Understanding macular hole symptoms: What to watch for and when to act
- Dr Rahul Dubey
- Nov 24, 2025
- 17 min read
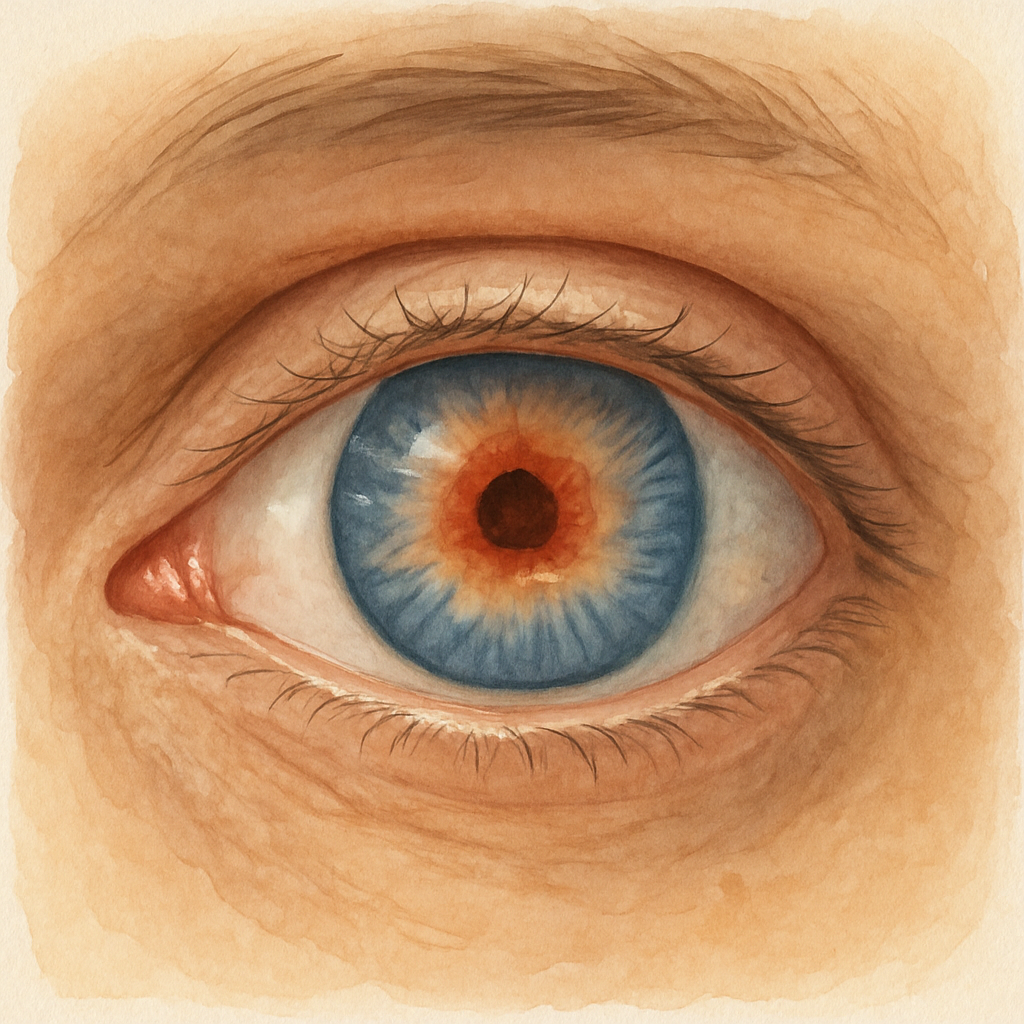
Imagine looking at a familiar face on your phone and suddenly the center of the image looks blurry, like someone placed a tiny smudge over the lens.
That weird distortion could be one of the first macular hole symptoms, and if you’ve never heard the term before it’s easy to dismiss it as just normal aging.
But the reality is a macular hole is a tiny break in the central retina, and the symptoms often start subtly—like a dark spot in the middle of your vision or a slight wobble when you read.
Do you ever notice straight lines bending or a sudden difficulty recognizing faces you’ve seen a hundred times? Those are classic red flags that something’s shifting in the macula.
Another common macular hole symptom is reduced contrast sensitivity—you might find it harder to see shades of gray, making everyday tasks like checking traffic lights feel off.
If you’ve experienced any of these signs—blurry central vision, a dark or gray spot, straight lines that look wavy, or trouble with contrast—it’s worth getting your eyes examined sooner rather than later.
The good news is that once a retinal surgeon like Dr Rahul Dubey identifies the macular hole, there are proven surgical options that can close the gap and restore much of your vision.
So, keep an eye out for those subtle changes, and don’t wait for them to worsen. Your next step? Book a comprehensive retinal check‑up and get clarity on what’s really happening inside your eye.
Early detection matters because the longer the hole stays open, the more retinal tissue can shrink, making surgery less effective. That's why noticing macular hole symptoms early gives you a better chance at a full recovery.
Remember, you don’t have to navigate this alone—Sydney’s retina specialists are ready to evaluate your vision and discuss personalized treatment plans that fit your lifestyle.
TL;DR
If you notice a blurry spot, wavy lines, or trouble recognizing familiar faces, those are classic macular hole symptoms that merit prompt eye‑exam. Early detection lets Sydney’s retinal surgeon Dr Rahul Dubey offer proven surgery, giving you a strong chance of restoring clear central vision and prevent permanent vision loss for you.
Recognizing early macular hole symptoms
Imagine you’re scrolling through photos on your phone and, out of nowhere, a tiny gray smudge appears right in the middle of the picture. It isn’t a camera glitch – it’s your eye sending you a warning sign.
That smudge, that wobble, that moment when straight lines look a little wavy – those are the classic earlymacular hole symptoms. They’re subtle, they’re easy to ignore, and that’s exactly why we need to talk about them in plain language.
What the symptoms actually feel like
First, there’s the blurry spot. Most people describe it as looking through a dirty window or a tiny oil droplet on a lens. It usually shows up in the center of your vision, so reading a page or recognizing a familiar face becomes a bit of a guessing game.
Second, you might noticemetamorphopsia– the fancy term for lines that bend or bend like they’re on a funhouse mirror. Think about it this way: you’re looking at a ruler, but it suddenly looks like it’s curving upward in the middle. That’s a red flag.
Third, contrast sensitivity can dip. You may find it harder to tell the difference between a pale gray sky and a slightly darker cloud, or you might misread traffic lights because the reds and greens don’t pop like they used to.
Real‑world examples that hit home
Sarah, a 62‑year‑old retiree from Sydney, first thought the dark spot in her central vision was just age‑related “cloudiness.” She kept reading her favorite newspaper and kept missing a few words. After a week of frustration, she mentioned the problem to her daughter, who suggested an eye check‑up. The exam revealed an early macular hole, and Dr. Rahul Dubey was able to schedule a vitrectomy before the hole enlarged.
Mike, a 48‑year‑old graphic designer, noticed that straight‑edge lines in his design software started to look wavy during a client presentation. He described the sensation as “the screen was breathing.” An urgent retinal scan showed a stage‑2 macular hole. Because he caught it early, the surgery restored his central vision to near‑normal levels, saving his career.
How to spot the signs yourself – a quick checklist
1.Central blur: Is a spot or smudge appearing in the middle of what you see?
2.Distorted lines: Do straight edges look bent, especially when looking at a grid or a printed page?
3.Reduced contrast: Are you struggling with subtle shades, like differentiating a pale traffic light?
4.Reading difficulty: Do you need to hold books farther away or squint more than usual?
If you answer “yes” to any of these, it’s time to book a comprehensive retinal exam.
What to do next – actionable steps
•Schedule an OCT scan. Optical coherence tomography gives a cross‑section view of your macula and can confirm a hole that looks invisible to the naked eye.
•Ask about the Watzke‑Allen test. It’s a simple slit‑lamp maneuver that helps differentiate a full‑thickness hole from a pseudo‑hole.
•Don’t wait for the hole to grow. Early surgery, often a pars‑plana vitrectomy with internal limiting membrane peeling, has a success rate above 90% for restoring central vision.
For a deeper dive into what the surgery entails, check out our Macular Hole | Dr Rahul Dubey page.
While you’re focusing on eye health, remember that nutrition plays a supporting role. Tracking your diet with a tool like Foodie Cal can help you ensure you’re getting the antioxidants and omega‑3s that support retinal health.
Lastly, keep a simple diary. Jot down when you first notice the smudge, any changes in distortion, and how it affects daily tasks. That record becomes valuable information for your surgeon.
Early detection turns a potentially permanent vision loss into a manageable condition with a high chance of recovery. So, if any of those symptoms ring a bell, treat them like a text message from your body that says, “Hey, check this out.”
How macular hole symptoms progress over time
When a macular hole first forms, the brain tries to compensate, so you might only notice a faint smudge or a subtle wobble when you read a newspaper. That feeling usually lasts a few weeks to a month, and many people shrug it off as “just getting older.” But underneath, the retinal tissue is already beginning to thin, and the hole can grow in size if nothing changes.
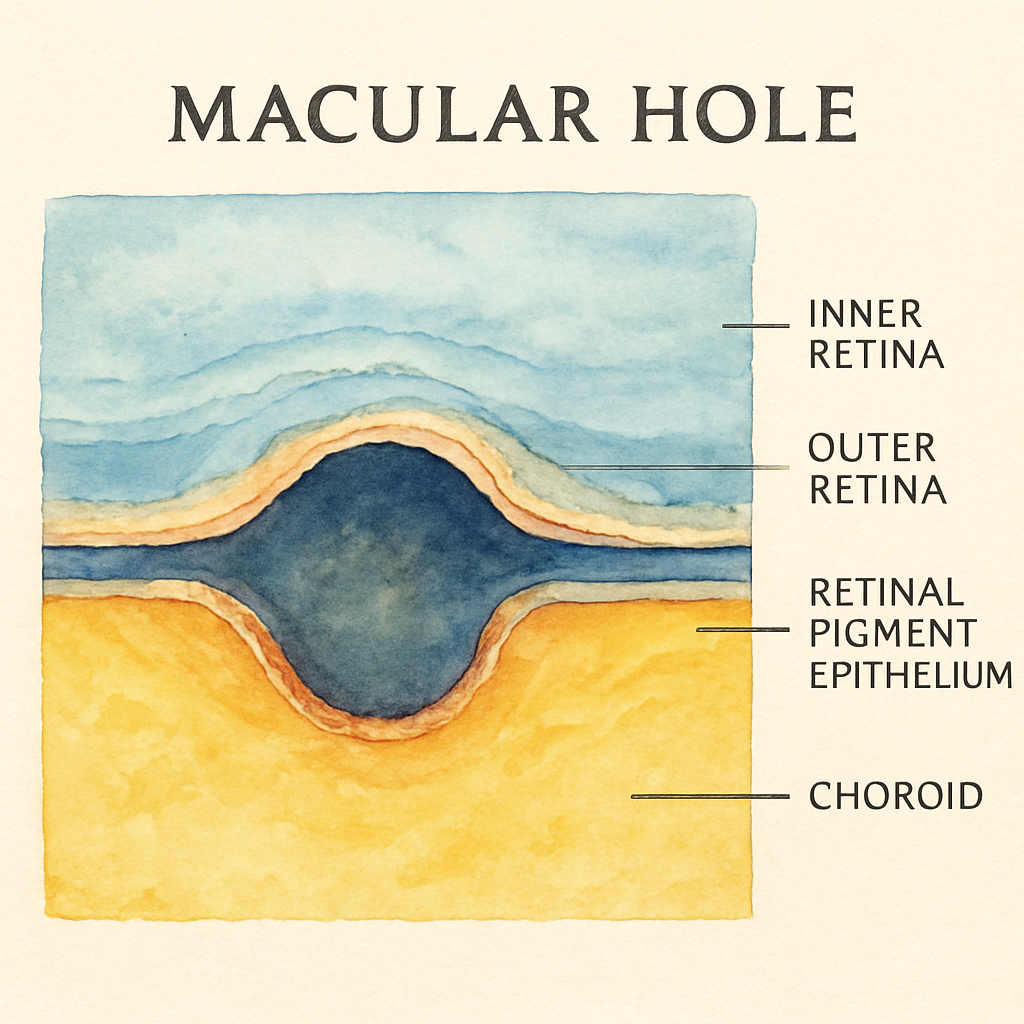
Stage 1 – the incipient blur.In the earliest phase the defect is less than 200 µm wide. Central vision is still mostly intact, but you may see a gray spot that disappears when you look away and comes back when you refocus. Contrast drops a notch, so a pale traffic light may look like a dimmer version of its usual bright color. At this point, an optical coherence tomography (OCT) scan will show a tiny interruption in the outer retinal layers, but the surrounding tissue looks healthy.
Stage 2 – widening and metamorphopsia.As the hole expands to 200‑400 µm, straight lines begin to bend. You might describe it as “the screen is breathing” or “the ruler looks like a smile.” Reading becomes slower because you have to guess missing letters. Studies of untreated eyes show that, on average, the hole enlarges about 100 µm every 6 months, although the rate can accelerate if vitreous traction increases.
Stage 3 – full‑thickness involvement.Once the gap exceeds 400 µm, the central fovea loses its photoreceptors. The dark spot becomes permanent, and you may notice a “missing puzzle piece” in the middle of your vision. Peripheral vision remains, so you can still drive, but facial recognition and fine detail work (like threading a needle) become frustratingly difficult.
Sarah, a 62‑year‑old retiree from Sydney, first thought her blurry spot was just age‑related cloudiness. She kept scrolling through her tablet, squinting to make out the headlines. After a week of missed words, she finally mentioned it to her daughter, who urged a retinal check‑up. The OCT revealed a stage‑1 hole, and Dr Rahul Dubey performed a pars‑plana vitrectomy within two weeks. Six months later Sarah reported “reading feels like I’m looking through a clean window again.”
Mike, a 48‑year‑old graphic designer, noticed his design grids wavering during a client presentation. He described the sensation as “the screen was breathing.” An urgent scan showed a stage‑2 hole measuring 350 µm. Because he acted quickly, the surgery restored his central acuity to 20/25, and he avoided a career‑limiting loss of detail work.
How to track the progression yourself
Mark the date you first see the smudge.
Every few days, stare at a printed 10‑centimeter ruler held at 30 cm and note any curvature.
Use a simple contrast chart (black on gray vs. black on white) to see if shades blend together.
Log these observations in a phone note or paper diary – the pattern often predicts how fast the hole is growing.
When you notice any change, schedule an OCT within 7 days. Early imaging lets your surgeon decide whether to observe or operate. If the hole is still under 400 µm, many surgeons, including Dr Dubey, recommend surgery because the success rate for restoring central vision exceeds 90 % when the procedure is done before the tissue shrinks.
Expert tip: don’t wait for “worse” – According to Dr Dubey, “the longer a macular hole stays open, the more the surrounding retina contracts, and the harder it is to close surgically.” He suggests a “watch‑and‑wait” window of no more than 8 weeks for stage‑1 holes; after that, the odds of a perfect closure drop noticeably.
For a deeper dive into the surgical steps, you can explore our Cataract | Dr Rahul Dubey page, which also outlines pre‑operative eye‑health checks that apply to macular procedures.
While you’re focused on your own vision, remember that the clinicians who treat you also need support. Our colleagues at e7D‑Wellness provide evidence‑based tools to help eye‑care professionals manage stress and avoid burnout – something that ultimately benefits every patient.
Bottom line: keep a simple diary, get an OCT at the first sign of change, and don’t let a tiny blur turn into a permanent blind spot. Acting within the first few weeks gives you the best chance of a full‑vision recovery.
When to seek professional help for macular hole symptoms
Ever notice a tiny smudge in the middle of your vision and think, "maybe I just need glasses"? That little blur can be the first whisper of a macular hole, and ignoring it might let the problem grow.
Here’s the thing: the longer the hole stays open, the more the surrounding retina contracts, making surgical closure tougher. Dr Rahul Dubey often says, “If you wait for the blur to get worse, you’re betting against yourself.” So, catching the warning signs early is the smartest move.
Red flags that scream "call your eye doctor"
•Central dark spotthat appears out of nowhere and doesn’t fade when you look away.
•Distorted lines– straight edges look wavy, like a funhouse mirror.
•Sudden loss of contrast– traffic lights feel muted, reading feels fuzzy.
•Reading fatigue– you have to hold books farther or squint more than usual.
If any of those hit home, it’s time to act. Even a single day of hesitation can let a 200 µm hole expand beyond the sweet‑spot where surgery boasts a 90 %+ closure rate.
What a timely OCT can tell you
Optical coherence tomography (OCT) is the gold‑standard for spotting a macular hole before it becomes obvious to the naked eye. A quick scan will show you the exact diameter – and that number guides whether you need surgery now or can watch a bit longer.
In a recent consensus study , experts agreed that holes smaller than 400 µm have the best chance of full closure when operated on within weeks of symptom onset.
So, schedule that OCT the moment you notice a change. Don’t wait for the next eye‑exam slot six weeks from now.
When to pick up the phone
• You see a new central blur that lasts more than a couple of days.
• Metamorphopsia (wavy lines) appears suddenly while you’re scrolling on your phone.
• Contrast loss makes everyday tasks feel like a guessing game.
• You’ve already kept a diary of symptoms and the pattern is worsening.
Give Dr Dubey’s clinic a call, mention the specific symptom, and ask for an urgent OCT appointment. Mention that you’ve been tracking the changes – it shows you’re proactive and helps the surgeon plan.
And if you’re already seeing a specialist, bring up the “watch‑and‑wait” window that Dr Dubey recommends: no more than eight weeks for stage‑1 holes. After that, the odds of a perfect closure drop noticeably.
What to expect when you get there
During the visit, the doctor will review your OCT, measure the hole, and discuss whether immediate surgery is the best route. If the hole is under 400 µm and you’re in the early weeks, surgery is usually advised because the success rate for restoring central vision exceeds 90 %.
Even if you’re still in the observation phase, the doctor might suggest lifestyle tweaks – like reducing prolonged screen time and protecting your eyes from bright glare – to ease the strain while you wait.
Need a quick look at what the surgery entails? Check out our full range of retinal services for a plain‑language overview of vitrectomy, internal limiting membrane peeling, and gas tamponade.
Below is a short video that walks you through the typical OCT scan and what surgeons look for. It’s a good way to visualise the process before you even step into the clinic.
After watching, you’ll see why waiting isn’t an option. The image on the screen shows the tiny break in the retina that can be closed with a tiny bubble of gas – but only if we act fast.
Bottom line: if any macular hole symptom pops up, treat it like a text message from your eye saying, “Help me now.” Book an OCT, call the clinic, and don’t let a tiny blur become a permanent blind spot.
Comparing diagnostic tools for macular hole evaluation
When you first notice a blurry spot, your brain starts looking for answers. Is it just eye‑strain, or is there something deeper under the retina?
We’ve already talked about the symptoms, now let’s see how the tools we use actually spot the hole. The right diagnostic test can mean the difference between watching a problem grow and catching it early enough for a 90%+ closure rate.
First up: Optical Coherence Tomography (OCT). Think of OCT as a tiny ultrasound that uses light instead of sound. It gives you a cross‑section view of every retinal layer, letting us measure the hole’s diameter down to the micron.
Why does that matter? A study showed a generative deep‑learning model could predict post‑surgery OCT images with 94.7% accuracy and an F1 score of 0.891, proving that OCT data is reliable enough to forecast how the macula will heal after surgery recent AI study .
Next, we have the classic fundus photograph. It’s quick, inexpensive, and great for documenting the overall health of the retina. But a macular hole often looks like a subtle dark spot on a color photo – easy to miss unless you’re trained to spot it.
Then there’s the Watzke‑Allen test, a simple slit‑lamp maneuver. You place a thin beam of light across the macula; if the patient sees a break in the line, you’ve got a functional confirmation of a full‑thickness hole.
So, how do you decide which tool to use? Below is a quick‑look table that compares the three most common options.
Feature | Tool | Notes |
Resolution | Optical Coherence Tomography (OCT) | Micron‑level detail; quantifies hole size, ELM/EZ status |
Speed & Cost | Fundus Photography | Fast, low‑cost; good for screening, less detail |
Functional Insight | Watzke‑Allen Test | Detects full‑thickness breaks; subjective, complements imaging |
In practice, most retina specialists start with OCT because it tells you exactly how big the hole is and whether the outer retinal layers (ELM, EZ) are intact – both big predictors of visual recovery.
But here’s a tip most people overlook: combine OCT with the Watzke‑Allen test if the scan is borderline. The test can catch a tiny fissure that the OCT algorithm might classify as a pseudo‑hole.
And don’t forget the patient’s own story. Keep a diary of when the blur started, how it changes with lighting, and whether straight lines look wavy. That narrative can guide you toward ordering the right test sooner rather than later.
If you’re wondering where to find more details about the surgeon’s expertise and why a particular technique (like an inverted ILM flap) might be chosen, check out the About Dr Rahul Dubey page. It explains the experience behind the equipment choices you’ll see in the clinic.
Finally, remember that technology is only as good as the clinician interpreting it. A high‑resolution OCT image can look perfect on paper, but if the doctor doesn’t connect the dots with your symptoms, the hole can still slip through the cracks.
Bottom line: OCT gives you the numbers, fundus photos give you the big picture, and the Watzke‑Allen test gives you functional confirmation. Use them together, keep track of your symptoms, and you’ll have the best shot at a successful repair.
Managing symptoms while awaiting treatment
So you’ve booked that urgent OCT and the surgeon has said “we’ll operate in a few weeks.” In the meantime the blurry spot is still there, the lines still wobble, and you’re probably wondering how to keep life from feeling like a constant reminder of the hole.
First thing: give your eye a break. It sounds simple, but we all push our screens, read in low light, and stare at road signs for hours. Reducing prolonged glare and screen time lets the retina settle and can lessen the sensation of metamorphopsia. Try the 20‑20‑20 rule – every 20 minutes look at something 20 feet away for 20 seconds. It’s a tiny habit that tricks your brain into resetting the visual processing loop.
Track what changes – a symptom diary works wonders
Grab a notebook or a note app and jot down three things each day: the time you first noticed the blur, any new distortion (like a wavy line on a printed page), and what you were doing when it got worse or better. Seeing a pattern on paper often reveals that certain lighting or specific tasks trigger the flare‑up. When you finally sit down with Dr Dubey, that diary becomes a shortcut to a focused conversation.
Does it feel like you’re over‑reacting? Not at all. Patients who log their symptoms tend to report less anxiety because they have concrete data instead of vague worries.
Nutrition and hydration – the quiet helpers
Your retina thrives on omega‑3 fatty acids, lutein, and zeaxanthin. Think of them as the oil that keeps the tiny gears of your eye moving smoothly. Adding a serving of salmon, a handful of walnuts, or a cup of kale smoothies each day can modestly improve contrast sensitivity. And stay hydrated – dehydration can thin the vitreous humor, potentially increasing traction on the macula.
While you’re tweaking your diet, remember that the same nutrients support overall eye health, so you’re not just “buying time” but actually strengthening the tissue that’s about to be repaired.
Protect your eyes from extra stress
Wearing sunglasses with UV‑400 protection outdoors isn’t just a fashion statement; UV light accelerates retinal aging. Inside, consider a matte screen filter on your laptop or phone to cut blue‑light glare. If you notice that bright sunlight makes the central blur pop out more, that’s a cue to wear your shades even on overcast days.
And if you wear contact lenses, keep them clean and follow the replacement schedule. A tiny scratch on a lens can amplify visual distortion, making it harder to separate “my symptom” from “my lens issue.”
Gentle eye exercises – don’t go overboard
There’s no magic cure, but a few simple eye‑movement drills can improve ocular blood flow. One favorite is the “figure‑eight” – slowly trace an imaginary eight in the air with your eyes, first clockwise then counter‑clockwise, for about a minute. Do it while seated, eyes relaxed, and you’ll often feel a subtle reduction in the “wiggle” you see on straight lines.
Just avoid any forceful squeezing or pressure; you want circulation, not strain.
When to call the clinic
If the central dark spot suddenly enlarges, if you start losing peripheral vision, or if you develop flashes of light, treat it like a fire alarm. Those are red‑flag signs that the hole may be progressing faster than expected, and you’ll want an urgent re‑scan.
Otherwise, keep the line open with the office. A quick email with a photo of your diary entry can prompt the nurse to prioritize a follow‑up OCT without you having to sit in the waiting room.
And just in case you’re curious about what the recovery will look like after the vitrectomy, you can read more about the post‑operative timeline on our Vitrectomy recovery guide . Knowing the next steps can make the waiting period feel less like a void and more like a preparation phase.
Bottom line: keep your eyes rested, log every change, feed your retina, protect against glare, and stay in touch with your surgeon. Those small actions won’t close the hole, but they’ll keep you comfortable and informed until the day you walk into the operating room.
Conclusion
We've walked through what macular hole symptoms feel like, why catching them early matters, and how to keep yourself comfortable while you wait for treatment.
So, what should you do next? First, treat that tiny blur like a text from your eye – log when it started, note any wavy lines, and compare how different lighting changes the view.
Second, book an OCT scan as soon as you notice a change. A quick scan gives your surgeon the exact size of the hole and lets you avoid the steep decline in closure rates that comes with delays.
Third, protect your retina every day: wear UV‑400 sunglasses outdoors, give your eyes regular breaks from screens, and add omega‑3‑rich foods or a kale‑salad smoothie to support healing.
Remember, these small steps won’t close the hole on their own, but they buy you time and keep your vision as clear as possible until surgery.
If any symptom worsens – the dark spot expands, you see flashes, or peripheral vision fades – call Dr Rahul Dubey’s clinic right away for an urgent re‑scan.
Bottom line: stay observant, act fast, and lean on a trusted retina specialist. Your eyes deserve that level of care.
By following this checklist you’ll move from uncertainty to confidence, knowing you’ve done everything possible to protect your sight.
FAQ
What are the earliest macular hole symptoms I should watch for?
In the first few weeks you might notice a tiny gray spot right in the center of your vision, like looking through a smudge on a camera lens. Straight lines can start to look a little wavy, especially when you read a newspaper or glance at a computer screen. Contrast may feel muted – a pale traffic light can look almost the same colour as the background. If any of these subtle changes appear, jot them down and schedule an OCT scan right away.
How quickly do macular hole symptoms progress if I wait?
Research shows that a hole smaller than 400 µm can enlarge about 100 µm every six months, but the rate can accelerate if vitreous traction increases. That means a hole you notice today could become twice its size in a year, lowering the chances of a full‑thickness closure after surgery. Acting within the first few weeks gives you the best odds – over 90 % success – for restoring central vision.
Can I still drive safely while I have macular hole symptoms?
Most people retain peripheral vision, so basic driving is usually possible, but reduced contrast can make it harder to see traffic lights or road signs in low light. If you find yourself squinting, missing colour cues, or feeling uneasy at night, limit driving to daylight hours and keep a pair of UV‑400 sunglasses handy. Inform your ophthalmologist about any driving concerns during your next visit.
Should I keep using contact lenses or glasses while I wait for surgery?
Yes, continue wearing your prescribed correction, but make sure lenses are clean and replaced on schedule. A scratched contact lens can add glare and exaggerate the wavy‑line effect, making it harder to distinguish your actual symptoms from lens artifacts. If you notice increased irritation or distortion after putting in contacts, switch to glasses until the surgeon advises otherwise.
What lifestyle changes can help slow the worsening of macular hole symptoms?
Give your eyes regular breaks – the 20‑20‑20 rule works wonders: every 20 minutes, look at something 20 feet away for 20 seconds. Protect your eyes from bright sunlight with UV‑400 sunglasses, and consider a matte screen filter for indoor devices. Adding omega‑3‑rich foods like salmon, walnuts, or a kale‑smoothie each day supports retinal health, while staying well‑hydrated helps keep the vitreous gel from pulling harder on the macula.
When is it an emergency and I need to call the clinic right away?
If the central dark spot suddenly expands, you start seeing flashes of light, or peripheral vision begins to fade, treat it like a fire alarm. Those signs suggest the hole may be growing rapidly or that a retinal detachment is developing. Call Dr Rahul Dubey’s clinic immediately, request an urgent OCT, and avoid driving until you’ve been cleared.






Comments