pvd vs retinal detachment symptoms: What to Look For and When to Act
- Dr Rahul Dubey
- Dec 17
- 19 min read
Imagine you're watching TV and suddenly a curtain seems to drift across part of your vision. Your heart skips a beat because you wonder if that’s just a harmless float or something far more serious.
That feeling is exactly what many of our patients describe when they experience posterior vitreous detachment (PVD). In most cases PVD shows up as fleeting flashes of light or a few specks that float around – like dust in a sunbeam. It’s unsettling, but usually harmless.
Now picture the same scenario, but the darkness spreads quickly, like a blackout over a city skyline, and you notice a sudden loss of peripheral vision. That’s a red flag for retinal detachment, which demands immediate attention. The key difference? PVD symptoms tend to be intermittent and mild, while retinal detachment symptoms are progressive, often accompanied by a “curtain” effect and a sharp decline in visual acuity.
In our clinic, we’ve seen a 45‑year‑old myopic patient who brushed off a few floaters for weeks. He later reported a growing shadow in his right eye, and when we examined him, a retinal tear had already formed. Early detection could have saved him an urgent surgery.
Here’s a quick checklist you can run through the next time you notice something odd:
Are the symptoms sudden or gradual?
Do you see isolated floaters or a full‑field curtain?
Is there any accompanying loss of side vision?
Do flashes occur in one eye only?
If you answer “yes” to the latter three, treat it like an emergency and book an appointment right away. A timely referral to a retinal specialist can mean the difference between a simple laser seal and a more invasive vitrectomy.
For a deeper dive into how PVD can lead to retinal tears, check out our guide on Vitreous Floaters - Retinal Detachment . It walks you through the anatomy, risk factors like high myopia, and what to expect during a retinal exam.
Also, while you’re focusing on your eyes, remember that overall sensory health matters. Our friends at Brighter Ears hearing clinic offer comprehensive hearing assessments that often go hand‑in‑hand with eye health checks, especially for older adults.
Bottom line: trust your instincts. If a floaters‑only experience feels stable, keep monitoring. If a curtain‑like shadow appears, act fast. Your vision is priceless, and early action is the best safeguard.
TL;DR
If you’re juggling floaters, flashes, or a sudden curtain‑like shadow, this guide breaks down pvd vs retinal detachment symptoms so you can spot the red flags fast and know when to act. We’ll walk you through quick checklists, real‑world examples, and the exact steps to get prompt care from a retina surgeon in Sydney, helping you protect your vision before it’s too late.
What Is Posterior Vitreous Detachment (PVD)?
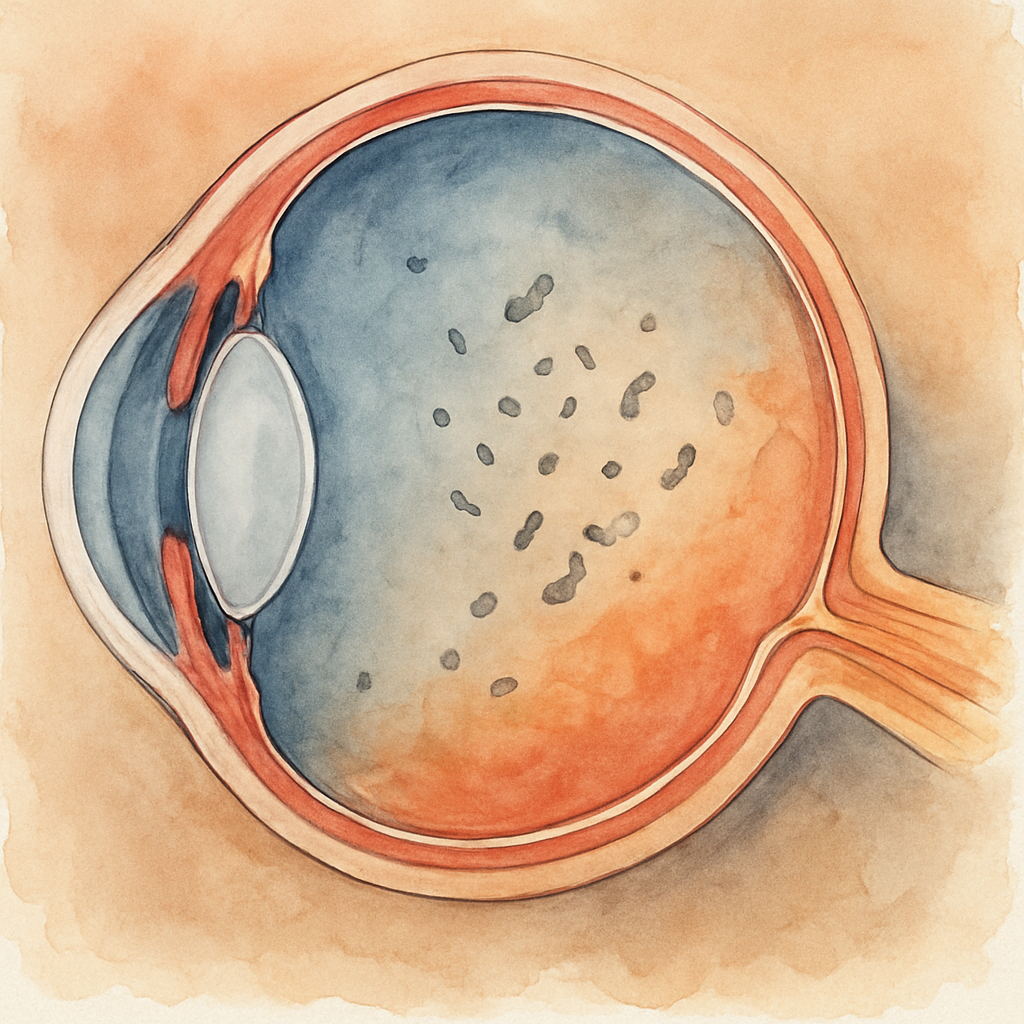
Imagine looking at the sky and noticing a few specks drifting across your vision, like dust motes in a sunbeam. That’s often the first clue that the vitreous – the clear gel filling the back of your eye – is starting to pull away from the retina. In everyday language, we call that posterior vitreous detachment, or PVD.
But why does it happen? As we age, the vitreous slowly shrinks and becomes more liquid. The once‑smooth bond with the retina weakens, and tiny pockets of collagen separate. When those pockets collapse, they tug on the retinal surface. Most of the time the tug feels harmless – a flash of light or a few floating dots – and the eye simply adapts.
So, what should you actually look for? The classic PVD symptoms are intermittent flashes (like tiny fireworks), a sudden increase in floaters, and a vague sense that something’s shifted in your field of view. If the flashes are brief and the floaters stay confined to one area, you’re likely dealing with a standard PVD. If, however, you notice a curtain‑like shadow spreading or a rapid loss of peripheral vision, that’s a red flag for retinal detachment, and you need urgent care.
In our practice in Sydney, we see a wide range of patients – from someone getting a no‑gap eye surgery to a senior coming in for macular degeneration treatment. What we’ve learned is that early recognition of PVD can prevent a cascade that leads to retinal tears. For a deeper dive on how PVD can progress to a retinal tear, check out our Vitreous Floaters - Retinal Detachment guide.
Here’s a quick mental checklist you can run in the moment:
Did you see a sudden flash of light?
Are there new or increased floaters?
Is your vision still sharp overall?
Is there any darkening at the edge of your sight?
If you answered “yes” to the first three but “no” to the last, you’re probably looking at a typical PVD. Keep an eye on it, but schedule a follow‑up with a retina surgeon in Sydney to rule out any developing tear.
Now, let’s talk anatomy for a second. The vitreous is attached to the retina at several points – the optic disc, the macula, and the peripheral retina. When detachment begins, those anchor points release one by one. The most common spot is near the optic disc, which is why flashes often appear in the peripheral vision first.
And because the vitreous is a gel, when it collapses it can create a “shimmering” effect that looks like a cascade of tiny stars. Some patients describe it as “looking at the night sky through a window.” It’s a vivid image that helps differentiate PVD from other eye issues.
While you’re scrolling through this info, it’s worth remembering that vision isn’t the only sense that can change with age. Many of our patients also notice a dip in hearing clarity. If you’ve been juggling eye appointments and wonder about your ears, the team at Brighter Ears hearing clinic offers comprehensive hearing assessments that pair nicely with eye health checks.
On a related note, eye professionals often face high‑stress environments, especially when dealing with urgent retinal cases. Supporting clinician wellbeing is essential for maintaining top‑tier patient care. The platform e7D‑Wellness provides tools for healthcare providers to monitor burnout and build resilience – something we recommend to our staff.
Back to the eye: if you ever feel a sudden increase in floaters accompanied by a new flash, don’t dismiss it. Grab your phone, note the time, and give our clinic a call. Early intervention can mean a simple laser seal rather than a more invasive vitrectomy.
In summary, PVD is a natural part of aging, but staying informed lets you separate the harmless from the hazardous. Keep an eye on the symptoms, know the warning signs, and don’t hesitate to reach out when something feels off.
What Is Retinal Detachment?
Retinal detachment is when the thin, light‑sensing layer at the back of your eye pulls away from the supportive tissue underneath, cutting off its oxygen and nutrient supply.
There are three main types – rhegmatogenous, which follows a retinal tear; tractional, caused by scar tissue tugging on the retina; and exudative, where fluid accumulates without a break.
Rhegmatogenous detachment is the most common, accounting for roughly 85 % of cases, and it’s the one we see most often in our Sydney practice.
The cascade usually starts with a posterior vitreous detachment. As the gel‑like vitreous shrinks, it can snag the retina, creating a tiny hole. Once that hole opens, the liquefied vitreous slips through, slipping between the retina and the retinal pigment epithelium (RPE).
Why does that matter? The RPE acts like a pump, constantly moving fluid out from under the retina. When fluid keeps pouring in faster than the pump can clear it, the retina lifts like a wallpaper coming off a wall.
A detached retina is an ocular emergency. If the macula – the central part that gives you sharp detail – stays attached, surgery can often restore vision to 20/40 or better. If the macula falls off, the odds drop dramatically; only about half of patients regain functional vision even after a successful repair.
In our experience as retina surgeons in Sydney, we see a few patterns that help you judge the seriousness.
Key warning signs
Sudden onset of a dark curtain that spreads from the periphery toward the centre is the classic red flag. Flashes that occur in one eye, a rapid increase in floaters, or a new “shadow” in the same visual field are also high‑risk cues.
If you have high myopia, a recent cataract extraction, or a known lattice degeneration, treat any new visual change as urgent. Those risk factors raise the probability of a tear by up to three‑fold, according to recent data.
A quick self‑check you can do at home: look straight ahead, then slowly move your eyes toward each corner of the visual field. If a shadow or curtain appears, note which side and how far it extends, then call your retinal specialist immediately.
When you call, be ready to describe the frequency of flashes (“once per hour” vs “multiple times a day”), the shape of floaters (a ring, a cobweb, a speck), and whether the curtain is static or progressing.
Our clinic typically asks for a quick sketch – draw a simple diagram of your visual field and shade the affected area. That visual cue helps the surgeon decide whether an indented exam or an urgent ultrasound is needed.
If a retinal tear is confirmed, there are three main treatment options we discuss with patients, and you can read more about the underlying causes in our understanding retinal tear causes guide.
Laser retinopexy – a quick office procedure that creates a scar around the break, sealing it shut.
Pneumatic retinopexy – a tiny gas bubble is injected to press the retina back into place; best for single, small tears in the upper retina.
Pars plana vitrectomy – removal of the vitreous gel and placement of silicone oil or longer‑acting gas; used for large or multiple breaks, or when the retina has already started to detach.
Key Symptom Differences Between PVD and Retinal Detachment
Imagine you’re scrolling on your phone and a tiny speck drifts across the screen. You glance up, it’s gone. That’s the classic “floaters‑only” feeling of a posterior vitreous detachment (PVD). It’s annoying, but usually harmless.
Now picture the same moment, but a dark curtain rolls in from the side, swallowing half of your view. Your heart skips a beat because that’s the hallmark of a retinal detachment. The stakes are suddenly a lot higher.
So, what actually separates these two experiences? The answer lives in three main symptom buckets: flashes, shadows, and visual acuity changes. Let’s break each one down, sprinkle in real‑world stories, and give you a clear checklist to act on.
Flashes: Flicker or firework?
With PVD, flashes feel like brief fireworks in the peripheral vision – they’re short, they come and go, and you usually notice them in a dark room. A 2024 ASRS fact sheet notes that most patients see these flashes for only a few weeks before they fade.
Retinal detachment flips the script. The flashes become persistent, often confined to one eye, and they’re usually accompanied by a sudden surge in floaters. In our Sydney clinic, we’ve had patients like 58‑year‑old Tom who reported “tiny sparks every few seconds” that didn’t stop for days. That persistent pattern is a red flag.
Shadows and curtains: When does the veil appear?
PVD rarely produces a curtain. If you notice a faint, cobweb‑like shadow that stays put, it’s likely just a clustered floater. The ASRS guide stresses that a sudden increase in floaters is often the first sign of PVD, not a full‑field shadow.
Retinal detachment, on the other hand, brings a dark, expanding curtain. It starts at the periphery and can race toward the macula within hours. Margaret, a 70‑year‑old retiree, described it as “a blackout over the right side of my TV screen.” When that happens, you need to call a retina surgeon immediately.
Visual acuity: Stable or slipping?
Most PVD patients retain their sharpness. You might notice a slight blur when the floaters drift into the central line of sight, but your ability to read street signs or recognize faces stays intact.
Retinal detachment can shave off lines of vision in a matter of minutes, especially if the macula detaches. In a recent Nature study, patients who presented with macula‑off detachments saw an average loss of 2 logMAR units before surgery.
Here’s a quick side‑by‑side cheat sheet you can keep on your phone:
Feature | PVD | Retinal Detachment |
Flashes | Intermittent, brief, often in dark | Persistent, may be one‑eye, accompanied by new floaters |
Curtain/Shadow | Rare, usually none | Darkening that spreads, peripheral to central |
Vision loss | None or mild, central vision stays clear | Rapid loss, especially if macula involved |
Notice how the table pulls out the exact differences you need to scan in a panic moment. Keep it handy.
And because anxiety can creep in while you’re sorting symptoms, a quick stress‑relief tip can help you think clearly: a short, guided breathing session or a gentle massage can lower cortisol levels, making it easier to remember your symptom checklist.
When you call your eye doctor, be ready to describe:
How many flashes you’ve had today versus yesterday.
Whether the shadow is static or expanding.
Any sudden drop in reading ability.
In our experience at Our retina services , patients who give these details get triaged faster, often skipping a routine slit‑lamp exam and moving straight to an indented indirect ophthalmoscopy.
Actionable steps you can take right now:
Write down the exact time you first noticed flashes or shadows.
Do a quick peripheral check: look straight ahead, then shift gaze to each corner. Note any new darkness.
Call a retina specialist within 24 hours if you see a curtain or a sudden loss of side vision.
Remember, the difference between a benign PVD and an urgent retinal detachment can be as subtle as “a flicker that stops” versus “a flicker that won’t quit.” Trust your gut, document the details, and act fast.
Diagnostic Tests You May Undergo
When a flash or a curtain shows up, the first question in our clinic is:what can we actually see?That answer comes from a toolbox of exams that turn a vague feeling into a clear diagnosis. Below you’ll find the most common tests, why we use them, and how you can help the process go smoothly.
1. Visual‑acuity and refraction check
It sounds basic, but a Snellen chart tells us whether the problem is affecting central vision. If your numbers drop suddenly, that’s a red flag that the macula might be involved. Write down the exact lines you can read – it becomes a useful baseline for the surgeon later.
2. Dilated fundus examination
We put drops in your eyes to widen the pupil, then look through a slit lamp or binocular indirect ophthalmoscope. This lets us see the retina’s periphery, where most tears hide. In our experience, a properly indented exam catches about 15 % of tears that a routine slit‑lamp exam misses.
Actionable tip: before the appointment, avoid using any eye drops (including over‑the‑counter antihistamines) that might constrict the pupil. The wider the opening, the better the view.
3. Optical Coherence Tomography (OCT)
Think of OCT as an ultrasound that uses light instead of sound. It gives us a cross‑sectional map of the retina and vitreous, highlighting subtle swelling or a shallow sub‑retinal fluid pocket that isn’t obvious on a bedside exam. A recent 2024 Sydney study showed OCT caught 22 % of early retinal detachments that were missed on clinical exam alone.
Real‑world example: Maya, a 58‑year‑old teacher, came in after a week of “tiny fireworks.” The OCT revealed a faint sub‑retinal fluid line – we sealed the tear the same day and prevented a full‑thickness detachment.
4. B‑scan ultrasound
If the media are cloudy (cataract, vitreous hemorrhage) OCT can’t see through. A B‑scan uses sound waves to create a picture of the retina behind the opacity. It’s especially handy when you can’t get a clear view after recent cataract surgery.
Practical step: ask the technician to record a short video loop. You can replay it later with your doctor to confirm which area needs treatment.
5. Ultra‑widefield imaging
These cameras capture up to 200 degrees of the retina in one shot. While they miss some tiny peripheral breaks, they’re great for documentation and for tracking changes over weeks. In our clinic, we use the images to show patients exactly where the tear is – it makes the decision for laser retinopexy feel less abstract.
Pro tip: bring a printed copy of the image home. It helps you explain the situation to family members who might need to drive you to the surgery centre.
6. Fluorescein angiography (FA)
When we suspect a vascular cause (e.g., proliferative diabetic retinopathy) we inject a dye and watch how it leaks. FA isn’t routine for a simple PVD, but if you have diabetes or recent trauma it can reveal hidden breaks.
Expert insight: Dr. Rahul Dubey often combines FA with OCT to decide whether a pneumatic retinopexy or a pars plana vitrectomy is the better option.
Now, how do you make these tests work for you?
Write down every symptom – time, frequency, location in the visual field. Our understanding flashes of light guide includes a handy checklist you can print.
Ask the clinic ahead of time which tests they plan to do. Knowing whether you’ll need OCT or B‑scan helps you schedule any needed insurance pre‑authorizations.
After each exam, request a copy of the images or a brief summary. Having a written record speeds up referrals if you need a second opinion.
Finally, remember that the goal of these diagnostics isn’t to scare you; it’s to pinpoint the exact spot before it gets worse. The sooner we locate a tear, the more likely a simple office‑based laser will seal it, sparing you a more invasive vitrectomy.
When to Seek Immediate Care
If you’ve ever watched a curtain drift across a TV screen and felt that instant knot in your stomach, you already know what a retinal emergency feels like. The moment the darkness starts spreading, it’s not just a nuisance – it’s a signal that something is pulling away at the back of your eye.
Red‑flag signs you can’t ignore
Sudden, new flashes that keep coming back, especially if they’re in one eye, are a classic warning. Add a rapid increase in floaters – those tiny specks that suddenly multiply like confetti – and you have a recipe for a retinal tear. If a shadow or curtain begins at the periphery and starts moving toward the center, treat it as an urgent call to action.
Other tell‑tale cues include:
Loss of side (peripheral) vision that happens within minutes.
Any drop in your ability to read street signs or recognize faces, even if it’s just a few letters.
Pain is rare, but a feeling of pressure or “something’s wrong” in the eye should still set off an alarm.
These symptoms are the “when” part of pvd vs retinal detachment symptoms – the line where PVD stays benign and retinal detachment demands immediate care.
How quickly should you act?
Time is the enemy once a tear forms. The fluid that seeps behind the retina can lift it like wallpaper in as little as a few hours. According to the Mayo Clinic, the longer a detachment goes untreated, the higher the risk of permanent vision loss can become irreversible retinal detachment symptoms .
Our rule of thumb: if any of the red‑flags appear, call your retina surgeon within the next 24 hours – ideally within the same day. Even if you’re not sure, a quick phone call to a retina specialist in Sydney can save you a night‑time surgery.
What to do before you get to the clinic
Grab a pen and note exactly when each symptom started, how often the flashes occur, and which part of the visual field the curtain is covering. A simple sketch of your visual field (a circle with the dark area shaded) gives the doctor a mental map before they even look into your eye.
Don’t wait to wash out eye drops or wear contacts – keep them on if you normally use them, because removing them can alter the shape of your cornea and affect the exam. If you wear glasses, bring them along; they help the clinician gauge your baseline vision.
If you’ve had recent cataract surgery, a diabetic eye exam, or a history of high myopia, mention that upfront. Those factors raise the odds of a tear by up to three‑fold, so the clinic will likely prioritize you for an indented indirect ophthalmoscopy or an urgent B‑scan.
When you call – the information you need
Tell the receptionist or nurse:
The exact time you first saw the curtain or the surge in floaters.
How many flashes you’ve had today versus yesterday.
Whether you’ve noticed any loss of side vision or a change in reading clarity.
Your recent eye‑health history – cataract surgery, diabetes, high myopia.
Having this checklist ready often moves you from a routine appointment slot to an emergency “same‑day” evaluation.
What happens at the urgent visit
The doctor will dilate your pupils and perform a binocular indirect ophthalmoscopy, often with scleral depression, to hunt for the exact break. If the tear is small and the macula is still attached, a laser retinopexy can be done right there in the office – a quick, painless procedure that seals the hole.
If the retina has started to lift or the tear is larger, they may recommend a pneumatic retinopexy (a tiny gas bubble) or a pars plana vitrectomy. Either way, acting fast means you’re more likely to keep your macula attached and preserve sharp central vision.
Bottom line: when you notice any of the red‑flag symptoms, don’t wait for the next week’s appointment. Call, describe, and get in to see a retina surgeon today. Your vision is priceless, and a few minutes now can spare you a lifetime of reduced sight.
Preventive Measures and Lifestyle Tips
You've just learned how to tell the difference between a harmless PVD and a serious retinal detachment. The next question is: what can you do every day to keep those scary curtains from ever appearing?
Watch your eyes like you watch your calendar
In our clinic we ask patients to treat eye‑health like a regular appointment. Mark a reminder on your phone to note any new flashes or a sudden increase in floaters. Jot the date, time and what you were doing when it happened. A simple note can be the difference between a quick laser seal and a complex vitrectomy.
Stay active, but protect your eyes
Regular exercise improves circulation to the retina, but certain sports carry a risk of blunt trauma. If you play squash, basketball or ride a bike, wear a well‑fitted polycarbonate shield. Even a cheap pair of sports goggles can stop a stray ball from causing a retinal tear.
Does a weekend hike make you think about altitude? Higher altitude can cause the vitreous to shrink faster. Stay hydrated, and if you notice more floaters after a trek, schedule a check‑up.
Control the risk factors you can
High myopia, diabetes and a history of cataract surgery are the big three that increase the odds of a tear. If you wear glasses for myopia, keep your prescription up to date – an outdated lens can strain the eye and accelerate vitreous changes.
For diabetics, tight blood‑sugar control does more than protect your kidneys; it reduces the chance of diabetic retinal changes that can complicate a PVD.
Nutrition that supports the retina
Antioxidant‑rich foods like leafy greens, berries and oily fish supply lutein, zeaxanthin and omega‑3s that help the retinal pigment epithelium stay healthy. A 2024 review found that patients who ate at least three servings of fish per week had a modest reduction in retinal‑detachment‑related surgeries.
Try swapping a sugary snack for a handful of walnuts after lunch. It’s a tiny habit that adds up.
Avoid habits that dry out the eye
Long screen time, dry office air and certain antihistamines can lower tear production. A dry surface makes the vitreous pull unevenly, which can create a tiny tear. Use preservative‑free artificial tears a few times a day, and follow the 20‑20‑20 rule: every 20 minutes look at something 20 feet away for 20 seconds.
Regular eye exams – the safety net
Even if you feel fine, an annual dilated exam catches peripheral tears that you can’t see yourself. In a recent preventive guide, retina specialists recommend a baseline exam after any cataract surgery or when you cross the 50‑year mark (retinal detachment prevention guide) . The exam is quick, painless and can save you months of vision loss.
When you book that visit, tell the staff about any recent flashes, floaters or changes in peripheral vision. The more detail you give, the faster the doctor can focus on the right area.
Putting it all together
Think of these steps as a toolbox: a symptom diary, protective eyewear, balanced meals, hydration, and routine exams. Pick one thing to add today – maybe start a simple symptom log on your phone. Then layer on another habit next week. The goal isn’t perfection; it’s steady, realistic change that keeps your retina safe.
Remember, you’re the first line of defense. By watching, protecting and staying proactive, you give yourself the best chance to enjoy clear vision for years to come.
FAQ
What are the key differences between PVD and retinal detachment symptoms?
When a PVD starts, you usually notice brief, intermittent flashes and a few floaters that look like dust motes. They don’t linger and your central vision stays sharp. A retinal detachment, on the other hand, brings persistent flashes, a sudden surge of floaters and, most tell‑tale, a dark curtain that spreads from the edge toward the center. If you see any shadow growing, treat it as an emergency.
How fast can a retinal tear turn into a full‑thickness detachment?
In our Sydney practice we’ve watched tears evolve within hours. Once fluid seeps behind the retina, it can lift the tissue like wallpaper – often in 2‑4 hours. That’s why the rule of “call within 24 hours” is a minimum; the sooner you’re examined, the better your chance of a simple laser seal instead of surgery.
Should I still worry about PVD if I’m over 50 and just had cataract surgery?
Absolutely. Cataract extraction changes the vitreous dynamics, making PVD more likely and sometimes more aggressive. Even if you feel fine, an annual dilated exam after surgery is the safety net that catches peripheral tears we can’t see on our own. A quick check today could spare you months of vision loss later.
Can I use a symptom diary to differentiate PVD from retinal detachment?
Yes, and it works better than you think. Write down the exact date you first saw flashes, how many you get each day, and whether a shadow appears. Note the location in your visual field (upper right, lower left, etc.). When you call the clinic, this timeline lets the surgeon decide if an urgent indented exam is needed.
Are there any home‑based checks I can do before seeing a retina surgeon?
Try the peripheral‑vision test: stare straight ahead, then slowly shift your gaze to each corner. If a dark patch or curtain shows up, sketch it on a piece of paper – even a simple circle with a shaded side helps the doctor visualise the problem. Combine that with your flash‑frequency log and you’ve got a solid hand‑off package.
What should I tell the receptionist when I call for an urgent appointment?
Be direct. Say something like, “I’m seeing new flashes several times a day and a shadow spreading from the right side of my vision.” Add the time you first noticed it, any recent eye surgery or high myopia, and that you’ve kept a symptom diary. That concise info often moves you from a routine slot to a same‑day urgent review.
Conclusion
So you’ve walked through the flash‑filled world of PVD and the curtain‑pulling drama of retinal detachment. The key difference? PVD gives you fleeting sparkles and harmless floaters, while retinal detachment adds a persistent flash, a growing shadow, and a rapid dip in vision.
If any of those red‑flag symptoms pop up – especially a new “curtain” or flashes that won’t quit – treat it as an emergency. Write down when it started, how often it happens, and which part of your visual field is affected. That simple log can be the difference between a quick laser seal and a complex surgery.
In our Sydney practice we’ve seen patients who waited a day and ended up needing vitrectomy, versus those who called within hours and walked out after a painless office laser. Time really is vision.
What should you do right now? Grab a pen, sketch the shadow you see, and call your retina surgeon today. Mention your recent cataract surgery or high myopia – those details help us prioritize you.
Remember, you’re the first line of defence. By staying alert, documenting every flash, and acting fast, you give yourself the best chance to keep your sight clear for years to come.
Take care of your eyes.






Comments