What to Expect During Vitrectomy Recovery Time: A Practical Guide
- Dr Rahul Dubey
- Nov 21
- 18 min read
If you’ve just had a vitrectomy, the swirl of emotions—relief that the surgery is over, anxiety about how long it will take to feel normal—can feel overwhelming.
Most people wonder, “When will I be able to read, drive, or simply look at my favorite TV show without the world feeling fuzzy?” The short answer: recovery isn’t a one‑size‑fits‑all timeline, but there are common milestones you can expect.
In the first 24 to 48 hours you’ll likely keep your eye patched and rest with your head tilted face‑down if a gas bubble was used. That positioning helps the retina seal and is the reason many patients describe the early days as “being on a pillow‑fort.” You’ll notice some blurriness and light sensitivity—normal, not a disaster.
By the end of week one, most surgeons schedule a follow‑up to check that the bubble is still in place and the retina is healing. Around this time you can usually lift the patch, start using prescribed eye drops, and begin light indoor activities. Many patients report being able to read short lines of text with a magnifier, though driving is still off‑limits.
Between two and four weeks, the eye continues to clear the gas or oil and visual acuity improves steadily. You might still need to avoid heavy lifting, vigorous exercise, and anything that raises intra‑ocular pressure. This is the phase where “I can see better, but it still feels weird” is a common sentiment.
Full visual recovery often takes six to eight weeks, but some subtle improvements can continue for three months. The exact timeline depends on factors like the underlying condition, whether a gas or silicone oil was used, and how closely you follow post‑op instructions. That’s why your surgeon will tailor advice to your case.
For a deeper look at how micro‑incision vitrectomy techniques translate into a shorter healing period, check out the Epiretinal Membrane | Dr Rahul Dubey page, which outlines the procedure and typical recovery expectations.
So, what can you do right now to smooth the road ahead? Keep your eye drops on schedule, protect your eye with the shield at night, and don’t hesitate to call your clinic if you notice sudden flashes, increasing pain, or a rapid loss of vision. Your proactive care makes the difference between a good recovery and a prolonged one.
TL;DR
Recovering from vitrectomy takes about six to eight weeks for most patients, with visual clarity steadily improving after the first month but full sharpness often arriving closer to two months.
Stick to your doctor’s drop schedule, protect your eye at night, avoid heavy lifting, and call the clinic immediately if you notice flashes or sudden pain to keep your vitrectomy recovery time on track.
Step 1: What Is Vitrectomy and Why It Matters for Recovery
Imagine waking up after eye surgery, still feeling a little foggy, and wondering exactly what was taken out of your eye. That’s the moment many patients face after a vitrectomy. In plain terms, a vitrectomy removes the gel‑like vitreous humor that fills the inside of your eyeball so your surgeon can repair the retina or clear out debris.
Why does this matter for your vitrectomy recovery time? Because once the vitreous is gone, the eye needs a new “support system” – usually a clear saline solution, a gas bubble, or silicone oil – to keep the retina flat while it heals. The type of fill you get directly influences how long you’ll need to stay face‑down, how quickly your vision sharpens, and what activities you must avoid.
What the surgeon actually does
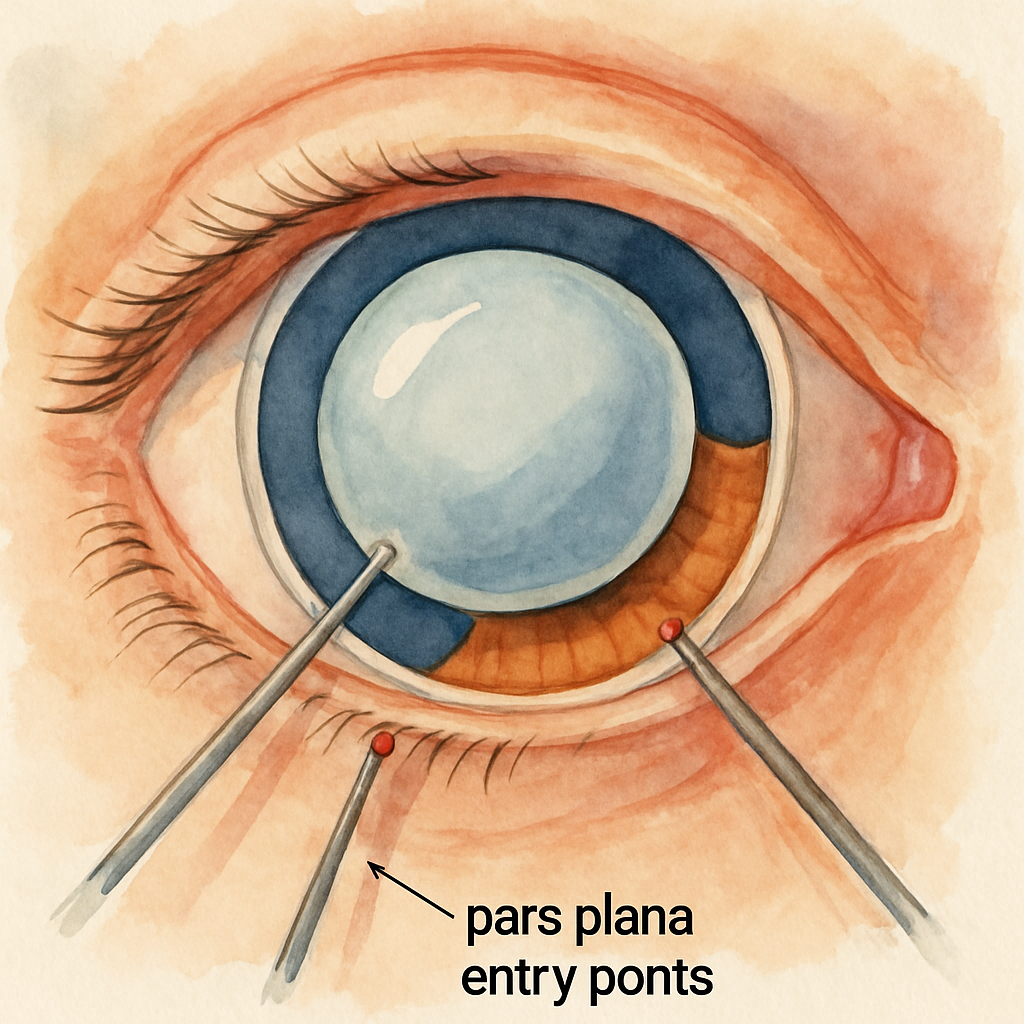
During the procedure the surgeon makes tiny incisions at the pars plana, the flat part of the ciliary body, and inserts micro‑instruments to gently suction out the vitreous. They may also use a laser to seal leaking blood vessels. After the repair, they replace the missing fluid with sterile salt water, a gas bubble, or silicone oil. The Cleveland Clinic explains that the vitreous is “replaced with a clear fluid or a gas bubble until your body begins producing the vitreous again” according to a medical overview .
That replacement is the heart of the recovery timeline. A gas bubble slowly dissolves over weeks, giving you a “cloudy” view that clears from the top down. Silicone oil stays longer and often requires a second surgery for removal. Saline is absorbed quickly, so you may notice visual improvement sooner.
How the fill affects daily life
If you have a gas bubble, you’ll spend the first few days with your head tilted down – think “pillow‑fort” again. That positioning keeps the bubble pressing against the retina, preventing it from shifting. You’ll likely wear an eye shield at night and avoid bending over. For silicone oil, the restrictions are similar, but you’ll also need to schedule a follow‑up to discuss removal.
When saline is used, the eye retains its shape right away, so you might be able to lift the patch and start light indoor tasks earlier. However, even with saline you’ll still need to use prescribed eye drops and watch for any sudden flashes or pain.
Understanding these nuances helps you set realistic expectations for your vitrectomy recovery time. It also guides you in asking the right questions at your post‑op appointment – like “How long will the gas stay in my eye?” or “When can I expect my vision to start clearing?”
Now that you know what’s happening inside your eye, let’s look at the first practical step: tracking your vitrectomy recovery time with a simple checklist. Write down the date of surgery, the type of fill used, and any specific positioning instructions your surgeon gave you. Check this list daily:
Are eye drops being applied on schedule?
Is the eye shield still in place at night?
Any new flashes, pain, or sudden loss of vision?
Keeping this log makes it easier to spot warning signs early and gives your surgeon concrete data at each follow‑up.
One common question is whether the same recovery timeline applies to every condition. The short answer: no. For a macular hole, the visual gains often align with the gas bubble’s absorption, whereas for vitreous hemorrhage the eye may clear faster once the blood is removed. If you’re curious how a macular hole influences recovery, check out our Macular Hole | Dr Rahul Dubey page for details.
Bottom line: the vitrectomy itself usually lasts 30‑60 minutes, but the healing phase stretches over weeks. By understanding why the eye needs a temporary fill and how that fill shapes your day‑to‑day routine, you can actively manage your vitrectomy recovery time and stay on track for clearer vision.
Step 2: Factors That Influence Vitrectomy Recovery Time
Now that you know what a vitrectomy does, let’s dig into the variables that stretch or shrink your healing timeline. It’s not magic – it’s biology, the type of fill you got, and how closely you follow the after‑care plan.
1. What’s inside the eye matters
If your surgeon used a gas bubble, expect a slower visual clearance because the bubble dissolves over weeks. A silicone oil fill can keep the eye stable for months, often requiring a second procedure to remove it. Saline or balanced‑salt solution disappears quickly, so you may notice sharper vision sooner. Our vitrectomy services explain which fill is best for your condition.
Does this change how you schedule appointments? Absolutely – gas‑filled eyes need more frequent checks while the bubble fades.
2. Underlying retinal problem
Macular holes, epiretinal membranes, diabetic tractional detachments – each heals at its own pace. A macular hole’s recovery often mirrors the gas absorption curve, while a vitreous hemorrhage may clear faster once the blood is removed. Knowing the diagnosis helps you set realistic expectations.
So, should you ask your surgeon “When will my specific condition let me drive?” Yes, that question drives better planning.
3. Your personal health profile
Age, diabetes, and smoking status all tip the scales. Diabetic patients are prone to neurotrophic keratopathy, which can add weeks to the timeline. A recent study showed that topical insulin shaved off an average of 12 days of healing time for neurotrophic keratopathy after diabetic vitrectomy (source) . Keeping blood sugar stable and quitting smoking give your cornea a fighting chance.
And what about your eyes themselves? Pre‑existing dry eye or corneal sensitivity issues can slow re‑epithelialization.
4. Post‑op care compliance
Missing eye‑drop doses, dropping the eye shield at night, or bending over too soon can all trigger inflammation or even a retinal detachment. Think of your regimen as a daily checklist – if one item slips, recovery can slip with it.
Do you keep a log? If not, start one now. Write the date, fill type, and any symptoms you notice.
5. Follow‑up visits and monitoring
Regular check‑ups let your surgeon spot trouble early – flashes, pain, or sudden loss of vision are red flags. The more often you’re seen, the sooner an issue can be corrected, preventing prolonged downtime.
What’s the sweet spot? Most surgeons schedule a week‑one visit, then another at two weeks, and a final at six weeks, but adjust based on your fill and condition.
Factor | Impact on Recovery Time | Tips to Optimize |
Intra‑ocular fill (gas, oil, saline) | Gas: 4–6 weeks; Oil: up to 3 months; Saline: 1–2 weeks | Follow positioning instructions; attend oil‑removal appointment |
Underlying retinal disease | Macular hole aligns with gas absorption; hemorrhage may clear faster | Ask surgeon for condition‑specific timeline |
Patient health (diabetes, age, smoking) | Diabetes can add 1–2 weeks; smoking may delay epithelial healing | Control blood sugar, quit smoking, consider topical insulin if neurotrophic keratopathy risk |
Bottom line: your vitrectomy recovery time is a puzzle made of fill type, diagnosis, health habits, and disciplined after‑care. Piece them together, and you’ll move from blurry to crystal‑clear faster than you imagined.
Step 3: Typical Recovery Timeline After Vitrectomy
Let’s walk through what you can expect day by day, week by week, and beyond. Knowing the checkpoints helps you stay on track and spot anything that needs a doctor’s eye.
Day 0‑3: The “Pillow‑Fort” Phase
Right after surgery your eye will be patched and you’ll likely be told to keep your head tilted down if a gas bubble was used. This isn’t just a quirky request; the bubble needs gravity to press against the retina and keep it sealed. Most surgeons ask you to stay face‑down for anywhere from a few days up to a week. The American Academy of Ophthalmology notes that the length depends on the bubble type and can range from a few days to more than a week face‑down recovery guidelines .
Tip: Set up a comfortable station with a face‑down pillow or a reclining chair. Keep water, snacks, and your phone within reach so you don’t have to sit up unintentionally.
Week 1: First Check‑In
At your one‑week appointment the surgeon will look at the bubble, the retina, and your pressure numbers. If everything looks good you’ll likely lift the patch, start using prescribed drops, and get permission for light indoor tasks.
What you might notice: still blurry vision, light sensitivity, and a slight feeling of pressure. That’s normal. Avoid heavy lifting, bending over, and vigorous exercise.
Weeks 2‑4: Bubble Starts to Dissolve
This is the period where you’ll see the most visual improvement. As the gas bubble shrinks, the cloudiness lifts from the top of your field downwards. You may be able to read short lines with a magnifier and watch TV from a comfortable distance.
Practical checklist for these weeks:
Apply eye drops exactly as prescribed – missing a dose can delay healing.
Wear your eye shield at night unless your doctor says otherwise.
Track any new flashes, pain, or sudden loss of vision in a simple log.
If you have silicone oil instead of gas, the timeline stretches a bit. Oil stays in place for weeks to months and usually requires a second procedure to remove it. Your surgeon will set a separate schedule for that.
Weeks 5‑8: Nearing Full Clarity
By the fifth week most gas bubbles are almost gone. Your vision should feel steadier, and you may be cleared for more activities like gentle walking, light housework, and short drives. Still, avoid anything that spikes intra‑ocular pressure – think heavy lifting or high‑intensity workouts.
Ask your doctor these questions at the visit:
When can I safely drive?
Is my visual acuity where we expect it to be for my condition?
Do I need any additional imaging before we call it “healed”?
Beyond Two Months: Fine‑Tuning
Even after the main timeline, subtle improvements can continue for up to three months, especially if you had a macular hole or complex retinal detachment. Keep using any prescribed lubricating drops and protect your eye from wind and dust.
One simple habit that pays off: a daily 5‑minute eye‑movement exercise. Look left, right, up, and down slowly. It encourages fluid circulation and can help reduce lingering glare.
Bottom line: your vitrectomy recovery time follows a predictable rhythm – face‑down positioning, gradual bubble absorption, and steady visual gains. Stick to the schedule, log your symptoms, and keep the follow‑up appointments. That way you move from blurry to clear with confidence.
Step 4: Post‑Operative Care Tips to Speed Up Healing
You've just made it past the bubble‑absorption phase, but the real work starts now. How you treat the next few weeks can shave days off your vitrectomy recovery time or add frustrating setbacks.
First thing’s first – protect that eye like it’s a newborn kitten. Keep the shield on at night, wear sunglasses outdoors, and avoid any situation where dust or wind can get in. A simple habit, but one that the Alberta Health post‑operative guide flags as essential for preventing infection and inflammation.
1. Master Your Drop Routine
Eye drops are the unsung heroes of healing. Set a timer on your phone, or use a pill‑box style organizer, and apply every dose exactly when it’s due. Missing a single dose can prolong inflammation, which in turn drags out the visual recovery curve.
Pro tip: tap the bottle lightly against the side of the sink before squeezing – that little air‑burst reduces the chance of a drop bouncing off the eye.
2. Positioning Without the Panic
If you had a gas bubble, you’ve already endured a few days of face‑down positioning. Now, transition slowly. For the next 7‑10 days, keep your head slightly tilted forward when you’re sleeping; a regular pillow won’t do – a donut‑shaped pillow or a specialized face‑down pillow works best.
Don’t over‑think it. You can still watch TV, read a book, or scroll on your phone – just keep the screen at eye level so you don’t have to crane your neck.
3. Gentle Movement, Not a Marathon
Light activity is a good idea, but heavy lifting, vigorous cardio, or yoga inversions are a no‑no until your surgeon clears you. Think of a daily walk around the block, light housework, or gentle stretching. One real‑world example: Jane, a 58‑year‑old teacher, swapped her morning jog for a 15‑minute stroll and reported clearer vision a week earlier than a friend who pushed through her usual run.
Remember, each spike in intra‑ocular pressure can push the bubble out of place, resetting weeks of progress.
4. Nutrition and Hydration Hacks
Your eye heals faster when your body is well‑fed. Aim for omega‑3‑rich foods (salmon, walnuts) and stay hydrated – the vitreous fluid is mostly water, after all. A study cited by the Practice Plus recovery guide showed patients who drank at least 2 liters of water daily reported less eye‑dryness and smoother drop absorption.
Skip the salty snacks that can cause fluid retention and raise blood pressure; high pressure can subtly affect the healing retina.
5. Keep a Symptom Log (Your Personal Dashboard)
Write down any flashes, new floaters, pain levels, and how many drops you’ve taken each day. This log becomes a conversation starter at your follow‑up and helps you spot red flags before they become emergencies.
Use a simple table on your phone or a paper notebook – whatever you’ll actually look at every night.
6. Know When to Call the Office
Red‑flag symptoms include sudden increase in pain, a rapid loss of vision, or a new curtain‑like shadow. If any of those pop up, call your clinic right away – early intervention can prevent a retinal detachment.
Also, if you notice the bubble isn’t shrinking as expected after two weeks, schedule an extra check‑up. Your surgeon can adjust positioning or prescribe a short course of steroids to speed up clearance.
7. Leverage Professional Support
Our team at About Dr Rahul Dubey offers personalized post‑op coaching. A quick 10‑minute phone call can clarify whether you’re ready to drive, return to work, or need an extra eye‑shield adjustment.
Take advantage of that resource – it’s free, it’s easy, and it keeps your recovery on track.
Bottom line: post‑operative care isn’t about strict rules; it’s about smart, consistent habits. Protect, drop, position, move gently, nourish, log, and call when needed. Follow these steps and you’ll watch your vitrectomy recovery time shrink, getting you back to reading, driving, and enjoying life sooner than you imagined.
Step 5: Lifestyle & Nutrition Adjustments for Faster Recovery
You've just gotten through the drop routine and the bubble is shrinking, but what you eat and how you live day to day can still shave weeks off your vitrectomy recovery time.
Hydrate like your eye depends on it
Water makes up most of the vitreous fluid, so staying well hydrated helps the eye maintain its shape and supports tissue repair. Aim for at least eight glasses a day, and sip steadily instead of gulping all at once. If you forget, set a phone reminder or keep a reusable bottle on your bedside table.
Does a coffee habit hurt you? A moderate cup in the morning is fine, but too much caffeine can raise blood pressure, and that tiny rise can stress the healing retina. Swap one of those extra cups for herbal tea or plain water.
Eat foods rich in omega‑3 and antioxidants
Omega‑3 fatty acids reduce inflammation, which means less swelling around the surgical site. Good sources are salmon, sardines, chia seeds, and walnuts. Toss a handful of walnuts into your morning oatmeal or grill a salmon fillet for dinner.
Antioxidants protect the delicate retinal cells. Berries, leafy greens, and orange vegetables deliver vitamin C, vitamin E, and lutein. A simple salad with spinach, orange carrots, and a squeeze of lemon gives you a nutrient boost without extra effort.
Limit salty and processed foods
Too much salt can cause fluid retention and raise intra‑ocular pressure, which may slow the clearing of the bubble. Try to keep processed snacks, canned soups, and fast‑food meals to a minimum. When you do indulge, balance it with extra water.
Gentle movement, not a marathon
Light activity keeps circulation going and prevents blood clots, but anything that spikes pressure should stay off the table. A 15‑minute walk around the block, gentle stretching, or slow yoga poses are perfect. Avoid heavy lifting, intense cardio, and upside‑down positions until your surgeon gives you the green light.
Remember the story of Jane, the teacher who swapped her morning jog for a short stroll. She noticed her vision cleared a few days earlier than a friend who kept running. Small changes add up.
Sleep posture matters
During the first two weeks keep your head slightly tilted forward while you sleep. A donut pillow or a specialized face‑down pillow works better than a regular pillow. This tiny adjustment keeps the bubble in place and reduces the chance of a sudden shift that could delay healing.
Mind‑body balance
Stress releases cortisol, which can interfere with wound healing. Take five minutes each day to breathe deeply, listen to calming music, or practice guided meditation. Even a short pause can lower heart rate and give your eye a calmer environment to repair.
If you feel anxious about your vitrectomy recovery time, write down three things you’re grateful for each evening. It shifts focus away from worries and reinforces a positive mindset.
Create a simple recovery checklist
Putting everything on paper turns vague advice into concrete actions. List each habit: drink eight glasses, eat omega‑3 at lunch, walk 15 minutes, log sleep position, and note any new flashes or pain. Check it off each evening. The habit of checking reinforces compliance and speeds up recovery.
So, what’s the next step? Grab a notebook, fill in the checklist, and start tweaking one habit today. You’ll notice the vitrectomy recovery time shrink as your body gets the nutrients, rest, and gentle movement it needs.
Step 6: Warning Signs & When to Contact Your Surgeon
You've just tuned your daily checklist, but there’s a flip side – the moments when something feels off and you need to act fast.
In the first weeks after vitrectomy, most days are routine: drops, rest, a quick walk. Still, a handful of warning signs can mean the difference between a smooth recovery and a setback that adds weeks to your vitrectomy recovery time.
Red‑flag symptoms you shouldn't ignore
Here are the top red‑flag symptoms that should trigger an immediate call to your surgeon:
Sudden increase in pain that doesn't ease with your usual eye‑drop regimen.
New or worsening flashes of light, especially if they appear in peripheral vision.
Rapid loss of vision – even a few letters on the eye chart disappearing fast.
Seeing a dark curtain or shadow that spreads across your field of view.
Persistent redness, swelling, or discharge that looks different from normal post‑op inflammation.
Feeling that the gas bubble is not shrinking as expected after two weeks (you might notice the cloudy spot staying the same size).
If any of these pop up, don't wait for the next appointment. A timely call can catch a retinal detachment, infection, or pressure spike before they turn into a longer‑term problem.
How to act when a warning pops up
Follow this quick three‑step plan to keep your vitrectomy recovery time on track:
Call your surgeon’s office right away.Mention the exact symptom, when it started, and whether it’s getting better or worse.
Document what you see.Write the time, intensity, and any activities you were doing when the symptom began. A quick photo of the eye (if you can safely do so) helps the doctor assess the situation.
Follow the surgeon’s instructions.They may ask you to come in for an urgent exam, adjust your drop schedule, or start a short course of steroids. Do exactly what they say – even if it feels like extra work.
While you’re waiting for the call to connect, keep your eye shield on and avoid rubbing the eye. Resting upright rather than bending over can also reduce pressure spikes.
Imagine you’re at work and a sudden flicker of light catches your eye. You pause, glance at the clock, and realize it’s been two days since your last check‑in. That tiny moment of awareness can prevent a full‑blown detachment and shave a week or two off the expected vitrectomy recovery time. Acting fast is the secret sauce.
Creating a quick‑response checklist
Turn the three‑step plan into a tiny checklist you can keep on your nightstand:
Symptom noticed? (yes / no)
Time and description written down?
Phone number of surgeon dialed?
Eye shield on and eye not touched?
Follow‑up instructions received?
Checking each box takes less than a minute, but it gives you a clear path when anxiety tries to creep in. Remember, the goal isn’t to panic – it’s to catch a problem early enough that your vitrectomy recovery time stays on schedule.
Bottom line: knowing the warning signs and having a ready‑to‑go response plan puts you in the driver’s seat of your own healing. Keep this checklist handy, trust your instincts, and don’t hesitate to pick up the phone. Your surgeon is there to help you get back to reading, driving, and enjoying life as quickly as possible.
Conclusion
We've walked through the timeline, the red‑flag checklist that can shave days off your vitrectomy recovery time. At the end of the day, the most powerful tool you have is simply paying attention to what your eye is telling you.
So, what’s the next move? Grab that quick‑response checklist you built earlier, keep it on your nightstand, and scan it each morning. If a flash or a new ache shows up, dial your surgeon right away – early action is what keeps the recovery clock from ticking up.
Remember, the type of fill (gas, oil, or saline) sets the baseline, but your compliance with drops, positioning, and activity limits decides how close you get to the best possible vitrectomy recovery time.
And if you’re wondering how a specific condition like a macular hole might change the curve, our Vitreous Floaters page breaks down the nuances in plain language.
Bottom line: stay proactive, log every symptom, and trust the checklist. Your vision will clear, your confidence will grow, and before you know it you’ll be back to reading, driving, and enjoying the things you love.
Take a minute each day to visualize the bubble shrinking and your eye getting clearer – it’s a tiny mental cue that reinforces your commitment and speeds healing.
FAQ
How long does vitrectomy recovery time usually take?
Most patients see the biggest jump in clarity within the first six to eight weeks after surgery. The first few days are all about the face‑down positioning and the bubble settling, then vision sharpens week by week. By the end of the second month many folks can read fine and even start short drives, though full stability can stretch to three months for complex cases.
What factors can speed up or slow down vitrectomy recovery time?
Age, diabetes, smoking and the specific retinal problem all play a part. Younger eyes with good blood flow tend to heal faster, while uncontrolled diabetes can add a week or two. A gas bubble usually drags the timeline out to four‑six weeks, but saline clears in a week or two. Sticking to the drop schedule and avoiding heavy lifting are the biggest levers you control.
When should I contact my surgeon during recovery?
Any sudden flash, new floaters, sharp pain or a rapid loss of vision means you should call your surgeon right away. Also, if the cloudy spot from the gas bubble isn’t shrinking after two weeks, give the office a ring. Keep a small notebook by your nightstand, jot down the time and what you were doing when the symptom appeared – it helps the doctor decide how urgent the visit is.
How does the type of intra‑ocular fill affect recovery time?
The fill you get – gas, silicone oil or balanced‑salt solution – is the biggest determinant of how long you’ll be in the recovery window. A gas bubble stays visible for four to six weeks, so you’ll notice a hazy view until it dissolves. Silicone oil can linger for months and often needs a second surgery for removal. Saline or BSS is absorbed in a week or two, letting you see sharper sooner.
What daily habits help shorten vitrectomy recovery time?
Stick to your drop schedule, protect the eye at night and keep the head slightly forward while you sleep for the first two weeks. Drink plenty of water, eat omega‑3 rich foods and avoid salty snacks that can raise intra‑ocular pressure. Light activity like a 10‑minute walk is great, but skip heavy lifting, vigorous cardio and yoga inversions until cleared. A quick daily log of symptoms and drop times keeps you honest and can shave a few days off the overall timeline.
Is it safe to resume driving and exercise, and when?
Most surgeons give the green light to drive once you can read a full eye‑chart line without magnification and your vision is at least 20/40 in the operated eye – typically around week six. For exercise, start with gentle walking or light household chores after the first two weeks, then add low‑impact activities like stationary cycling around week four. Always get a clearance note before returning to running, weightlifting or any sport that could raise intra‑ocular pressure.






Comments