Macular Hole Causes: A Comprehensive Guide to Understanding and Prevention
- Dr Rahul Dubey
- 1 day ago
- 16 min read
Ever caught yourself squinting at a newspaper headline, only to realize the words are blurry in the middle? That tiny, unsettling spot could be the early whisper of a macular hole, and you’re not alone—many people notice it after years of clear vision.
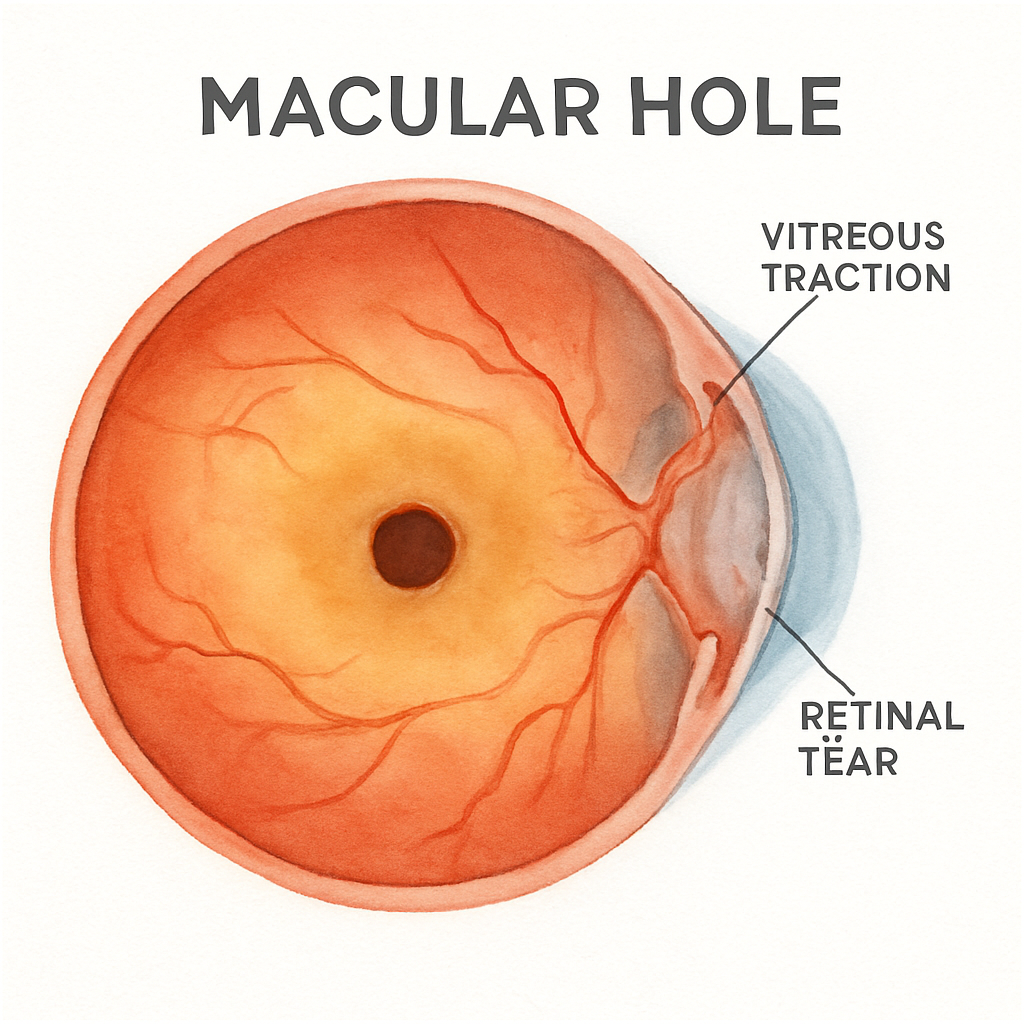
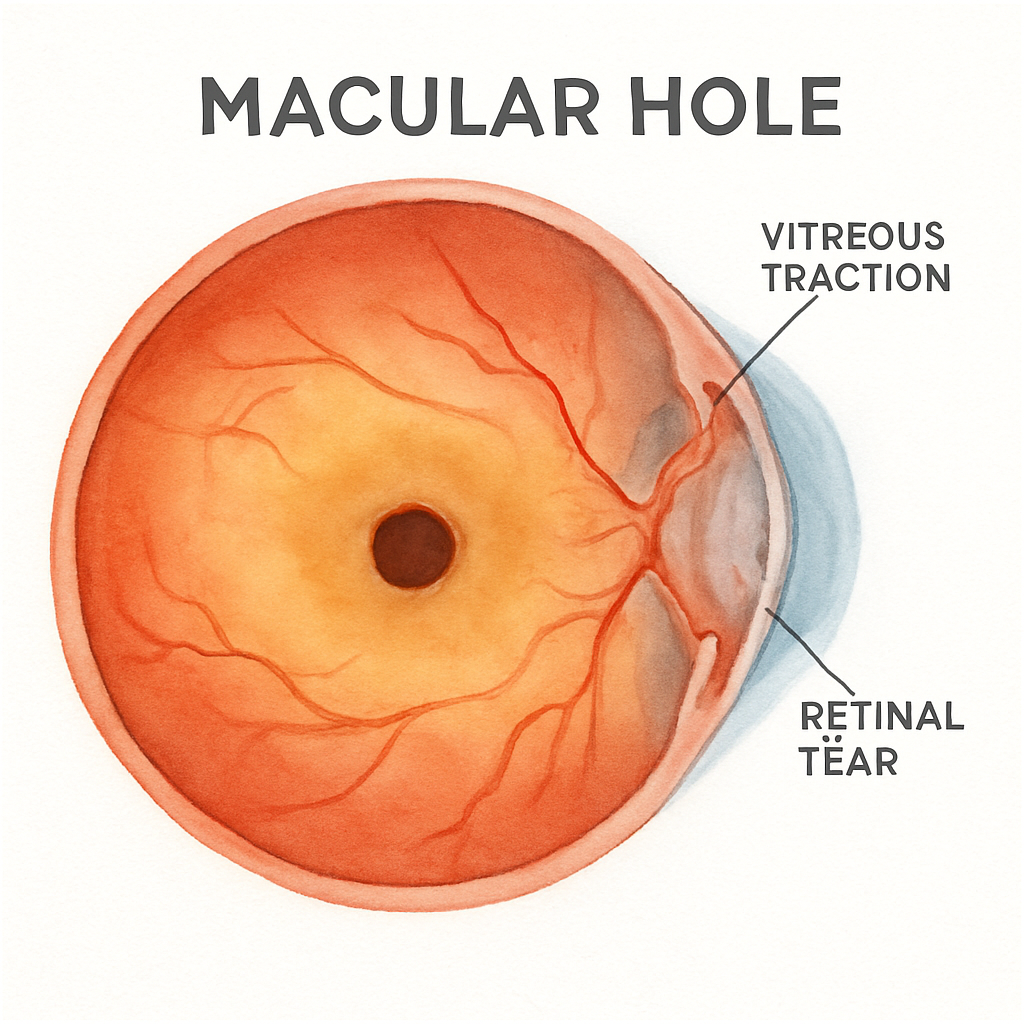
Understanding macular hole causes helps you spot the red flags before they turn into permanent vision loss. The most common trigger is a natural aging process called posterior vitreous detachment (PVD). As the gel‑like vitreous shifts away from the retina, it can tug on the delicate macula, creating a tiny tear that widens over time. Think of it like a loose thread pulling at a fabric seam.
But it’s not just age. High myopia, or severe nearsightedness, stretches the retina, making it more vulnerable. A person with a prescription of –8.00 diopters or worse often experiences thinner retinal tissue, which can crack under minimal stress. For example, Sarah, a 58‑year‑old graphic designer, noticed a dark spot after years of wearing contacts; her doctor linked it to her long‑standing myopia.
Eye injuries also play a role. A blunt impact—say, a sports ball hitting the eye—can cause sudden vitreous movement, instantly creating a macular hole. Even minor surgeries on the eye, like cataract removal, sometimes disturb the vitreous enough to spark a hole, though this is relatively rare.
Systemic health matters, too. Conditions that affect blood vessels, such as hypertension or diabetes, can compromise retinal circulation, weakening the macula. A study of patients over 60 showed that those with uncontrolled blood pressure had a 1.5‑times higher risk of developing macular holes compared to normotensive peers.
So, what can you do right now? First, schedule a comprehensive retinal exam if you’re over 50, have high myopia, or notice any sudden central blur. During the check‑up, ask your doctor about the Macular Hole | Dr Rahul Dubey page to see visual examples and learn about early‑stage treatment options. Second, keep systemic conditions in check—regularly monitor blood pressure and blood sugar levels. Third, protect your eyes during sports or DIY projects with appropriate safety glasses.
Finally, if you experience a new central dark spot, flashing lights, or distorted straight lines, act quickly. Early intervention, often with a vitrectomy or gas tamponade, can close the hole and restore vision. You don’t have to accept blurry central vision as “just getting older”—understanding the causes empowers you to take control.
TL;DR
Macular hole causes include aging‑related vitreous detachment, high myopia, eye trauma, and systemic vascular issues like hypertension or diabetes. If you notice sudden central blur, schedule a retinal exam, manage blood pressure and sugar, and protect your eyes to catch and treat holes early before vision declines significantly for you.
Understanding Macular Hole Causes
When you first notice a dark spot in the middle of your vision, it can feel like your world has taken a tiny, unwanted shortcut. You might wonder, “Is this just age, or is something more serious happening inside my eye?” The answer often lies in a handful of surprisingly common triggers that tug, stretch, or scar the macula.
Let’s break them down so you can recognize the warning signs before they turn into permanent vision loss.
Age‑related vitreous changes (Posterior Vitreous Detachment)
As we get older, the gel‑like vitreous that fills the eye slowly collapses and pulls away from the retina. This process, called posterior vitreous detachment (PVD), is the single biggest driver ofmacular hole causes. When the vitreous tugs too hard, it can create a tiny tear in the central retina. Think of it like a loose thread snagging the seam of a favorite shirt – one pull, and a small hole appears.
If you’ve ever felt a sudden “floaters‑and‑flashes” episode, that’s often the vitreous saying it’s moving. In many cases the eye adapts, but for some, especially those with a predisposition, the tear widens into a macular hole.
High myopia – the stretched retina
Severe nearsightedness stretches the retina thin, making it vulnerable to even minor stress. People with prescriptions of –8.00 diopters or worse often have a retinal layer that’s barely holding together. A gentle head movement or a routine eye exam can sometimes be enough to trigger a hole.
Sarah, a 58‑year‑old graphic designer, thought her blurry spot was just “eye strain”. A quick retinal scan revealed a myopia‑related macular hole that was caught early enough for a simple surgery.
Trauma and ocular surgery
A blunt impact – say, a basketball hitting the eye during a weekend game – can jolt the vitreous and instantly create a macular hole. Even cataract surgery, while generally safe, can disturb the vitreous enough to cause a hole in rare cases.
Because these events are sudden, you’ll often notice a rapid change in central vision, sometimes accompanied by a “black spot” that seems to grow overnight.
Systemic vascular health
Conditions that affect tiny blood vessels, like hypertension or diabetes, subtly weaken the macula’s support network. Poor circulation means the retinal tissue doesn’t get the oxygen it needs, and over time that can lead to micro‑tears that evolve into macular holes.
Keeping blood pressure and blood sugar in check isn’t just good for your heart – it’s a direct line of defense for your central vision.
For a deeper look at what a macular hole looks like and why early detection matters, check out Macular Hole | Dr Rahul Dubey . The page walks you through real‑world images and explains the treatment options we offer in Sydney.
So, how do you protect yourself? First, schedule a comprehensive retinal exam if you’re over 50, have high myopia, or notice any sudden central blur. Second, manage systemic health – a simple daily blood pressure check can be a lifesaver for your eyes.
And here’s a practical tip you might not expect: using an AI‑powered reminder system can keep your follow‑up appointments on track. Platforms like Assistaix let you set automated alerts for eye‑doctor visits, medication refills, and vision‑screening reminders, so you never miss a critical check‑up.
Watching a short video on macular hole formation can help you visualize what’s happening inside the eye – it’s surprisingly clear once you see the retina in motion.
Beyond your own health, if you’re a fellow eye‑care professional looking to boost your online presence, consider partnering with a reputable SEO service. Companies like Rebelgrowth specialize in building authority for medical practices, helping patients find the right specialist when they need it most.
Bottom line: macular hole causes are often a mix of natural aging, structural eye factors, trauma, and overall vascular health. By staying vigilant, managing systemic risks, and using smart tools for reminders, you give yourself the best chance to catch a hole early and preserve the clear, central vision you rely on every day.
Age‑Related Factors and Macular Hole Development
When you hit your late 50s or early 60s, you might notice the world looking a little fuzzier in the center. That’s not just “getting older” – it’s the eye’s own aging process tugging at the macula. The most common driver is posterior vitreous detachment (PVD), where the jelly‑like vitreous slowly separates from the retina. As it pulls away, tiny traction forces can concentrate right over the macula, eventually punching a microscopic hole.
But age‑related change isn’t a single event. It’s a cascade. The vitreous shrinks, the retina thins, and the supporting collagen framework weakens. Think of an old rope that’s lost its elasticity – one sudden snap and the knot loosens. In a 2023 Mayo Clinic overview, experts note that retinal tissue becomes more fragile with age, making it easier for traction to translate into a macular defect.
Real‑world example: Maria, a 62‑year‑old retired teacher from Sydney, started seeing a “shadow” while reading her favorite mystery novel. She thought it was just fatigue, but her ophthalmologist spotted a stage‑2 macular hole linked to PVD. Early surgery restored her reading comfort – a reminder that age‑related factors are often silent until they strike.
High myopia accelerates this wear‑and‑tear. A stretched‑out eye means the retina is already under tension, so when the vitreous finally detaches, the macula bears the brunt. In people with prescriptions worse than –6.00 diopters, the risk of a hole jumps significantly. If you fall into that category, keep a close eye on any new central blur.
Systemic health also sneaks into the picture. Hypertension and diabetes can compromise the tiny blood vessels feeding the macula, reducing its ability to repair micro‑tears. A study cited by the Mayo Clinic shows that uncontrolled blood pressure raises the odds of macular holes by about 1.5‑times. Managing these conditions is a practical step you can take right now.
Actionable checklist for age‑related risk:
Schedule a retinal OCT annually once you’re past 50, or sooner if you’re highly myopic.
Ask your doctor about PVD status during any eye exam.
Track blood pressure and blood sugar weekly; aim for the targets your GP recommends.
Stay active – gentle cardio improves circulation to the retina.
Consider a brief discussion about Age‑Related Macular Degeneration to see how overlapping risk factors might affect you.
Another subtle factor is inflammation. Chronic low‑grade inflammation, whether from diet, stress, or even seasonal allergies, can make the vitreous‑retina interface more susceptible to traction. Some patients have found relief by incorporating anti‑inflammatory lifestyle habits – omega‑3 rich foods, regular sleep, and stress‑reduction techniques. If you’re looking for a complementary approach, halotherapy (salt‑room therapy) is reported to help reduce systemic inflammation, which may indirectly support retinal health.
So, what should you do if you spot a new “spot” or distortion? First, don’t panic, but don’t ignore it either. Book an appointment within two weeks. Early vitrectomy or gas tamponade can seal the hole before vision loss becomes permanent. Second, bring a list of your recent health changes – new meds, blood pressure spikes, or recent injuries – to help your surgeon pinpoint the trigger.
Finally, remember that age‑related macular hole development is often a combination of factors, not a single cause. By staying vigilant, managing systemic health, and addressing vitreous changes early, you give yourself the best shot at preserving clear central vision well into your golden years.
Trauma and Eye Injuries Leading to Macular Holes
Ever felt a sudden jolt in your eye after a basketball hit or a hammer slip, and then noticed a tiny dark spot in the center of your vision? That moment is more than a fleeting annoyance – it can be the first sign of a macular hole caused by trauma.
Blunt trauma sends a shock wave through the vitreous gel, pulling and shearing the delicate macular tissue. The force is often enough to create a micro‑tear that widens as the eye’s natural healing processes kick in. In many cases the hole doesn’t appear immediately; you might only notice distortion a few days later when straight lines start to bend.
Think about a weekend soccer game. You dive for the ball, the impact lands square on the globe, and the next morning you see a small “smudge” while reading your text messages. That’s a classic example of vitreomacular traction triggered by a sudden impact. Studies show that up to 20 % of macular holes in patients under 50 have a history of such blunt injury.
Penetrating injuries and surgical mishaps
A penetrating wound – a shard of glass or a metal fragment – can directly lacerate the macula. Even when the entry wound is peripheral, the ensuing inflammation and vitreous shift can still focus stress on the central retina.
Eye surgeries aren’t exempt. Cataract extraction or intravitreal injections occasionally disturb the vitreous enough to generate a hole, especially if the eye already has a thin retina from high myopia. The key difference is that surgical trauma is usually planned, so you have a chance to catch any early changes during post‑op follow‑up.
After you’ve watched the short video above, keep this in mind: not every hole shows up right away. Some patients report a “delayed blur” weeks after the injury, when scar tissue contracts and pulls the macula into a hole.
Quick comparison of trauma‑related triggers
Trigger type | Typical mechanism | Onset of symptoms |
Blunt impact (sports, falls) | Sudden vitreous shock causing traction | Hours to days |
Penetrating injury (glass, metal) | Direct macular laceration + inflammation | Immediate to few days |
Iatrogenic (cataract surgery, injections) | Vitreous displacement in already thin retina | Days to weeks |
Knowing which scenario fits your story helps you decide how fast to act. If you’ve just suffered a hit, schedule an urgent retinal OCT within 48 hours. For surgical cases, attend every post‑op check‑up and mention any new central blur right away.
When you’re trying to piece together the cause, it can be useful to review the full symptom checklist. A helpful resource that walks you through what to watch for is Understanding macular hole symptoms: What to watch for and when to act . It breaks down the visual clues that separate a harmless floaters burst from a genuine macular hole.
Bottom line: trauma‑related macular holes are preventable if you catch them early. Keep a symptom diary, protect your eyes with safety glasses during high‑risk activities, and never ignore a new central distortion. Prompt evaluation and, when needed, a vitrectomy can close the hole and restore your vision.
Medical Conditions and Systemic Risks
When you think about a macular hole, the first image that pops up is usually a tiny tear in the center of the retina. But behind that tiny defect is a whole cascade of systemic health issues that can tip the balance.
High blood pressure, for instance, isn’t just a heart problem. It quietly strains the tiny vessels that feed the macula. Over time, those vessels can leak or become too stiff, making the retinal tissue more prone to tearing when the vitreous shifts.
And diabetes? It does more than raise your sugar levels. Chronic hyperglycemia damages the retinal capillaries, reducing oxygen delivery and creating a fragile environment where even a mild vitreous tug can open a hole.
That’s why you’ll often hear clinicians ask about your diabetic eye disease history during a macular hole work‑up. Knowing whether you’ve dealt with diabetic retinopathy gives the surgeon clues about how resilient—or vulnerable—your macula might be.
But blood pressure and sugar aren’t the only culprits. Inflammatory conditions, whether they stem from autoimmune disease, chronic allergies, or even an unhealthy diet, can increase cytokine levels in the eye. Those inflammatory signals make the vitreous‑retina interface stickier, so when the vitreous finally separates (the dreaded posterior vitreous detachment), it does so with extra force.
Think about it like this: imagine pulling a piece of tape off a dusty surface versus a clean one. The dusty side needs a bigger yank. Similarly, inflammation adds “dust” to the retinal surface, amplifying traction.
Recent research on GLP‑1 agonists, drugs commonly used for diabetes and obesity, suggests they might actually dampen that inflammatory environment and even protect against age‑related macular degeneration. The Cleveland Clinic study found a lower incidence of dry AMD among long‑term users, hinting at a broader neuroprotective role that could translate to fewer macular holes, though more eye‑specific trials are needed.
So, what does this mean for you? First, keep your blood pressure in the target range your doctor recommends—usually below 130/80 mmHg for most adults. Second, manage your blood sugar tightly; an A1C under 7% cuts down on micro‑vascular damage. Third, consider lifestyle tweaks that lower systemic inflammation: omega‑3 rich fish, regular moderate exercise, and adequate sleep.
And don’t forget the hidden players like cholesterol. Elevated LDL can clog the retinal micro‑circulation, subtly weakening the macula over years. A simple lipid panel every few years can flag issues before they become a problem for your eyes.
When you’re juggling these health numbers, it helps to track them in one place. Write them down, set phone reminders, or use a health app that syncs with your doctor’s portal. The more consistently you monitor, the quicker you can spot a trend that needs attention.
Now, let’s talk about the practical side of connecting systemic health to macular hole risk. If you’ve been diagnosed with hypertension, ask your ophthalmologist to check the retinal vasculature during your regular eye exam. If you have diabetes, a yearly dilated exam is non‑negotiable—not just for retinopathy, but to catch early signs of macular traction.
And if you’re already on a GLP‑1 agonist, bring that up at your next visit. Your eye doctor might consider it a small piece of the puzzle that tips the scales toward a healthier macula.
Bottom line: macular hole causes aren’t isolated to the eye. They’re a symptom of a larger systemic picture. By tightening control on blood pressure, blood sugar, inflammation, and cholesterol, you’re not just protecting your heart—you’re giving your macula a better chance to stay intact.
Take the next step today: schedule a check‑up for your blood pressure, review your diabetes management plan, and book an eye exam if you haven’t had one in the past year. Small, consistent actions now can prevent a macular hole later.
Preventive Measures and Early Detection
Imagine you’re scrolling through photos on your phone and suddenly a tiny dark spot blurs the center of a loved one’s smile. That moment can feel like a warning bell for a macular hole, but the good news is you can often catch it before it steals your central vision.
Why spotting the problem early matters
Macular hole causes usually stem from subtle shifts inside the eye—think vitreomacular traction that pulls on the macula as the gel‑like vitreous shrinks. When that tug becomes strong enough, a small tear forms and can quickly enlarge. According to Retina Associates of St. Louis , once the hole reaches stage 2, many patients need surgery to close it.
Because the early stages often produce only a faint blur or a few stray floaters, it’s easy to dismiss the symptoms. That’s why regular checks are your safety net.
Everyday habits that lower risk
1.Control blood pressure and blood sugar.Hypertension and diabetes make the tiny vessels that feed the macula less flexible, so any vitreous tug is more likely to rip tissue. Aim for a BP under 130/80 mmHg and an A1C below 7 % if you have diabetes.
2.Stay active.Light‑to‑moderate cardio improves retinal circulation. Even a daily 30‑minute walk can keep the micro‑vasculature supple enough to repair tiny micro‑tears.
3.Eat anti‑inflammatory foods.Omega‑3‑rich fish, leafy greens, and a handful of nuts lower systemic inflammation, which otherwise makes the vitreous‑retina interface stickier.
4.Protect your eyes.Whenever you’re hammering, mowing, or playing contact sports, wear certified safety glasses. A single blunt impact can trigger the same vitreous shock that causes a macular hole in younger athletes.
5.Limit smoking and excess alcohol.Both accelerate retinal aging and raise the odds of vitreous degeneration.
Proactive screening checklist
Here’s a simple, repeatable routine you can slot into your calendar:
Schedule a dilated retinal exam with a retina‑specialist at least once a year after age 50, or sooner if you have high myopia (‑6 D or worse).
Ask the doctor to run an Optical Coherence Tomography (OCT) scan. OCT gives a cross‑sectional view of the macula and can spot vitreomacular traction before a hole even forms.
During the visit, request a quick review of your retinal vasculature—especially if you have hypertension or diabetes. Small vessel changes often show up before you notice any vision shift.
Keep a symptom diary. Note any new central blur, straight‑line distortion, or flashes. Even a one‑week delay in reporting can shrink the window for a painless, outpatient vitrectomy.
When you walk into the clinic, bring a printed list of your recent health numbers (BP, glucose, cholesterol). That tiny extra detail helps the surgeon pinpoint whether a systemic flare‑up contributed to the macular stress.
When to act fast
If you notice any of these red flags, treat them like a fire alarm:
Sudden central dark spot that doesn’t fade in a few days.
Straight lines (like a window frame) that appear wavy or bent.
Frequent flashes of light accompanied by new floaters.
Call your eye doctor within 48 hours and request an urgent OCT. Early vitrectomy with gas tamponade can seal a fresh hole and preserve up to 90 % of central vision, according to clinical experience shared by retinal surgeons.
And remember, you don’t have to wait for symptoms to appear. If you’re already managing hypertension, diabetes, or high myopia, ask your ophthalmologist about a “pre‑emptive” OCT during your next routine check‑up. That quick scan might reveal microscopic traction that you’d never feel.
Bottom line: preventive measures are a mix of lifestyle tweaks, diligent monitoring, and timely specialist visits. By keeping your blood pressure steady, feeding your eyes anti‑inflammatory nutrients, and getting regular OCT scans, you dramatically lower the odds that macular hole causes turn into permanent vision loss.
Take the next 15 minutes now: write down your latest BP and glucose readings, schedule that annual retinal OCT, and slip a pair of safety glasses into your gym bag. Those small steps today can keep your macula—and your life—clear for years to come.
Conclusion
We’ve walked through the main macular hole causes – aging vitreous shifts, high myopia, blunt or penetrating trauma, and systemic health issues like hypertension and diabetes.
The common thread is that each factor creates traction or weakens the retina, turning a harmless float‑flair into a tiny tear that can grow quickly.
That’s why early detection matters. A quick symptom check – sudden central blur, wavy lines, flashes – and an OCT scan can catch the problem before vision is lost.
You can lower your risk today by keeping blood pressure and sugar in range, staying active, eating anti‑inflammatory foods, and wearing safety glasses whenever you swing a hammer or play sport.
Make a habit of jotting down your latest BP, glucose, and any new visual oddities, then schedule a retinal OCT at your next eye‑doctor visit.
If any red flag appears, call your ophthalmologist within 48 hours – early vitrectomy or gas tamponade preserves up to 90 % of central vision, according to retinal surgeons.
Bottom line: understanding the why behind macular hole causes empowers you to act fast and protect the sight you rely on every day.
Ready to take the next step? Book your exam now. Your eyes deserve that extra minute of attention.
FAQ
What are the main macular hole causes?
Most macular holes start with a tug on the central retina. The usual suspects are age‑related posterior vitreous detachment, severe myopia that stretches the retina, blunt or penetrating eye trauma, and systemic health problems like high blood pressure or diabetes. Each of these factors creates traction or weakens the tissue, turning a harmless float‑flair into a tiny tear that can grow quickly.
How does aging lead to a macular hole?
As you get older, the gel‑like vitreous inside the eye slowly shrinks and pulls away from the retina. When that separation happens near the macula, it can create a localized pull—called vitreomacular traction. Over weeks or months that pull can puncture the delicate central retina, especially if the surrounding tissue has already thinned with age.
Can my high myopia increase my risk?
Absolutely. A prescription stronger than about –6.00 diopters means your eye is elongated, which stretches the retina thin. That thin sheet is far less forgiving when the vitreous moves. Even a modest eye movement or a small float‑flair can create enough force to start a hole, so people with high myopia need regular OCT scans to catch early signs.
What kind of eye injuries should I worry about?
Both blunt blows—like a soccer ball hitting the eye—or a sharp object that penetrates the globe can spark a macular hole. A blunt impact sends a shock wave through the vitreous, while a penetrating wound can directly lacerate the macula or cause inflammation that pulls on it later. After any injury, watch for new central blur or wavy lines and seek an urgent retinal exam.
Do systemic conditions like hypertension or diabetes really affect macular holes?
Yes. High blood pressure and diabetes damage the tiny blood vessels that nourish the macula. When those vessels become stiff or leaky, the retinal tissue loses some of its ability to repair micro‑tears. That makes any vitreous traction more likely to turn into a full‑thickness hole. Keeping your BP below 130/80 mmHg and your A1C under 7 % dramatically lowers that risk.
How can I lower my chances of developing a macular hole?
Start with a healthy lifestyle: control blood pressure and blood sugar, stay active, and eat anti‑inflammatory foods like oily fish and leafy greens. Wear safety glasses whenever you’re doing DIY projects or playing contact sports. Schedule a dilated retinal exam with OCT at least once a year after age 50—or sooner if you’re highly myopic. And keep a symptom diary so you can act fast if something changes.






Comments