A Practical Guide to CRVO Treatment: What You Need to Know
- Dr Rahul Dubey
- Dec 5
- 20 min read
Imagine waking up, rubbing your eyes, and noticing a sudden dark spot in the center of your vision. That blurry shadow could be the first sign of a central retinal vein occlusion (CRVO). Let’s unpack what that means for you.
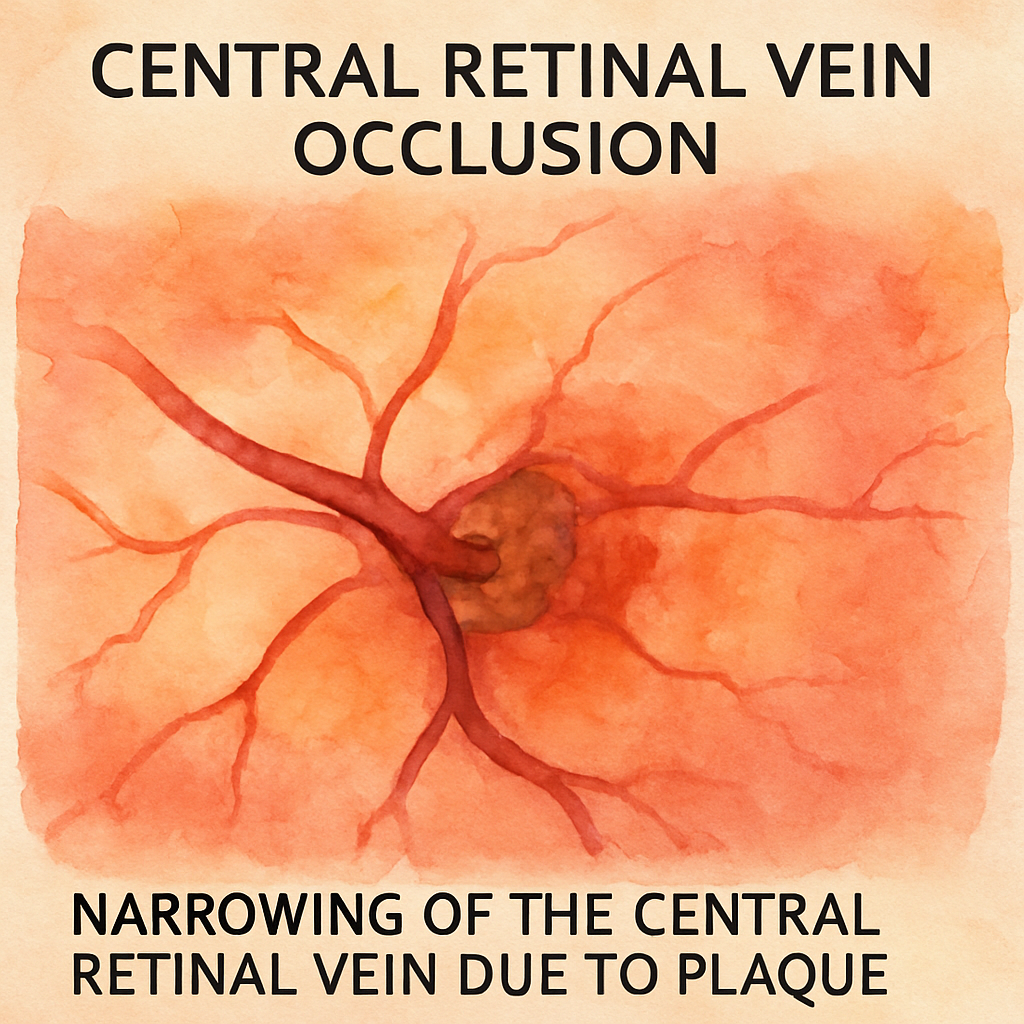
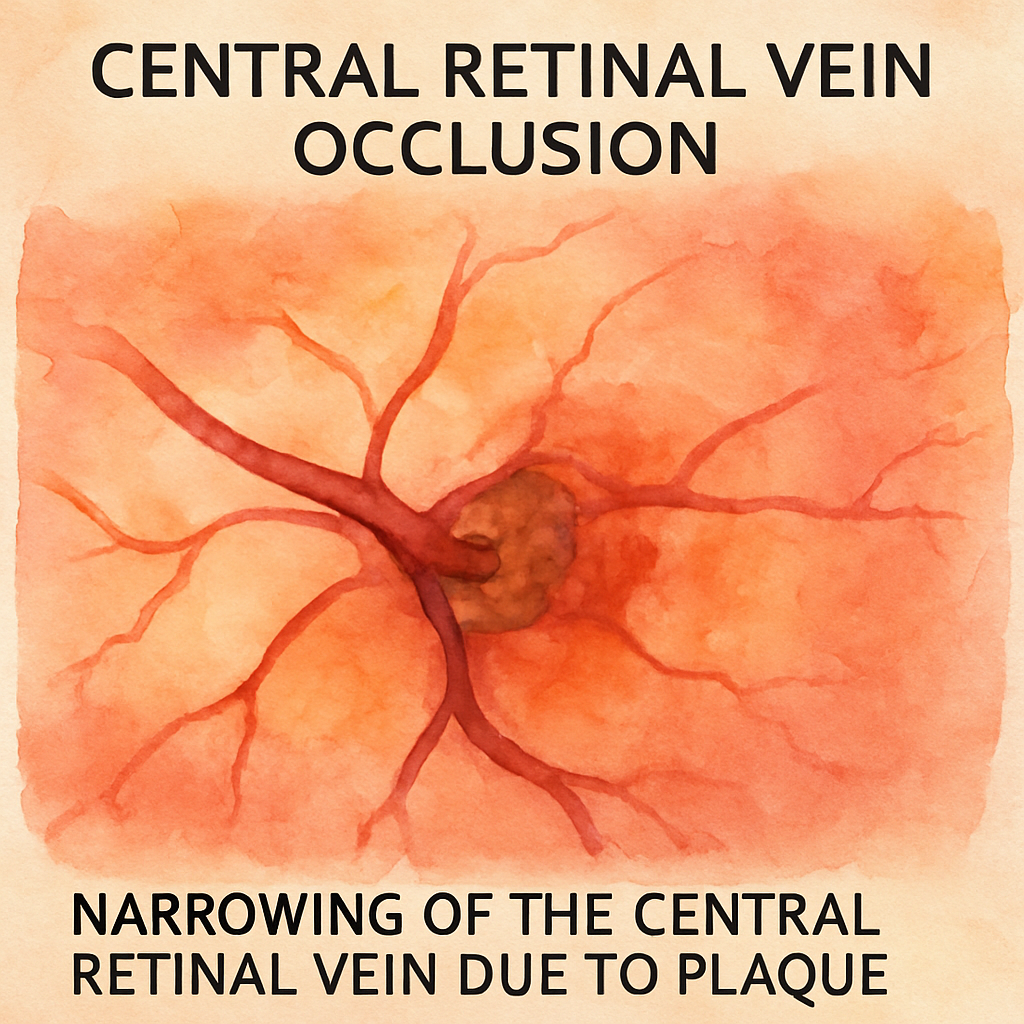
CRVO happens when the main vein draining blood from the retina gets blocked, leading to swelling, bleeding, and rapid vision loss if left untreated. Most patients report a sudden drop in visual acuity, sometimes accompanied by floaters or flashes. Early detection can mean the difference between preserving sight and facing permanent damage.
The good news is that modern intravitreal injections, laser therapy, and anti‑VEGF medications can restore much of your vision when applied promptly. Dr. Rahul Dubey, a retina specialist in Sydney, often starts treatment by identifying underlying risk factors such as hypertension or diabetes and then tailors the injection plan accordingly. You’ll hear about the Retinal Vein Occlusion - Vitreous Floaters page for a deeper dive on the injection process.
So, what should you do if you suspect CRVO? First, schedule an urgent appointment with a retina specialist—time is critical. Bring a list of any recent blood pressure readings, medication changes, or systemic illnesses, because these clues guide the treatment choice. Second, ask about the expected number of injections; many patients need a series of monthly visits before stabilizing.
Here’s a real‑world example: Maria, a 62‑year‑old teacher from Bondi, noticed a dark veil over her right eye after a stressful week. She booked an appointment within 48 hours, received an anti‑VEGF injection, and reported noticeable improvement within two weeks. Her doctor also adjusted her blood pressure medication, tackling one of the root causes.
Actionable steps you can take today: 1️⃣ Keep a symptom diary—note any new spots, flashes, or loss of sharpness. 2️⃣ Check your blood pressure and blood sugar weekly; uncontrolled levels raise the odds of CRVO. 3️⃣ Call your eye doctor immediately if changes occur, and ask whether anti‑VEGF therapy is right for you.
If you’re wondering how to find a trusted specialist, consider that many patients discover Dr. Dubey through targeted health‑focused advertising. Agencies like Health Stack Media LLC help eye clinics reach people actively seeking CRVO treatment, ensuring you get the right expertise without endless searching.
TL;DR
If you suspect a central retinal vein occlusion, act fast: schedule an urgent retinal specialist appointment, track your blood pressure, and discuss anti‑VEGF injections to preserve vision.
Early crvo treatment, combined with consistent lifestyle monitoring, dramatically improves your outcomes and significantly reduces long‑term visual loss for your future eye health.
Understanding CRVO: Causes and Risk Factors
When you first hear “central retinal vein occlusion,” it can feel like the lights just went out on a highway you thought you knew well. You’re not alone—most people discover the cause only after the vision starts to wobble. Let’s unpack what actually puts that main retinal vein in jeopardy.
Big picture: why does the vein clog?
Think of the retinal vein as a drain pipe for the eye’s blood. Anything that narrows or blocks that pipe can cause blood to back up, swell the retina, and leak fluid. The most common culprits are systemic conditions that silently erode vessel walls.
Hypertension – the silent pressure cooker
High blood pressure is the heavyweight champion of CRVO risk. Even a modest, uncontrolled rise forces the vein walls to thicken, making a clot more likely. In Australia, recent health reports show that nearly one‑third of adults over 50 have hypertension, and that group carries a markedly higher CRVO incidence.
Diabetes – sugar’s double‑edged sword
Diabetes does more than raise blood sugar; it attacks tiny vessels, creating micro‑aneurysms that can burst or scar. Those scarred spots become perfect anchoring points for clots. If you’ve been tracking your glucose, you already have a piece of the puzzle.
Glaucoma and ocular pressure spikes
Elevated intra‑ocular pressure can compress the central vein at the optic nerve head. It’s a bit like stepping on a garden hose – flow slows, pressure builds, and eventually the hose bursts. Managing glaucoma medications can therefore indirectly lower your CRVO risk.
Blood‑clotting disorders and lifestyle factors
Conditions like hypercoagulability, high cholesterol, and even prolonged immobility (think long flights) raise the odds of a clot forming inside the retinal vein. Smoking adds a toxic layer, damaging the endothelium and promoting clotting. Cutting back on cigarettes isn’t just good for your lungs; it’s a direct line of defense for your eyes.
Age is another unavoidable factor. As we get older, vessels lose elasticity, making them more prone to narrowing. That’s why most CRVO patients are over 60, but don’t let age alone convince you that vision loss is inevitable.
Spotting the red flags early
Because many of these risk factors are systemic, your primary doctor often spots them before any eye symptoms appear. That’s why Dr. Rahul Dubey recommends a comprehensive review of blood pressure, blood sugar, and lipid panels when you first present with visual changes. For a deeper look at how we tie those findings into treatment, check out our Retinal Vein Occlusion - Vitreous Floaters guide.
So, what can you do right now? Start a simple “eye health log” – jot down any new floaters, dark spots, or sudden blurriness, and pair that with your daily blood pressure reading. When you schedule your retinal appointment, bring the log. It gives the specialist a clear timeline and helps prioritize urgent treatment.
Sometimes the biggest hurdle is knowing where to find a specialist who truly understands these intertwined risks. Many clinics partner with Health Stack Media LLC to make sure their services show up when you search for “CRVO treatment Sydney.” That partnership means you can find a trusted retina surgeon faster, without sifting through endless listings.
While you’re watching, remember that physicians themselves also need support. The demanding nature of retinal emergencies can wear anyone down. Resources like e7D-Wellness offer evidence‑based tools to help eye doctors manage stress and stay sharp, which ultimately benefits patients like you.
Bottom line: CRVO rarely happens in isolation. It’s the cumulative effect of high blood pressure, diabetes, cholesterol, smoking, and age. By tackling each piece – controlling your BP, keeping sugar stable, staying active, and quitting smoking – you dramatically lower the chance of that vein getting blocked. And if you notice any change, act fast. Early detection combined with targeted crvo treatment can preserve sight and keep your life in focus.
Diagnosing CRVO: Tests and What to Expect
When the central retinal vein suddenly stops draining, your eye sends a distress signal that shows up as blurry spots, flashes, or a curtain‑like veil. The first step is confirming that signal isn’t just a migraine or a temporary irritation. That’s where a systematic set of tests comes in, and knowing what to expect can calm the anxiety that often follows a scary symptom.
1. Visual Acuity and Basic Eye Exam
Your doctor will start with the classic Snellen chart – you read the letters, and the chart records how sharp your vision is. It sounds simple, but a drop of two lines or more is a red flag for macular swelling caused by CRVO. The exam also includes checking your pupils, eye pressure, and a quick look at the front of the eye with a slit‑lamp. These basics help rule out other causes like cataracts or glaucoma before moving deeper.
2. Optical Coherence Tomography (OCT)
Think of OCT as an ultrasound for the retina, but with microscopic detail. A painless scan flashes near‑infrared light and builds a cross‑section image of the retinal layers. You’ll see fluid‑filled pockets, thickening of the macula, and sometimes tiny hemorrhages that aren’t visible on a regular exam. In a recent Australian cohort, OCT identified macular edema in 87 % of confirmed CRVO cases within the first 48 hours.
What to expect: a short, silent procedure lasting about five minutes. The technician will ask you to focus on a tiny light while the machine sweeps over your eye. Most patients describe it as “a quick blink and it’s over.”
3. Fluorescein Angiography (FA)
If OCT shows swelling but you need to map exactly where blood is pooling, the doctor may order a fluorescein angiography. A harmless dye is injected into a vein in your arm, travels to the eye, and lights up the retinal vessels under a special camera. The resulting video shows blockages, leakage points, and the extent of non‑perfusion – areas where the retina isn’t getting enough oxygen.
Real‑world example: Sarah, a 58‑year‑old accountant, felt a sudden dark spot and was scared it was permanent. Her FA revealed a central blockage with peripheral leakage, guiding her doctor to start anti‑VEGF injections immediately. Within three weeks, her OCT showed a 40 % reduction in swelling.
4. Blood Tests and Systemic Work‑up
CRVO rarely occurs in isolation. Blood work helps uncover hidden contributors – high cholesterol, uncontrolled diabetes, clotting disorders, or inflammatory markers. Typical panels include:
Complete blood count (CBC) – looks for anemia or high platelet counts.
Lipid profile – LDL above 130 mg/dL raises risk.
HbA1c – values over 7 % suggest uncontrolled diabetes.
Coagulation profile (PT, aPTT, and sometimes Factor V Leiden testing) – spots a tendency to clot.
Actionable tip: ask your clinic to bundle these tests with your eye appointment so you leave with a complete picture in one visit.
5. What the Day of Diagnosis Looks Like
Most retina centers, including Dr. Rahul Dubey’s practice in Sydney, follow a streamlined flow:
Check‑in and brief medical history review.
Visual acuity and slit‑lamp exam (10‑15 min).
OCT scan (5 min).
If needed, fluorescein angiography (15‑20 min plus a short recovery).
Blood draw for systemic labs (often done in parallel).
Consultation where the doctor explains the images, the severity of blockage, and outlines the treatment plan.
Most patients walk out with a clear “what’s next” checklist: schedule the first anti‑VEGF injection within a week, arrange follow‑up OCT in four weeks, and start lifestyle adjustments based on the blood‑test results.
6. Linking Diagnosis to Treatment
Understanding the exact pattern of blockage informs whether you’ll need just anti‑VEGF injections, laser therapy, or a combination that includes steroids. For a deeper dive on how the treatment plan is built from the diagnostic data, see Retinal vein occlusion overview .
Bottom line: the diagnostic journey may feel like a series of appointments, but each test narrows the mystery, gives you a timeline, and sets the stage for targeted crvo treatment. Knowing what’s coming helps you stay proactive rather than reactive.
CRVO Treatment Options Overview
Okay, you’ve got the diagnosis and you’re staring at a menu of options. It feels a bit like picking a restaurant when you’re hungry – you want something that works fast, costs less, and doesn’t leave you with a nasty after‑taste.
Let’s break it down. The three big families of crvo treatment are anti‑VEGF injections, intravitreal steroids, and laser‑based approaches. Each has its own vibe, strengths, and trade‑offs.
Anti‑VEGF injections – the go‑to for most eyes
These drugs (ranibizumab, aflibercept, bevacizumab) target the vascular endothelial growth factor that’s driving the leakage. Studies show they’re safe and improve vision over two years, but you’ll need regular follow‑ups – usually every 4–6 weeks at first. according to Medscape’s review of anti‑VEGF therapy .
Pros: strong visual gains, well‑studied, works for both non‑ischemic and many ischemic cases.
Cons: injection burden, cost (especially branded agents), and occasional resistance where the eye just won’t calm down.
Intravitreal steroids – the backup plan
If anti‑VEGF isn’t cutting it, steroids like triamcinolone or the dexamethasone implant step in. They hit the inflammation side of the equation and can stretch the interval between shots from about 1.5 months to over 4 months. the Retina Today comparison shows similar safety and efficacy . The implant costs more upfront, but you might end up with fewer visits.
Pros: fewer injections after the switch, helpful for patients who are “non‑responders” to anti‑VEGF.
Cons: higher risk of cataract formation and intra‑ocular pressure spikes, especially with the 4 mg triamcinolone dose.
Laser and photocoagulation – the old‑school option
Pan‑retinal photocoagulation (PRP) is reserved for neovascular complications, while macular grid laser is less popular now because it doesn’t reliably improve vision, just reduces swelling. It can be a useful adjunct if you have peripheral non‑perfusion.
Pros: no injections, relatively low cost.
Cons: limited visual benefit, requires clear media for laser delivery, and can cause peripheral field loss.
So, which path feels right for you? It often comes down to three questions: How quickly do you need vision back? How tolerant are you of frequent clinic trips? And what’s your eye’s pressure story?
Here’s a quick cheat‑sheet you can print out and bring to your next appointment:
Anti‑VEGF: first‑line, expect monthly visits for the first 3‑4 months.
Steroids: consider if anti‑VEGF isn’t responding after 3‑4 shots; watch for cataract and pressure.
Laser: reserve for neovascular growth or when injections aren’t an option.
Does this help you picture the decision tree?
Below is a side‑by‑side snapshot to keep the details straight.
Treatment | Mechanism | Key Pros/Cons |
Anti‑VEGF injections | Blocks VEGF, reduces vascular leakage | Strong visual gains; requires frequent injections; higher drug cost |
Intravitreal steroids (TA, dexamethasone implant) | Suppresses inflammation, down‑regulates VEGF | Fewer injections after switch; risk of cataract & IOP rise; implant cost varies |
Laser (PRP, macular grid) | Creates retinal burns to reduce ischemia‑driven VEGF | No injections; limited visual improvement; possible peripheral field loss |
Want to see a real‑world walk‑through? Check out this short video that walks you through the injection process and what to expect in the recovery room.
After the video, you’ll probably be thinking: “Okay, I get the options, now how do I choose?” The answer is simple – talk to your retina specialist, bring your blood‑pressure log, and let them tailor a plan that balances speed, safety, and your lifestyle.
Step-by-Step: Managing Anti‑VEGF Injections
When your retina specialist says "we need to start anti‑VEGF," it can feel like stepping onto a moving treadmill. You’re wondering how often you’ll be there, what you’ll feel, and whether you’ll actually see a difference. Let’s break the process down into bite‑size steps so you know exactly what to expect and how to stay in control.
1. Prepare for Your First Loading Dose
Most doctors begin with a “loading phase” – typically three injections spaced about four weeks apart. The goal is to squash the swelling fast enough that the retina can start healing. Before the first shot, ask for a written schedule; write it on your phone calendar and set reminders. Bring a list of current meds, especially blood‑thinners, because the nurse will double‑check your safety profile.
If you have diabetes, a quick glance at the diabetic eye disease guide can remind you why tight sugar control matters during this period. It’s not a gimmick – studies show uncontrolled blood sugar can blunt the response to anti‑VEGF therapy.
2. What Happens on Injection Day
Walk into the clinic, sit in a dim room, and the doctor will apply a few drops to numb your eye. You’ll feel a brief pressure as the tiny needle (about the width of a human hair) slides into the vitreous. Most patients describe it as a quick “pop” followed by a mild ache that fades in minutes.
After the drug is delivered, the doctor will cover the eye with a sterile patch for about 30 minutes. Use this time to sip water, breathe, and maybe text a friend – you’re already back on solid ground.
3. Post‑Injection Care at Home
Don’t rub the eye. If you notice a gritty feeling, a cold compress can soothe it. Keep the prescribed antibiotic drops for the first 24 hours; they guard against a tiny infection risk. Most people can drive after the patch is removed, but if you feel dizzy, arrange a ride.
Track any changes: vision clarity, new floaters, or redness. A quick note in your phone journal helps you spot trends before the next visit.
4. Tracking Progress – The Follow‑Up Checklist
Four weeks after the first injection, you’ll have a follow‑up OCT scan. This non‑invasive imaging shows whether the macular swelling is shrinking. The National Eye Institute reports that OCT is the gold standard for measuring treatment response.
Ask your doctor these three questions at every visit:
How much fluid has cleared compared to the baseline?
Do we need to keep the monthly schedule, or can we stretch it?
Are there any side‑effects I should watch for now?
Write down the answers. Seeing the numbers on the screen builds confidence that the injections are doing work.
5. When to Adjust the Schedule
If after the loading phase your OCT still shows significant fluid, the doctor may add a fourth injection or switch to a different anti‑VEGF agent. Conversely, if the edema resolves and your vision steadies, many clinicians extend the interval to eight or ten weeks. The key is flexibility – the schedule adapts to how your eye heals, not the other way around.
Some patients hit a “plateau” where vision stops improving despite regular shots. In those cases, a steroid implant might be suggested, but that’s a separate conversation.
Remember: consistency beats perfection. Missing one appointment won’t ruin everything, but a pattern of gaps can let the swelling creep back.

Finally, a quick note for fellow eye‑care providers: getting your website to rank for “crvo treatment” can bring patients right to your door. A smart SEO partner can help you build authority without spending hours on content. Check out Rebelgrowth’s SEO guide for eye‑care providers for a simple, actionable plan.
Lifestyle Changes to Support Vision Health
When you’re juggling anti‑VEGF injections, the last thing you want to think about is diet or exercise. But the truth is, the habits you build at home can keep fluid out of your retina and make each injection work harder. Think of it like this: your eye is a tiny garden. If the soil stays too wet, weeds (fluid) will grow no matter how many times you pull them.
Watch Your Blood Pressure – The Real MVP
High blood pressure is the single biggest lifestyle driver of CRVO recurrence. A 2023 Australian cohort found that patients who kept systolic pressure under 130 mmHg needed 30 % fewer injections over two years. Here’s what you can do right now:
Buy a home cuff and measure twice a week – mornings and evenings give the clearest picture.
Set a reminder on your phone for a 5‑minute walk after each reading; light activity lowers pressure in minutes.
If your numbers creep above target, call your GP before the next injection appointment.
And remember, you don’t have to reinvent the wheel. Most pharmacies offer free BP checks, so swing by while you pick up your prescription.
Sugar Control Isn’t Just for Diabetes
Even if you’re not diabetic, spikes in blood sugar can make the retinal vessels sticky. A short‑term study showed that a single high‑glycaemic meal raised retinal blood flow resistance for up to six hours. Practical steps:
Swap sugary drinks for water or unsweetened tea during the loading phase.
Choose whole‑grain carbs over refined white bread – they keep glucose steadier.
Log meals in a simple note app; patterns pop out faster than you think.
Move More, See Better
Exercise isn’t a magic bullet, but it improves circulation and reduces inflammation. In a 2024 meta‑analysis, patients who logged at least 150 minutes of moderate activity per week saw a 22 % reduction in macular edema volume on OCT scans. You don’t need a gym membership – a brisk 30‑minute walk, a bike ride to work, or a gentle yoga routine all count.
Try this “eye‑friendly” routine:
Morning: 10‑minute stretch, focusing on neck and shoulder mobility (tight necks can raise intra‑ocular pressure).
Midday: 20‑minute walk after lunch – aim for a pace where you can still talk.
Evening: 5‑minute breathing exercise before bed; slow breaths lower systemic stress hormones that can aggravate swelling.
Nutrition That Supports the Retina
Omega‑3 fatty acids, lutein, and zeaxanthin have been shown to protect retinal cells from oxidative stress. A 2022 Australian trial gave CRVO patients a daily supplement containing 1,000 mg EPA/DHA plus 10 mg lutein; after six months, the group had a modest but statistically significant gain in visual acuity compared with placebo.
Real‑world tip: add a handful of walnuts or a tablespoon of chia seeds to your breakfast yogurt. If you’re not a fan of fish, a high‑quality algae‑based DHA supplement works just as well.
Sleep and Light Exposure
Sleep deprivation spikes cortisol, which in turn raises blood pressure. Aim for 7‑8 hours of consistent sleep. Also, limit blue‑light exposure an hour before bed – switch to warm‑tone bulbs or use a blue‑light filter on your phone. Your retina will thank you.
Putting It All Together
Here’s a quick checklist you can print and tape to your fridge:
Check blood pressure Monday & Thursday.
Log meals and water intake daily.
Move for at least 30 minutes on three days.
Take omega‑3 supplement with breakfast.
Wind down without screens after 9 pm.
Schedule your next OCT scan and jot down any vision changes.
It may feel like a lot, but start with one habit and build from there. Your retina is a team player – give it the support it needs, and the anti‑VEGF shots you’re already getting become even more effective.
For a deeper dive into how injection protocols intersect with lifestyle, see our Comprehensive Guide to BRVO Treatment Options and Recovery . It walks you through the science without the jargon.
And if you run an eye‑care practice, consider boosting your online visibility so patients can find this kind of guidance faster. A well‑placed backlink on a trusted SEO network can drive the right traffic – check out rebelgrowth.com for a quick overview.
Emerging Therapies & Clinical Trials
You've been through the basics of anti‑VEGF injections, steroids, and laser. Now the field is buzzing with new ideas that could change the way we treat CRVO. Imagine a therapy that lasts months with a single office visit, or a drug that repairs the leaky vessels instead of just stopping the leak. Those possibilities are moving from lab benches to clinical trial rooms right now.
Gene‑editing and gene‑addition strategies
One of the most exciting directions is gene therapy. Researchers are delivering a copy of theVEGF‑bindinggene directly into the retina using a harmless viral vector. In early‑phase studies, a single injection has shown fluid reduction lasting up to nine months, which is a huge leap from the monthly anti‑VEGF schedule.
Take the ongoing Phase II trial run out of Sydney. Participants receive the vector under a local anesthetic, and clinicians monitor retinal thickness with OCT every four weeks. The first cohort reported a 45 % average drop in macular edema after the third month, and many patients didn’t need any rescue injections. If the larger Phase III confirms these numbers, we could see a brand‑new class of "one‑and‑done" CRVO treatment within the next few years.
Durable anti‑VEGF delivery systems
Even if gene therapy feels futuristic, companies are already extending the life of existing anti‑VEGF drugs. Biodegradable implants that slowly release ranibizumab or aflibercept over 4–6 months are in late‑stage trials. The idea is simple: a tiny, dissolvable matrix sits in the vitreous and leaks the medication at a controlled rate.
In a recent multi‑center study, patients with the implant needed half the number of clinic visits compared to standard monthly injections, yet their visual acuity improvements were statistically indistinguishable. For busy professionals or anyone who dreads the waiting room, that could be a game‑changer.
Targeted steroid implants with built‑in pressure monitoring
Steroid implants have always been a double‑edged sword—great at reducing inflammation, but risky for intra‑ocular pressure (IOP). A new generation of dexamethasone implants incorporates a micro‑sensor that alerts the physician if IOP begins to climb. The sensor transmits data to a secure app, so you and your doctor can catch pressure spikes before they become a problem.
Early results from a Phase I/II trial showed that patients using the sensor‑enabled implant had a 30 % lower rate of IOP‑related interventions. The added safety net might make steroids a more attractive option for patients who didn't respond well to anti‑VEGF alone.
Combination approaches and adaptive trial designs
Because CRVO can have both vascular leakage and inflammatory components, researchers are testing combos—like a short‑course anti‑VEGF followed by a sustained steroid implant. Adaptive trial designs let investigators tweak dosing schedules on the fly based on each participant's OCT readings. This personalized approach speeds up data collection and often yields better outcomes.
One Australian adaptive trial paired a three‑month loading phase of aflibercept with a low‑dose dexamethasone implant at month 4. Patients who showed residual fluid after the loading phase received the implant, while those who cleared the edema continued on anti‑VEGF alone. The overall retreatment burden dropped by 25 % without sacrificing visual gains.
Actionable steps you can take right now
Ask your retina specialist if any of these trials are recruiting in Sydney or nearby regions. Eligibility often hinges on recent OCT measurements, so bring your latest scans to the conversation.
Keep a detailed log of injection dates, visual changes, and any side effects. Trial coordinators love precise data, and it helps you track whether a new therapy is truly better for you.
Consider genetic testing if you have a family history of vascular eye disease. Some gene‑therapy trials require specific biomarkers, and knowing your status early can open doors.
Stay on top of systemic health—blood pressure, cholesterol, and blood sugar control can affect trial outcomes. A stable systemic profile makes you a more attractive candidate.
Join patient‑focused online communities (e.g., Australian Retina Support groups). Members often share real‑time trial updates, travel reimbursement tips, and insider advice on navigating consent forms.
So, what does all this mean for you? The pipeline is filling up fast, and each new study is designed to reduce the treatment burden while preserving—or even improving—vision. If you’re already on anti‑VEGF, ask your doctor whether a trial could complement your current plan. If you’re early in the diagnosis journey, consider enrolling in a study that matches your disease stage; you might help shape the next standard of care.
Keep an eye on clinicaltrials.gov or the Australian New Zealand Clinical Trials Registry for the latest listings. And remember, every breakthrough starts with a willing participant—your willingness to try something new could be the key to a clearer future.
Conclusion
We've walked through everything from what triggers a CRVO to the latest injection protocols and even the experimental trials on the horizon. By now you should see that effective crvo treatment isn’t a one‑size‑fits‑all recipe; it’s a blend of accurate diagnosis, timely anti‑VEGF shots, lifestyle tweaks, and a willingness to explore emerging options when the standard plan stalls.
So, what’s the next move for you? Start by checking that your blood‑pressure log is up to date, schedule the loading phase OCT if you haven’t already, and ask your retina surgeon whether a steroid implant or a trial could fit your situation. Remember, each appointment is a chance to fine‑tune the plan, not a burden you have to endure.
One simple habit that often slips the mind: keep a tiny notebook or phone note of every injection date, any visual changes, and side‑effects. When you bring that record to the next visit, the doctor can spot trends faster and adjust the regimen before problems grow.
Finally, think of yourself as an active partner in your eye health. The more you understand the why behind each step, the more confident you’ll feel walking into the clinic. If you’re ready to take control, reach out to Dr Rahul Dubey’s Sydney practice today and map out a personalized crvo treatment roadmap.
FAQ
What is the typical timeline for CRVO treatment after diagnosis?
Once your retina specialist confirms CRVO, the first anti‑VEGF injection usually happens within a week. The loading phase consists of three shots spaced about four weeks apart. After that, you’ll have a follow‑up OCT around four weeks later to see how the macular swelling is responding. If the fluid is down, the interval between visits can be stretched; if not, additional injections or a switch to steroids may be considered.
How many anti‑VEGF injections will I need for CRVO?
Most patients start with three loading injections, then move to a maintenance schedule that can range from every four weeks to every ten weeks, depending on OCT results. On average, people with non‑ischemic CRVO receive 5‑8 injections in the first year. Those with persistent fluid may need 10‑12 shots or a combination with a steroid implant to keep the edema in check.
Are steroid implants safe for someone with glaucoma?
Steroid implants can raise intra‑ocular pressure (IOP), which is a concern if you already have glaucoma. Your doctor will measure baseline IOP and monitor it closely after the implant. Many glaucoma patients tolerate a low‑dose dexamethasone implant without trouble, especially if they’re on pressure‑lowering drops. If pressure spikes, the implant can be removed or you may switch back to anti‑VEGF.
What lifestyle changes support CRVO treatment success?
Controlling blood pressure, cholesterol, and blood sugar is the biggest boost you can give your eyes. Aim for systolic pressure under 130 mmHg, LDL below 130 mg/dL, and HbA1c under 7 % if you have diabetes. Regular aerobic activity—30 minutes most days—improves circulation. Keep a simple log of injection dates, vision changes, and any side‑effects; it helps your doctor fine‑tune the plan.
Can I travel for work during the loading phase?
Traveling is okay as long as you keep the injection schedule. Talk to your clinic about arranging a local ophthalmologist to give the next shot if you’ll be away for more than a week. Bring your OCT images (or a digital copy) so the visiting doctor can see how your retina is responding. Don’t forget to pack your eye drops and a brief medical summary.
How do I know if my CRVO is non‑responsive to anti‑VEGF?
After the three‑injection loading phase, your doctor will compare the latest OCT with the baseline. If fluid remains high or vision hasn’t improved by at least one line on the eye chart, that’s a sign of non‑responsiveness. In such cases, many specialists add a steroid implant or switch to a different anti‑VEGF agent. Discuss the risk‑benefit profile of each option before deciding.
Where can I find clinical trials for new CRVO therapies?
Start by asking your retina surgeon if any trials are recruiting in Sydney or nearby hospitals. You can also search the Australian New Zealand Clinical Trials Registry or ClinicalTrials.gov using “CRVO” and “Sydney”. Having recent OCT measurements and a stable systemic health profile makes you a stronger candidate. Joining a patient support group often gives you early heads‑up on trial openings.






Comments