aren’t immune if other risk factors linger.
Both stories underline a key point: BRVO rarely shows up out of the blue. It’s the cumulative effect of systemic health and lifestyle.
How to Spot Early Signs
Here’s what to watch for:
A sudden dark spot or shadow that doesn’t move with your eye.
Blurry vision that’s worse in one eye.
Seeing “flashes” of light, especially when looking at a plain background.
If any of these pop up, book a retinal exam ASAP. Early detection is the difference between a quick recovery and permanent vision loss.
Actionable Steps for You
1.Schedule a comprehensive eye exam.Ask your optometrist to do a dilated retinal scan – it’s the gold standard for spotting vein blockages.
2.Control systemic health.Keep blood pressure < 130/80 mmHg, maintain A1C under 7 % if you have diabetes, and aim for LDL‑C below 100 mg/dL.
3.Quit smoking.Even cutting back by one cigarette a day can improve blood flow to the retina.
4.Stay active.A 30‑minute walk most days helps regulate blood pressure and cholesterol.
5.Know your treatment options.Anti‑VEGF injections are often the first line because they quickly reduce macular oedema – the swelling that threatens your central vision. For a deeper dive into how these injections work, check out Retinal Vein Occlusion - Vitreous Floaters .
6.Check your insurance coverage.Many health plans now cover retinal injections. A quick read on group health insurance options can save you surprise bills.
7.Consider promotion support.If you run a clinic, partnering with a specialist ad agency can help you reach patients who need urgent BRVO care. Learn how targeted Facebook ads work here .
By understanding the why behind BRVO and acting on these steps, you give yourself the best shot at preserving clear sight.
Step 2: Diagnosing BRVO – Tests and What They Reveal
Okay, you’ve spotted that dark wedge in your vision and you’re wondering what’s really going on. The next logical step isn’t “wait and see” – it’s getting the right tests so you and your doctor can actually see the blockage.
1. Dilated Fundus Exam – the baseline
First up, the good‑old dilated eye exam. Your eye doctor puts drops in your eyes, waits for them to work, and then looks through a slit‑lamp with a special lens. This lets them see the retina’s blood vessels, the exact spot of the vein blockage, and any hemorrhage or swelling. It’s quick, painless, and it’s the foundation for every other test.
2. Optical Coherence Tomography (OCT) – a cross‑section snapshot
Think of OCT like an ultrasound for your eye, but with micrometer‑level detail. It creates a layered image of the retina, showing you whether fluid has built up in the macula – the part that gives you sharp central vision. If the OCT shows macular oedema, that’s a clear sign you’ll likely need anti‑VEGF injections later.
Real‑world example: James, a 62‑year‑old accountant, noticed a sudden “shadow” in his left eye after a stressful tax season. His OCT revealed 150‑micron thick fluid under the macula. Within two weeks of treatment, the fluid thinned to 70 microns and his vision improved dramatically.
3. Fluorescein Angiography (FA) – mapping blood flow
FA involves injecting a fluorescent dye into your arm and taking rapid‑fire photos as the dye travels through retinal vessels. It highlights areas of leakage, non‑perfusion, and the exact point where the vein is blocked. The test is especially useful when OCT findings are ambiguous.
Expert tip from Dr. Rahul Dubey: “If you see irregular leakage on FA, we often pair it with targeted laser photocoagulation to seal off the leaky vessels before starting injections.”
4. Ultrasound B‑scan – when the view is cloudy
If there’s a lot of bleeding or a dense cataract obscuring the retina, a B‑scan ultrasound can still visualize the back of the eye. It helps rule out other causes of vision loss, such as retinal detachment, which would require a different treatment pathway.
5. Systemic Work‑up – the whole‑body connection
BRVO rarely happens in isolation. Your eye doctor will likely order blood pressure checks, a lipid panel, and an HbA1c test. High blood pressure, uncontrolled diabetes, and elevated cholesterol are the three biggest risk factors. Knowing your numbers lets you and your doctor tailor both ocular and systemic treatment.
Case in point: Maya, 55, came in with a blurry spot after a marathon. Her eye work‑up showed normal OCT but the FA revealed a tiny non‑perfused area. A simultaneous blood work panel uncovered borderline high LDL. Adjusting her diet and starting a low‑dose statin stopped further vein occlusions.
Actionable Checklist for Your Diagnosis Visit
Call your eye clinic and request a dilated retinal exam with OCT and FA.
Ask if a B‑scan is needed based on any media opacity (cataract, vitreous bleed).
Bring a list of your current medications, recent blood pressure readings, and any recent lab results.
Write down any symptoms you’ve noticed – flashes, floaters, or changes in peripheral vision.
Ask the doctor to explain what each test will show you and how the results will guide treatment.
When you walk out of the office with a clear picture of what’s happening inside your eye, you can move confidently toward the right retina specialist vs ophthalmologist decision and the most effective brvo treatment plan.
And a quick heads‑up: clinics that keep their websites up‑to‑date and secure make it easier to book appointments and download test results. If you run a practice, consider partnering with a reliable website maintenance service to keep everything running smoothly.
Step 3: Treatment Options Overview (Video)
You've made it past the diagnosis maze and now you’re staring at a list of possible treatments. It can feel overwhelming – anti‑VEGF injections, laser photocoagulation, steroid implants, even vitrectomy in rare cases. To cut through the noise, we've embedded a short video that walks you through each option in plain language.
Hit play and pause whenever you need to jot something down. The narrator, Dr. Rahul Dubey, points out the pros, the downsides, and the typical timeline for each therapy. It’s the kind of “watch‑and‑learn” moment that replaces a dense brochure with a friendly chat over coffee.
What the video covers
First, the anti‑VEGF injections. These are the workhorse for most BRVO patients because they target the VEGF molecule that drives macular edema. In the clip, Dr. Dubey explains why you’ll likely need a series of monthly shots before the swelling eases, and how the retina’s thickness is tracked with OCT after each visit.
Second, laser photocoagulation. The video shows a split‑screen of the laser map and the actual fundus, so you can see exactly where the burns are placed to seal off the leaking vein. It’s a one‑time procedure in many cases, but the recovery window is a bit longer than injections.
Third, corticosteroid implants. If you have a history of frequent injections or a contraindication to anti‑VEGF drugs, the steroid option might be a better fit. The narrator walks through the insertion technique and highlights the need for regular intra‑ocular pressure checks.
How to use the video as a decision‑making tool
While you watch, keep a notebook or your phone handy. Write down three things that matter most to you – speed of vision recovery, number of clinic visits, or cost concerns. Then, after each segment, note which treatment checks those boxes.
Next, compare your notes with your own health profile. For example, if you have uncontrolled glaucoma, the steroid route might raise red flags. If you’re juggling a busy job, the laser’s single‑visit nature could be appealing.
Finally, bring this shortlist to your next appointment. Say something like, “I watched the video and I’m leaning toward anti‑VEGF because I want the quickest visual improvement, but I’m worried about the number of injections.” This shows you’re engaged and gives the doctor a clear starting point.
Quick checklist after the video
Identify which treatment aligns with your lifestyle and medical history.
Ask your doctor about the expected number of injections or laser sessions.
Clarify any side‑effect profile – for injections, see Eye Injection Side Effects for a concise rundown.
Confirm insurance coverage and out‑of‑pocket costs before you sign any consent.
Schedule a follow‑up OCT in 4‑6 weeks to see if the macular thickness is improving.
One emerging tool that may soon help you decide is artificial‑intelligence prediction. A recent study showed that a deep‑learning model using fluorescein angiography images predicted short‑term anti‑VEGF success with 88.6% accuracy, giving doctors an extra data point when tailoring therapy according to the research .
Bottom line: the video gives you a visual, jargon‑free overview, and the checklist turns that knowledge into an actionable plan. You’re no longer guessing – you’re making an informed choice about your brvo treatment.
Step 4: Choosing the Right Treatment – Comparison Table
Alright, you’ve watched the video, jotted down your priorities, and now you need a quick way to see which brvo treatment actually fits your life. That’s where a side‑by‑side table becomes your best friend.
Do you want the fastest visual recovery, the fewest clinic visits, or the lowest out‑of‑pocket cost? Maybe you’re juggling glaucoma meds and worry about steroid‑induced pressure spikes. Whatever your “must‑have”, line it up against the three main options and let the facts do the heavy lifting.
Comparison at a glance
Treatment | Typical Sessions | Pros | Cons |
Anti‑VEGF injections | 1‑month intervals, 3‑6 initial shots then as‑needed | Fastest edema reduction, strong visual‑acuity gains, proven across many trials | Requires repeated visits, small risk of infection, cost can add up |
Grid laser photocoagulation | Single session (sometimes a repeat after 4‑6 months) | One‑time procedure, lower complication rate, no injection‑related anxiety | Slower vision improvement, may be less effective for thick macular edema |
Intravitreal steroid (TA or dexamethasone implant) | Every 3‑4 months (implant) or 4‑6 months (TA) | Reduces injection burden, helpful when anti‑VEGF response wanes | Higher chance of cataract formation and IOP rise, cost varies |
Notice the pattern? Injections win on speed, laser wins on simplicity, steroids sit in the middle but bring their own risk profile.
Let’s unpack each column so you can match it to your story.
Anti‑VEGF injections
These drugs target the VEGF molecule that fuels macular swelling. Studies repeatedly show that patients gain three or more lines on a vision chart within a few months — the same improvement reported in the SCORE study for laser, but with a quicker timeline according to the National Eye Institute . If you need your eyesight back for work or driving, this is the go‑to.
But remember, you’ll be back in the clinic every four weeks at first. That’s why many people ask, “Can I switch later if injections become a hassle?” The answer is often yes – you can transition to a steroid or laser once the edema settles.
Grid laser photocoagulation
Laser applies a patterned series of burns to the leaking vein area. The SCORE trial found visual gains comparable to steroids, yet with fewer complications the same NEI report notes . It’s attractive if you dread needles or have a busy schedule that can’t accommodate monthly visits.
On the downside, the vision improvement can take 8‑12 weeks, and some patients still need a follow‑up injection if edema persists.
Intravitreal steroids
Both triamcinolone acetonide and the dexamethasone implant have shown similar efficacy in reducing cystoid macular edema — the OMAR study even highlighted a 30 % drop in injection frequency after switching from anti‑VEGF as reported by Retina Today . If you’ve hit a plateau with anti‑VEGF, a steroid may give you that extra push.
Just keep an eye on cataract development and intra‑ocular pressure; those are the two most common side effects.
Now, how do you turn this table into a decision? Grab a pen, write down your top three priorities, and give each treatment a score from 1 – 5. Add the scores up and you’ll see which option tops the list.
Cost is another reality check. Anti‑VEGF drugs can run 1,200‑1,500 per injection in Australia, while a single laser session might cost a few hundred dollars and steroids sit somewhere in between. Your insurance plan will tip the scales, so jot down the approximate out‑of‑pocket amount for each option.
Still feeling stuck? A quick chat with your retina specialist can clarify any gray area. You might even pull up the Retinal Vein Occlusion – Vitreous Floaters guide during the appointment so you both speak the same language.
Bottom line: the right brvo treatment isn’t a one‑size‑fits‑all. It’s the one that aligns with how fast you want results, how often you can visit the clinic, and how comfortable you are with potential side effects. Use the table, score your needs, and you’ll walk into your next appointment with confidence.
Step 5: Post‑Treatment Care and Lifestyle Adjustments
You've just finished your brvo treatment and the clinic lights are dimming. That mix of relief and uncertainty is normal – you wonder what comes next and how to keep the progress you just earned.
What to expect in the first days
Right after an injection or laser session it's common to feel a little gritty, like dust in your eye. A faint redness or mild ache may linger for a few hours. Most patients notice the hazy vision clears within 24‑48 hours, although a brief flash of floaters can pop up and then fade.
According to clinical observations, temporary blurriness and floaters are typical and usually resolve on their own source . Your doctor will give you a follow‑up schedule – expect an OCT scan in about a month to see how the macular edema is responding.
During this window, avoid rubbing the eye. A gentle rinse with sterile saline if something feels gritty can help, but never press on the treated eye.

Managing common side effects
Most side effects are mild. Over‑the‑counter pain relievers like ibuprofen can tame a throbbing headache, and a cold compress for 10 minutes a few times a day eases surface irritation.
If you notice a rise in eye pressure, increasing redness, or worsening vision, call your retina specialist right away – those could signal an infection or pressure spike that needs prompt attention.
For those who received a steroid implant, keep an eye on cataract development and intra‑ocular pressure. Those two issues pop up more often with steroids, so regular pressure checks are part of the plan.
Long‑term eye health habits
Post‑treatment isn’t just about the eye; it’s about the whole body. High blood pressure, diabetes, and cholesterol are the three big risk factors that keep coming back. Keeping your systolic below 130 mmHg, your A1C under 7 %, and your LDL under 100 mg/dL dramatically lowers the chance of another blockage.
Eat a rainbow of vegetables, grab a handful of walnuts for omega‑3s, and stay hydrated. A 30‑minute walk most days helps regulate blood pressure and reduces inflammation. And if you smoke, cutting down even a few cigarettes a day can improve retinal circulation.
Regular eye exams remain the backbone of prevention. Even if your vision feels back to normal, schedule a dilated exam with your retina specialist every six months. Those visits let the doctor catch tiny leaks before they become big problems.
When to call your retina specialist
Here’s a quick checklist you can keep on your phone:
Sharp pain that doesn’t ease after an hour.
Sudden increase in redness or swelling.
Vision that gets noticeably worse – like a new dark spot.
Persistent floaters that last more than two days.
If any of those pop up, reach out immediately. Early intervention can save you from a full‑blown infection or pressure damage.
And remember, the journey doesn’t end after the first injection. Your doctor may suggest additional anti‑VEGF shots, a laser touch‑up, or a steroid boost based on how the retina heals. The key is staying proactive and keeping the conversation open.
Need a deeper dive into how injections can affect your eye over time? Our vitrectomy recovery guide walks you through post‑procedure care step by step, even if you never need surgery.
Bottom line: the best brvo treatment results come from a partnership between you, your doctor, and the habits you build every day. Follow the short‑term care tips, lock in the long‑term health habits, and you’ll give your eyes the best chance to stay clear and strong.
Conclusion
We've walked through what BRVO is, how it's diagnosed, the treatment options, and what to expect after a procedure. By now you probably feel a mix of relief and a lingering question: what's the next step for you?
First, schedule that dilated retinal exam if you haven't already. Early detection lets your doctor choose the most effective brvo treatment before swelling becomes stubborn. Remember, anti‑VEGF injections give the fastest visual recovery, laser saves you clinic trips, and steroids sit somewhere in between.
Second, keep the conversation alive with your retina specialist. Bring a short list of your priorities—speed, comfort, cost—and ask how each option aligns with them. A clear, two‑way dialogue turns a complex plan into a simple checklist you can follow.
Finally, protect your eyes every day. Control blood pressure, maintain healthy blood sugar, quit smoking, and stick to regular six‑month check‑ups. Those habits are the real backbone of long‑term success, no matter which brvo treatment you choose.
So, are you ready to take charge of your vision? Book that appointment, ask the right questions, and let the partnership between you and Dr. Rahul Dubey keep your sight sharp.
Remember, consistent care today means clearer sight tomorrow for you.
FAQ
What is brvo treatment and how does it work?
BRVO treatment targets the leaky blood vessels that form after a branch retinal vein blockage. Most often we use anti‑VEGF injections, which neutralise a protein that makes the retina swell. Laser photocoagulation seals the affected vein, and steroid implants calm inflammation when injections aren’t enough. The goal is simple: shrink macular oedema so you can see clearly again.
How many anti‑VEGF injections will I need?
Typically you start with one shot each month for three to six weeks. If the swelling eases, the schedule spreads out to every six to eight weeks. Some people stay on a maintenance plan for a year or longer, but many see stable vision after the first few visits. Your retina specialist will adjust the timing based on OCT scans.
Is laser therapy as effective as injections?
Laser can be just as effective for mild to moderate swelling, especially if you prefer fewer clinic trips. It’s a one‑time (or occasional) procedure, so you avoid the needle routine. However, the visual recovery is slower—often eight to twelve weeks—while injections usually deliver improvement within weeks. Your choice depends on how quickly you need clearer sight and how comfortable you are with needles.
What are the risks of steroid implants?
Steroid implants reduce injection frequency, but they raise two main concerns: cataract formation and increased eye pressure. About one in five patients notice a mild pressure rise that’s easily managed with eye drops. Cataracts develop slower than with repeated steroids, but they may still require surgery later. Your doctor will monitor pressure and lens clarity at every follow‑up.
Can I combine treatments for better results?
Yes, many clinicians start with anti‑VEGF to bring the swelling down fast, then add a laser spot to seal the leaking vein. This hybrid approach can cut down the total number of injections you need. It’s also useful if the edema returns after the initial course—switching to a steroid implant can give you another boost without restarting monthly shots.
How soon should I schedule my first appointment after noticing symptoms?
Don’t wait more than a week. The sooner you get a dilated retinal exam and OCT, the better the odds of preserving central vision. Early detection lets the doctor choose the most effective brvo treatment before the fluid hardens into scar tissue. If you’ve already seen a dark spot, call the clinic today and ask for an urgent slot.
What lifestyle changes support the success of brvo treatment?
Controlling blood pressure, blood sugar, and cholesterol is crucial—these factors drive vein blockages. Aim for a systolic below 130 mmHg, keep HbA1c under 7 % if you have diabetes, and maintain a healthy weight. Quit smoking, stay active with a daily walk, and keep up regular six‑month eye exams. Those habits reinforce the medical work and help prevent a repeat blockage.






Comments