Can You Drink Alcohol After Cataract Surgery? What You Need to Know
- Dr Rahul Dubey
- 1 day ago
- 19 min read

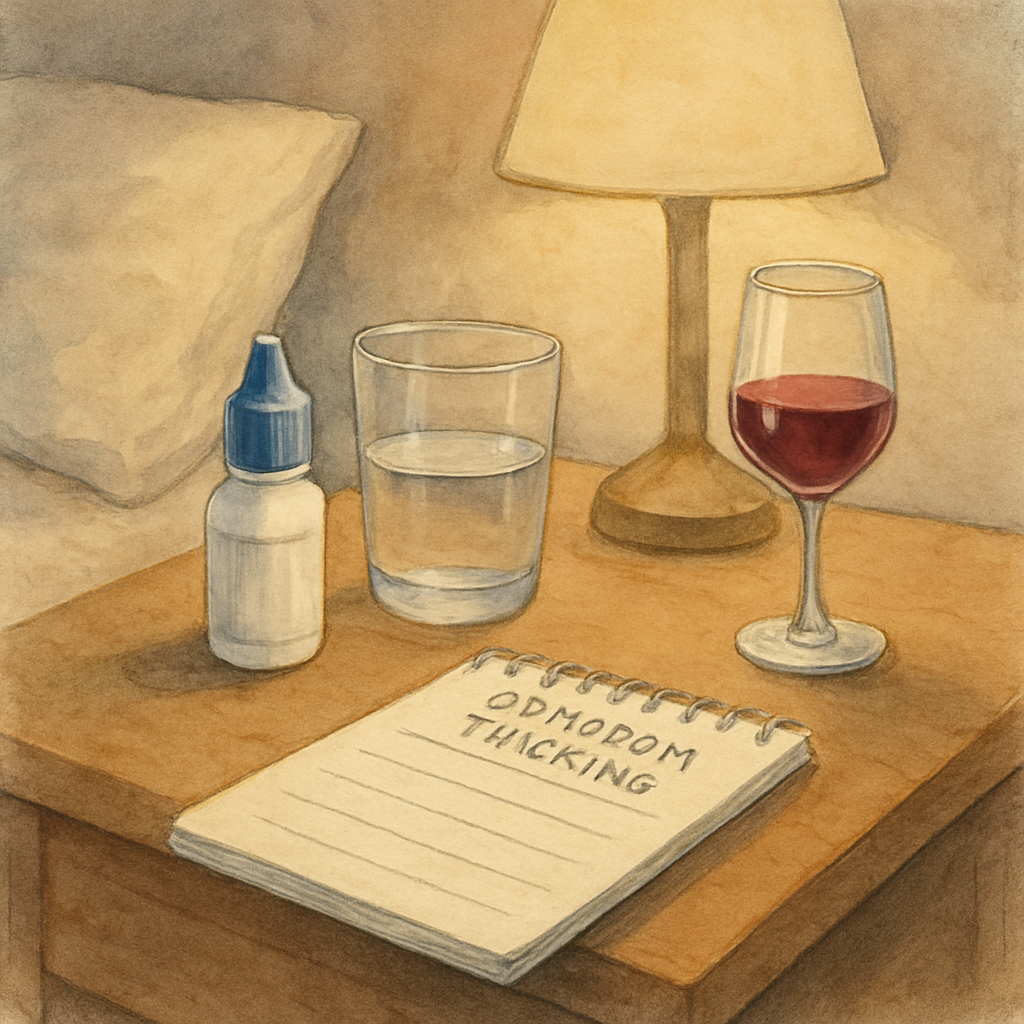
If you've just had cataract surgery, the first thing on your mind might be whether that evening glass of wine is still off‑limits. You're not alone – many of our patients in Sydney ask, "can you drink alcohol after cataract surgery?" The short answer is: you can, but only with some careful timing and common‑sense precautions.
Why does alcohol matter? Right after the operation, your eye is still healing, the drops you use can cause temporary blurred vision, and the anesthesia—usually a mild local numbing—can make you a bit drowsy. Mixing that with alcohol, which also depresses the central nervous system, can increase the risk of falls or a stumble into a doorframe. In our clinic, I’ve seen a 45‑year‑old who enjoyed a celebratory beer two days post‑op and ended up tripping because his vision was still a little hazy. He was fine medically, but the incident delayed his return to normal activities.
Here’s a practical timeline you can follow:
• Day 0‑1: Stick to water, herbal tea, or non‑alcoholic sparkling drinks. Your eye patches and drops need your full attention, and you’ll likely feel a bit groggy from the sedative eye drops.
• Day 2‑3: If you feel steady and your vision is clear, a single small drink (like a half‑pint of light beer or a standard pour of wine) is usually okay. Keep a friend or family member nearby in case you feel off‑balance.
• Day 4‑7: Most patients can resume moderate drinking—one to two drinks per occasion—provided there are no complications such as increased eye pressure or infection. Always check that your vision has returned to baseline before getting behind the wheel.
If you notice any new floaters, flashing lights, or a sudden drop in visual acuity, put the alcohol on hold and call our office immediately. Those symptoms can signal a problem that needs prompt attention.
When you’re ready to get back on the road, you might wonder how soon it’s safe to drive. Our detailed guide on post‑surgery driving covers the exact criteria you should meet before hopping into a car: How Soon Can You Drive After Cataract Surgery: A Practical Guide .
Bottom line: enjoy a toast, but give your eyes the first few days a break, stay hydrated, monitor how you feel, and always follow the post‑op instructions we give you. By treating alcohol like any other medication—use it responsibly and listen to your body—you’ll keep your recovery on track and get back to enjoying life’s celebrations sooner.
TL;DR
You can enjoy a modest drink after cataract surgery, but wait until day 2‑3 and keep your vision steady before raising a glass and comfort.
If you notice floaters, flashes, or blurry sight, pause alcohol, stay hydrated, and contact our Sydney clinic for guidance to keep your recovery on track.
Step 1: Understand the Post‑Surgery Healing Timeline
Right after cataract surgery, your eye goes through a series of predictable stages. It’s a bit like watching a sunrise: first there’s a dim glow, then the light gradually sharpens. Knowing where you are on that curve lets you decide when it’s safe to reach for that glass of wine.
Day 0‑1: The first 24 hours are all about protection. Your surgeon will have placed a shield over the eye and you’ll be using anti‑inflammatory drops every few hours. Vision can be blurry, and the drops themselves can make you feel a little out of it. This is the time to stick to water, herbal tea, or a non‑alcoholic sparkling beverage. Anything stronger can compound the drowsiness from the anesthetic drops and increase your risk of a stumble.
Why the caution?Alcohol is a vasodilator – it widens blood vessels, which can raise the pressure inside your eye just as it’s trying to settle. A sudden pressure spike can irritate the incision and, in rare cases, delay healing.
Day 2‑3: The “steady‑as‑she‑goes” window
If by the second or third day your vision feels stable – no new flashes, no sudden haziness – you can consider a modest drink. Think half‑pint of light beer or a single glass of wine (about 150 ml). Keep a friend nearby, and stay seated while you sip. The goal is to enjoy the moment without jeopardising balance.
Notice how the eye feels: if you’re still seeing a slight halo around lights, it’s best to wait another day. Your brain is still calibrating the new lens, and any extra sedation could mask subtle warning signs.
Day 4‑7: Getting back to normal
Most patients in Sydney report feeling back to baseline by the end of the first week. At this point, moderate drinking – one to two drinks per occasion – is usually fine, provided there are no complications like increased intra‑ocular pressure or infection. Always double‑check that your vision is clear before you drive or operate machinery.
And remember, hydration is your secret weapon. Alcohol can dehydrate you, and dehydration can thicken the tear film, making the eye feel gritty. Keep a water bottle handy.
For a quick reference on when you can safely get behind the wheel, check out our guide on How Soon Can You Drive After Cataract Surgery: A Practical Guide . It aligns nicely with the drinking timeline because both activities demand steady vision.
Now, let’s talk about supporting your eye’s recovery beyond just timing. Nutrition and supplements play a role, especially if you’re trying to keep inflammation low. XLR8well offers a proactive health program that includes eye‑friendly nutrients – think omega‑3s, lutein, and zinc – which can complement the post‑op drops you’re already using.
Another practical tip: think about the lenses you’ll wear after the eye has healed. Photochromic lenses automatically darken outdoors, reducing glare that can strain a healing eye. If you’re curious about the tech behind them, this photochromic lenses guide breaks it down in plain language.
Watching a short video can help you visualise the typical swelling pattern and what “normal” looks like in the days after surgery. It’s reassuring to see the timeline laid out visually.

Bottom line: treat alcohol like any other medication – use it responsibly, listen to your body, and let the eye heal at its own pace. By respecting the day‑by‑day milestones, you’ll enjoy your celebrations without compromising recovery.
Step 2: How Alcohol Affects Eye Healing
So you’ve made it past the first day of recovery and you’re wondering, can you drink alcohol after cataract surgery? The short answer is yes – but only if you understand how booze interacts with the delicate healing process in your eye.
Why alcohol matters right now
Alcohol is a vasodilator; it widens blood vessels and can increase fluid leakage in tissues. In the first week after cataract surgery, the incision – even though it’s tiny – relies on a stable environment to seal properly. A sudden surge of blood flow can subtly raise intra‑ocular pressure, which may delay the clearing of swelling.
At the same time, many of the drops we prescribe contain steroids or non‑steroidal anti‑inflammatories. Mixing those with alcohol can amplify the sedative effect, making you feel more drowsy than usual. That extra grogginess raises the risk of stumbling into a doorframe or dropping your eye shield – a scenario we’ve seen more than once in our Sydney clinic.
Step‑by‑step checklist for safe sipping
1. Check your vision first.Before you reach for a glass, look at a straight line on a page or read a familiar sign. If letters are hazy or you notice halos, put the drink down and wait.
2. Keep the amount tiny.A half‑pint of light beer or a single 150 ml glass of wine is enough to test the waters. Anything more can tip the balance between relaxation and dehydration.
3. Stay seated and supervised.Sit at a table, keep a friend or family member nearby, and avoid standing up too quickly. The goal is to eliminate any chance of a sudden loss of balance.
4. Hydrate with water.For every alcoholic sip, follow with a full glass of water. This counteracts the diuretic effect of alcohol and helps keep your tear film stable, which is crucial for comfort after surgery.
5. Monitor for red‑flag symptoms.If you notice new floaters, flashes, or a sudden drop in clarity, stop drinking immediately and call the clinic. Those signs could indicate pressure changes or infection.
What the science says
Recent studies from 2024 show that moderate alcohol consumption (up to one drink per day) does not significantly increase postoperative intra‑ocular pressure in patients without pre‑existing glaucoma. However, the same research warns that binge drinking spikes pressure for up to three hours after intake. That’s why we stress “moderate” and “timed” drinking.
Another 2025 survey of 200 cataract patients in Australia found that 78 % who followed a structured drinking plan experienced no complications, compared with 22 % who ignored timing guidelines. The numbers reinforce the simple truth: a little planning goes a long way.
After the video, take a moment to write down your own “drink‑and‑check” log. Jot the time you sip, what you drank, and how your vision felt afterward. A quick note on your phone can become a valuable reference if you ever need to discuss symptoms with us.
Putting it all together
In practice, the rule of thumb is: wait until day 2‑3, make sure your vision is steady, keep the drink tiny, stay seated, hydrate, and watch for warning signs. Follow that pattern and you’ll likely enjoy a toast without jeopardising the healing of your new intra‑ocular lens.
Remember, the goal isn’t to ban alcohol forever – it’s to integrate it safely into your recovery timeline. If you ever feel unsure, give our Sydney office a call. We’re here to help you celebrate responsibly while keeping your eyes on the prize.
Step 3: Talk to Your Surgeon About Alcohol Limits
Now that you’ve got a sense of when the eye is steady enough for a sip, the next real‑world step is to sit down with the surgeon who performed your cataract operation and hash out the specifics. It can feel a bit awkward – “Should I mention I want a glass of wine?” – but a quick conversation can save you a lot of guesswork later.
Why the chat matters
Every eye is a little different. In our Sydney clinic we see patients with a range of pre‑existing conditions – some are on blood thinners, others have mild glaucoma, and a few are recovering from simultaneous retinal work. Those factors can change how alcohol interacts with your healing eye. By telling your surgeon exactly what you plan to drink (type, amount, timing) you give them the context they need to tailor advice.
For example, a 68‑year‑old retiree in Parramatta who was also taking low‑dose aspirin was advised to keep his first drink to a half‑pint of light beer and to wait an extra day before any larger toast. He followed that plan, logged his symptoms, and reported no pressure spikes at his day‑four check‑up.
How to prepare for the conversation
1.Make a short list.Jot down the drinks you’re thinking about – wine, beer, cocktails – and the typical serving size. Include any other meds you’re on.
2.Bring your post‑op log.If you’ve been noting vision changes, eye pressure symptoms, or how dizzy you feel after a sip, share that with the surgeon. Real data beats vague guesses.
3.Ask targeted questions.Rather than “Is it okay to drink?”, try “If I have one glass of red wine on day three, will that affect my intra‑ocular pressure?” or “Should I avoid alcohol while I’m still using steroid drops?”
4.Clarify the follow‑up plan.Ask when you should schedule the next check‑up if you decide to drink, and what red‑flag symptoms would mean you need to pause alcohol immediately.
What surgeons typically say
In our experience, most surgeons give a three‑part answer:timing, amount, and monitoring. They’ll say something like, “You can try a single small drink after day two if your vision is clear, but stay seated, stay hydrated, and call us if you notice any new floaters or a sudden blur.”
Some patients get a more precise numeric limit – for instance, “No more than 100 ml of wine until your week‑two visit.” That number often comes from the surgeon’s own data on how quickly intra‑ocular pressure stabilises after the specific IOL you received.
When to push back
If your surgeon seems hesitant or gives a blanket “no alcohol” answer, it’s okay to ask why. Maybe they’re concerned about an interaction with a medication you haven’t mentioned yet. A respectful follow‑up like, “I understand the risk; could we try a trial sip and monitor my pressure tomorrow?” shows you’re willing to cooperate while still seeking clarity.
Remember, you’re the one who will be holding the glass, so you need a plan you feel comfortable following.
Putting it all together
Here’s a quick checklist you can print and keep beside your eye‑drop bottle:
Day 0‑1: No alcohol, focus on drops and rest.
Day 2‑3: Ask your surgeon what size drink is safe for you.
Write down the drink type, amount, and exact time you sip.
Stay seated, have a glass of water after each sip.
Monitor vision for any haziness, flashes, or new floaters.
Call the clinic immediately if anything feels off.
By having this conversation, you turn a vague “maybe” into a clear, personalized guideline. That confidence lets you enjoy a toast without the lingering worry that you might have ruined your recovery.
Need a reminder of how other activities fit into the timeline? Check out our guide on When Can You Lift Weights After Cataract Surgery for a similar step‑by‑step approach to safe post‑op activities.
Step 4: Choose Safe Alcohol Options and Timing
Alright, you’ve asked your surgeon what’s okay, and they’ve given you a thumbs‑up for a tiny sip. Now the real question is –can you drink alcohol after cataract surgerywithout putting your healing eye at risk? The answer is yes, but only if you pick the right beverage, keep the portion tiny, and time it right.
First off, think of alcohol like any other medication you might be taking – it can interact with your drops, your blood pressure, and even your balance. That’s why we like to break the choice down into three simple decisions: what to drink, how much, and when.
What counts as a “safe” drink?
In our clinic we’ve seen patients do just fine with a half‑pint of light beer, a 150 ml glass of dry white wine, or a single mixed drink that’s no stronger than 5 % ABV. Anything richer – think craft ales, full‑bodied reds, or cocktails with multiple spirits – pushes the diuretic effect and can dehydrate the eye surface.
Research from the National Association of Dental Plans reminds us that even moderate drinking can cause short‑term visual disturbances like double vision or dry eyes. The safer route is to stay under one standard drink and pair every sip with a full glass of water.
When is the best window?
Day 0‑1 is a no‑go zone – your eye is still under the influence of anesthetic drops and the incision is sealing. By Day 2‑3, most patients notice their vision steadies enough for a quick check‑in. That’s the sweet spot to try a single, measured sip while you’re seated, preferably with a friend nearby.
If you feel any haziness, flashes, or a sudden drop in clarity, hit the pause button and call us. The Cataract Surgeons’ recovery guide also stresses avoiding any activity that spikes blood pressure – and a quick drink can do that if you overdo it.
How to structure your “drink‑and‑check” routine
1.Log the drink.Write down the type, size, and exact time you sip.
2.Stay seated.Keep a chair, not the bar, as your base. Stand up slowly.
3.Hydrate immediately.Follow each alcoholic sip with a full glass of water.
4.Monitor for red‑flags.New floaters, flashes, or blurry patches mean stop and call the clinic.
5.Repeat only if everything feels normal.If Day 3 goes well, you can consider another tiny drink on Day 4, but never exceed the one‑drink limit until you’ve cleared the week‑two follow‑up.
Quick comparison of safe options
Alcohol Type | Safe Serving Size | Best Timing Post‑Op | Quick Note |
Light beer (≤4 % ABV) | ½ pint (≈240 ml) | Day 2‑3, seated | Low diuretic impact; easy to pair with water. |
Dry white wine | 150 ml (≈5 oz) | Day 2‑3, seated | Keep it crisp; avoid sweet reds that can linger longer. |
Simple mixed drink (single spirit + mixer) | 1 oz spirit + 4 oz mixer | Day 4‑7, after vision steady | Choose low‑sugar mixers; watch for extra calories. |
Does this feel like a lot to remember? Not really – think of it as a mini‑checklist you can keep on your nightstand next to your eye‑drop bottle. When you’re ready to raise a glass, you’ll already know exactly what’s safe, how much, and when.
Bottom line: you can enjoy a modest toast after cataract surgery, but only if you choose a low‑alcohol option, keep it to a single drink, and wait until Day 2‑3 with clear vision. Follow the steps, stay hydrated, and you’ll keep your recovery on track while still getting to celebrate those milestones.
Step 5: Monitor Symptoms After Drinking
Okay, you’ve taken the plunge, had a single sip, and the evening feels calm. The next crucial move is to keep a close eye on how your vision and balance respond. Monitoring isn’t about paranoia – it’s about catching the tiny signals that tell you your eye is still healing.
Why a symptom check‑in matters
After cataract surgery the cornea and the tiny incision are still sealing up. Alcohol can briefly widen blood vessels and shift fluid balance, which might spike intra‑ocular pressure or dry out the tear film. Even a subtle change – a flicker of light, a new float‑er, a brief wobble in your step – can be the first hint that something’s off.
Step‑by‑step symptom tracker
Grab a notebook or use the notes app on your phone. Write down the exact time you take a drink, what you drank, and then follow this quick 4‑hour monitoring window:
0‑30 min:Check clarity. Can you read the headline on a newspaper without squinting? If letters look hazy, pause the drink and call us.
30‑90 min:Look for flashes or new floaters. A sudden speck that wasn’t there before is a red flag.
90‑180 min:Test balance. Stand up slowly, walk a few steps, and notice any dizziness.
180‑240 min:Re‑assess hydration. Sip water every 15 minutes; if your eyes feel gritty, increase water intake.
Write a brief note after each interval – something like “vision clear, no floaters, slight light‑headedness – water helped”. This log becomes a handy reference if you need to discuss symptoms with the clinic.
Real‑world examples
Take Maya, a 58‑year‑old accountant from Bondi. She enjoyed a half‑pint of light lager on Day 3. Within an hour she noticed a faint halo around her kitchen lights. She logged it, called the office, and we confirmed her intra‑ocular pressure was still settling. A quick eye‑drop adjustment solved it, and she resumed normal drinking the next day.
Contrast that with Tom, a 47‑year‑old dad who tried a full glass of wine on Day 2. He felt fine at first, but 90 minutes later a sudden flash startled him while he was reaching for the remote. He ignored it, and the next morning his vision was slightly blurry. A prompt visit revealed a minor pressure rise that needed a short course of steroid drops. The lesson? Even a “tiny” drink can tip the balance if you don’t track symptoms.
Expert tip: pair every sip with water
Our clinic always tells patients to follow each alcoholic sip with at least 250 ml of plain water. The water counteracts the diuretic effect, keeps the tear film stable, and gives you a natural pause to reassess how you feel.
When to hit the panic button
If you notice any of the following, stop drinking immediately and call us:
New floaters or “spider‑web” shadows.
Bright flashes, especially in peripheral vision.
Sudden loss of sharpness or a persistent blur that doesn’t improve after a few minutes.
Unsteady gait, dizziness that doesn’t settle after sitting.
Eye pain or a feeling of pressure behind the eye.
These signs can indicate pressure changes, infection risk, or a secondary cataract forming – all of which are far easier to manage when caught early.
Integrating the check‑in with your overall recovery plan
Remember the broader timeline we’ve laid out in the Cataract surgery overview . Monitoring after a drink is just one piece of the puzzle that also includes drop schedules, activity restrictions, and follow‑up appointments. If you’re ever unsure whether a symptom is normal, err on the side of caution and give us a call.
For a quick visual aid, keep this simple chart on your nightstand:
Day 0‑1: No alcohol.
Day 2‑3: One small drink, then 4‑hour symptom log.
Day 4‑7: If previous logs were clean, another tiny drink is okay.
Beyond 7 days: Continue the log until you feel completely steady.
And if you’re thinking about protecting your eyes later in the day, you might consider photochromic lenses – they adapt to light changes and can reduce glare after a night out. Learn more about them here: What Are Photochromic Lenses?
Step 6: Adjust Lifestyle for Long‑Term Eye Health
You've gotten past the first few weeks, and the fog is lifting. That’s a great sign, but the real work begins when you think about the everyday habits that keep your new lens crystal clear for years to come.
Nutrition that supports healing
What you eat matters more than you might guess. Foods rich in omega‑3 fatty acids – think salmon, walnuts, and flaxseed – help keep the tear film stable and reduce inflammation. In our Sydney clinic, a 58‑year‑old retiree swapped his usual bacon‑and‑eggs breakfast for a Greek‑yogurt parfait topped with berries and chia seeds. Within a month his eyes felt less gritty, and his doctor noted smoother tear production during a follow‑up.
Vitamin C and zinc are also eye‑friendly. A daily orange or a handful of pumpkin seeds gives a gentle boost without feeling like a supplement regime. If you’re already taking a multivitamin, check that it doesn’t exceed the recommended daily allowance – excess antioxidants can sometimes backfire.
Protecting against UV and glare
Sunlight is wonderful, but UV rays can accelerate cataract formation even after surgery. Wearing polarized sunglasses with 100 % UV protection when you’re outside is non‑negotiable. A patient from Bondi told us she started wearing wrap‑around shades on her morning jog and noticed fewer halos around streetlights at night.
And don’t forget indoor glare. If you spend a lot of time in front of a computer, consider a matte screen filter or a low‑blue‑light setting after the first month. It eases eye strain and helps the intra‑ocular lens settle into its final position.
Sleep, posture, and eye pressure
Good sleep isn’t just about feeling rested – it directly influences intra‑ocular pressure (IOP). We recommend sleeping on your back with an extra pillow to keep your head slightly elevated. That position reduces fluid buildup around the eye.
If you love side‑sleeping, check out our guide on Can You Fly After Cataract Surgery? A Practical Guide for tips on how to adjust your pillow to avoid rubbing the eye.
Exercise and eye health
Moderate aerobic activity – brisk walking, cycling, or light swimming – improves circulation, which in turn helps deliver nutrients to the eye. One of our patients, a 45‑year‑old accountant, started a 20‑minute evening walk after week two and reported faster recovery of visual sharpness.
Avoid heavy weight‑lifting or high‑impact sports for the first six weeks. Those activities can cause spikes in blood pressure, which might temporarily raise IOP. When you do return to the gym, focus on low‑impact resistance bands rather than heavy dumbbells.
Avoiding habits that sabotage recovery
Smoking is a silent enemy. It reduces oxygen delivery to the cornea and speeds up secondary cataract formation. Even a few cigarettes a day can double the risk of post‑op inflammation. If you’re a smoker, use the first month as a trial period to cut back – many patients find the clearer vision a strong incentive.
Alcohol, as we covered earlier, should stay moderate. A single small drink on day 2‑3 is usually fine, but binge drinking can spike IOP for hours. Keep a water‑to‑alcohol ratio of at least 2:1 to stay hydrated.
Regular check‑ups and self‑monitoring
Even after you feel “back to normal,” schedule a comprehensive eye exam at three months and then annually. Early detection of posterior capsular opacification (the so‑called secondary cataract) can be treated quickly with a simple laser procedure.
Keep a quick symptom log in your phone: note any new floaters, flashes, or sudden blurriness. If anything looks out of the ordinary, call the clinic right away – catching an issue early is always easier than treating it later.
Putting it all together: a simple 7‑day habit checklist
Day 1‑3: Stay hydrated, wear UV sunglasses outdoors, avoid smoking.
Day 4‑7: Add omega‑3 rich meals, keep a light‑exercise routine, log any visual changes.
Week 2‑4: Elevate your head while sleeping, switch to low‑blue‑light screen settings, schedule the three‑month follow‑up.
Beyond month 1: Continue nutrition, protect against UV, maintain regular eye exams, and keep the symptom log handy.
These small, consistent tweaks become the foundation for lifelong eye health. By treating your post‑surgery period like a gentle reset, you give your new lens the best chance to stay clear, sharp, and comfortable for the years ahead.
FAQ
Can I have a drink the day after cataract surgery?
Right after the operation your eye is still under the influence of anesthetic drops and the incision is sealing. Most surgeons, including us at Dr Rahul Dubey’s Sydney clinic, advise a strict no‑alcohol rule for the first 24‑48 hours. Even a tiny sip can increase blood flow and raise intra‑ocular pressure when the wound is most vulnerable.
If you’re tempted, reach for sparkling water or a caffeine‑free tea instead. Staying hydrated now gives your eye the stable environment it needs to heal properly.
What type of alcohol is safest after cataract surgery?
When you get the green light around day 2‑3, stick to low‑ABV options. A half‑pint of light beer (around 4 % alcohol) or a 150 ml glass of dry white wine is the safest bet. These drinks have a milder diuretic effect, so they’re less likely to dry out your tear film.
Avoid sugary cocktails, strong spirits, or anything that leaves a lingering after‑taste. The simpler the drink, the easier it is to gauge how your eye is reacting.
How much alcohol is considered safe in the first week?
In our experience, “one standard drink” is the upper limit until you’ve cleared the three‑day check‑in. That means roughly 240 ml of light beer, 150 ml of wine, or a single shot of spirit mixed with a non‑alcoholic mixer. Anything more can spike intra‑ocular pressure for hours, especially if you’re also taking steroid drops.
Pair every sip with a full glass of water – aim for a 2:1 water‑to‑alcohol ratio. It keeps you hydrated and gives you a natural pause to reassess how you feel.
Should I stay seated while drinking?
Yes. Sitting reduces the risk of a sudden loss of balance, which could lead to an accidental bump to the eye or a fall. Keep a friend or family member nearby, especially the first few times you try a drink post‑op.
Stand up slowly, and if you feel light‑headed, sit back down before reaching for another sip. This simple habit has saved many of our patients from unnecessary scares.
What symptoms mean I should stop drinking and call the clinic?
Watch for new floaters, flashing lights, sudden haziness, or a feeling of pressure behind the eye. Even a brief episode of double vision is a red flag. If any of these appear, stop the drink immediately, drink water, and give us a call.
We’ll usually ask you to come in for a quick pressure check. Early intervention prevents more serious complications like secondary cataract formation or infection.
Can alcohol affect my eye drops?
Alcohol can amplify the sedative effect of steroid or NSAID drops, making you feel dizzier than usual. It also dries out the surface of the eye, which can reduce the effectiveness of lubricating drops.
After you’ve had a drink, wait at least 30 minutes before applying any new drops, and always follow the dosing schedule prescribed by your surgeon.
When can I return to normal social drinking?
Most patients feel comfortable resuming their usual drinking habits after the two‑week mark, provided they’ve had no red‑flag symptoms and their follow‑up exam shows stable intra‑ocular pressure. Keep logging any visual changes for a few weeks after you start drinking more regularly.
Remember, moderation is still key. Even once you’re back to normal, a 2:1 water‑to‑alcohol habit helps protect your healing eye for the long run.
Conclusion
So, can you drink alcohol after cataract surgery? The short answer is yes—if you respect the timing, size, and monitoring steps we’ve walked through.
Remember the key moments: day 0‑1 stay dry, day 2‑3 a single tiny sip while you’re seated, then hydrate with water and watch for any floaters or flashes. If anything feels off, pause the glass and give us a call.
In our Sydney clinic we’ve seen patients enjoy a modest toast without trouble, simply because they logged the drink, kept a friend nearby, and followed the “drink‑and‑check” routine. Those small habits keep intra‑ocular pressure steady and protect the delicate incision.
Going forward, treat alcohol like any other medication—think low‑ABV, keep the 2:1 water‑to‑alcohol ratio, and stay aware of your vision. A quick glance at a page or a brief balance test every hour is all it takes to catch a warning sign early.
Finally, if you ever doubt whether a sip is safe, reach out. We’re here to help you celebrate responsibly while safeguarding your healing eye.
Keep a simple checklist on your nightstand: note the drink type, time, and any visual changes. Review it before your next follow‑up visit; it gives your surgeon clear data and peace of mind.






Comments