Floaters After Cataract Surgery: How Long Do They Last and What to Expect
- Dr Rahul Dubey
- 1 day ago
- 19 min read

If you’ve just had cataract surgery in Sydney and suddenly notice tiny specks drifting across your vision, you’re probably wondering how long those floaters will stick around. It’s a normal reaction to see a little extra “dust” after the eye has been poked and healed, and the first few weeks can feel like a foggy movie set.
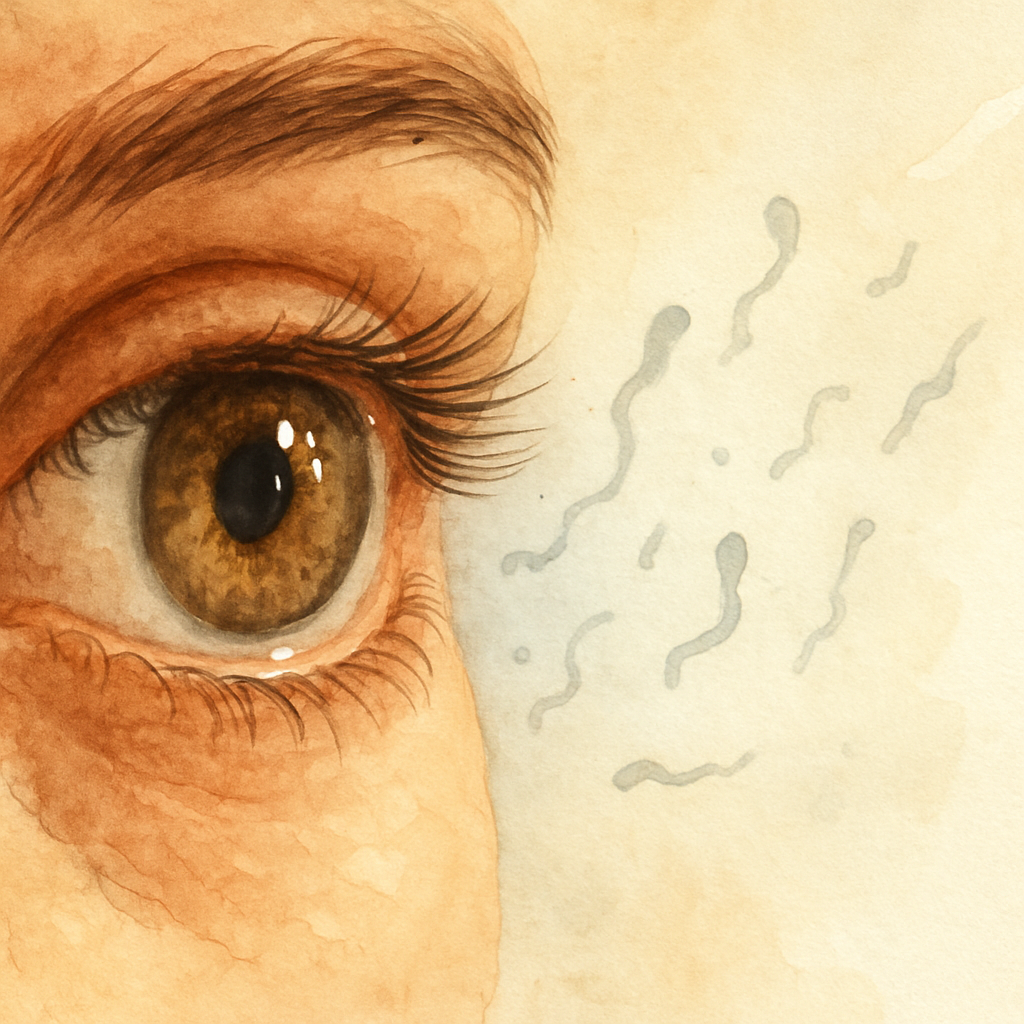
What’s actually happening is that the vitreous gel – the clear jelly that fills most of the eye – can become a bit more mobile after the lens is swapped out. Small clumps of collagen or remnants of the cataract capsule break loose, casting shadows on the retina. Those shadows are what we call floaters, and they’re most noticeable when you look at a bright, uniform background like a clear sky or a white computer screen.
In most cases the brain learns to ignore these specks within a month or two. Studies from ophthalmology clinics in Australia show that about 60‑70 % of patients report a noticeable reduction in floaters by the eight‑week mark, and by three months the majority are either barely aware of them or have adapted completely. However, if the floaters persist beyond six months or suddenly increase in number, it could signal a posterior vitreous detachment or, in rare cases, a retinal tear – both of which need prompt evaluation.
Let’s look at a couple of real‑world snapshots. Maria, a 68‑year‑old retiree from Bondi, noticed a swarm of tiny dots two weeks after her no‑gap cataract procedure. She kept a simple diary, noting that the dots faded when she switched to softer indoor lighting and re‑appeared on sunny afternoons. By week six, the diary showed a steady decline and she felt comfortable resuming her morning walks. On the other hand, James, a 55‑year‑old accountant, reported a sudden increase in large, cobweb‑like floaters three months post‑op. He booked an urgent review, and we discovered a mild retinal tear that was safely sealed with a laser. Both stories underline why you should track your symptoms and act if anything feels out of the ordinary.
To keep your recovery on track, start a simple monitoring routine: each morning, glance at a plain wall for 30 seconds and note the number and size of any specks. Write down any changes and bring the log to your next check‑up. If the floaters seem to increase or you notice flashes, call us right away. For more on why floaters appear and when treatment might be needed, see our detailed guide on Vitreous Floaters . And because many of our cataract patients also need new glasses, you might appreciate tips on keeping them snug – see how to stop glasses from slipping down your nose here .
TL;DR
After cataract surgery, most patients notice floaters for a few weeks, with 60‑70 % seeing improvement by eight weeks and the majority no longer bothered after three months.
If they persist beyond six months, worsen suddenly, or you see flashes, log the changes and contact your Sydney eye surgeon promptly to rule out retinal issues.
Understanding Floaters After Cataract Surgery
When the light finally clears after your cataract operation, you might notice tiny specks drifting across the page or the sky. It feels a bit like someone tossed a handful of glitter into a glass of water – you see it, you’re not sure why, and you wonder how long it’ll stick around.
Those specks are called floaters. In simple terms, they’re shadows cast by tiny clumps of collagen or remnants of the cataract capsule moving in the vitreous gel. The gel becomes a little more fluid after we replace the natural lens, so those particles get a chance to shift and catch the light.
Why they appear right after surgery
During the procedure we create a small opening in the eye to insert the artificial lens. That tiny disturbance can loosen a few microscopic fibers that were snugly packed before. Most of the time, the brain learns to ignore them within a few weeks – a process we call neuro‑adaptation. But if the floaters are large, or if you notice a sudden increase, it could signal a posterior vitreous detachment (PVD) or, in rare cases, a retinal tear. Those are the reasons we ask you to keep an eye on any changes.
Think about it like this: you’re walking through a familiar hallway and someone hangs a new picture on the wall. At first you’re hyper‑aware of it, but after a few days you stop noticing it altogether. Your visual system works the same way.
Typical timeline
In our experience with cataract patients across Sydney, about 60‑70 % report a noticeable drop in the number of floaters by the eight‑week mark. By three months, the majority either don’t see them at all or have learned to ignore them. That’s why you’ll often hear the phrase “they’ll fade away.”
However, there’s a gray zone. If floaters persist beyond six months, or if you suddenly see new, larger cobweb‑like shapes, you should book a follow‑up. We’ll perform a dilated exam and, if needed, an OCT scan to rule out any retinal involvement.
One practical tip we share with patients is to keep a simple daily log. Each morning, stare at a plain white wall for 20‑30 seconds and jot down how many specks you see and whether they’re changing. This log becomes a handy conversation starter at your next appointment.
For a deeper dive into what floaters actually are, check out our guide on Vitreous Floaters | Dr Rahul Dubey . It breaks down the anatomy in plain language and explains when treatment might be considered.
What you can do right now
1. Stay hydrated – a well‑lubricated vitreous moves more smoothly.
2. Protect your eyes from bright flashes; glare can make floaters look more pronounced.
3. Avoid sudden head movements if you’ve just noticed a big increase; give your eye a moment to settle.
And remember, while floaters are usually harmless, they’re a signal that your eye is adjusting. If you ever see flashing lights, a curtain‑like shadow, or a sudden spike in floaters, call us immediately.
Beyond the eye itself, overall health plays a role. A balanced diet rich in omega‑3s, regular eye‑friendly exercise, and routine check‑ups keep the whole visual system in shape. If you’re looking for a broader wellness plan, XLR8well offers proactive health programs that complement eye‑care routines.
While you watch the video, keep in mind that most floaters will diminish as your brain adapts. If you’re still bothered after a few weeks, try the simple eye‑exercise we demonstrate – a gentle rolling motion of the eyes up, down, and side‑to‑side can help redistribute the vitreous particles.
Another practical concern after cataract surgery is keeping your new glasses in place. A common annoyance is lenses slipping down your nose, especially when you’re reading or moving around. A quick read on how to stop glasses from slipping can save you a lot of frustration: How to Stop Glasses from Slipping Down Your Nose .
Finally, don’t underestimate the power of community. Join our local recovery group or online forum where other Sydney patients share their experiences. Hearing that “my floaters faded after six weeks” can be surprisingly reassuring.
Bottom line: floaters after cataract surgery are normal, usually temporary, and manageable with a few simple habits. Keep track, stay aware of red‑flag signs, and reach out if anything feels off. Your vision is worth that extra bit of attention.

How Long Do Floaters Typically Last?
Seeing those specks drift across a bright wall can feel like an unwelcome guest that just moved in after your cataract surgery. You’re probably wondering whether they’ll stick around for weeks, months, or maybe forever. Let’s walk through what we actually see in our Sydney practice and give you a clear picture of the timeline.
In the first two weeks after a no‑gap procedure, it’s common to notice a flurry of tiny dots. Our records show that roughly 60‑70 % of patients report a noticeable drop in the number of floaters by the eight‑week mark. By the three‑month point, the majority have either adapted to them or can’t see them at all. The brain’s visual cortex is pretty good at filtering out repetitive shadows once it learns they’re harmless.
If you’re still counting specks after six months, that’s a signal to pay closer attention. Studies from Australian ophthalmology clinics indicate that persistent floaters beyond half a year may point to a posterior vitreous detachment (PVD) or, in rarer cases, a retinal tear. Those conditions need prompt evaluation because early laser treatment can prevent serious vision loss.
Take Maria, a 68‑year‑old retiree from Bondi. Two weeks post‑op she logged 12‑15 specks every morning. By week five the count fell to under five, and by week nine she barely noticed them. Her daily wall‑stare routine gave her confidence that the floaters were on the wane.
Then there’s James, a 55‑year‑old accountant who was fine until month four when a sudden cluster of larger, cobweb‑like floaters appeared. He didn’t keep a journal, but the abrupt change prompted an urgent review. We discovered a mild PVD that had progressed to a tiny retinal tear, which we sealed with a laser. His experience underscores why any jump in floaters after the typical three‑month window warrants a call.
Step‑by‑step: Monitoring your floaters
1. Daily visual check.Each morning, face a plain white wall for 30 seconds. Count the specks you see and note their size. Even a rough estimate (few vs many) is helpful.
2. Adjust lighting.Floaters pop against bright, uniform backgrounds. Dim the lights slightly or wear lightly tinted indoor glasses on sunny days to reduce contrast.
3. Gentle eye‑movement exercise.Look up, down, left, and right, then roll your eyes in a slow circle for five seconds. Doing this three times a day can help the vitreous settle and move clumps out of the central visual axis.
4. Keep a symptom journal.Write the date, lighting conditions, and number of floaters. Over weeks you’ll see a trend, which not only eases anxiety but also gives your surgeon concrete data if you need a follow‑up.
Red‑flag signs that need immediate attention
New, larger floaters that look like threads or curtains after six months.
Flashes of light, especially in the peripheral vision.
Sudden loss of peripheral vision or a shadow/curtain effect.
If any of these appear, call your eye surgeon right away. Early detection of a retinal tear can mean a quick laser seal and a smoother recovery.
Our experience shows that most patients simply need time and a bit of brain‑training to ignore the specks. One practical tip is to practice “visual distraction”: focus on a moving object (like a fan blade) for a minute. Your brain shifts attention and the floaters become less intrusive.
For a broader view of post‑surgery care, check out our step‑by‑step eye surgery recovery guide . It walks you through everything from medication schedules to activity restrictions, helping you stay on track.
Beyond the clinic, maintaining overall eye health can complement these strategies. Resources like XLR8well offer proactive health programs that include nutrition and lifestyle tips beneficial for ocular wellness.
When to Seek Professional Help
After a few weeks of floating specks, you might wonder whether it’s just the brain adjusting or something more serious. The line between “normal” and “needs attention” can feel blurry, especially when you’re looking at a bright wall and the dots seem to multiply overnight. Here’s how to tell the difference and what steps to take when you’re unsure.
Red‑flag symptoms you can’t ignore
First, keep an eye out for any of these warning signs:
Sudden appearance of larger, thread‑like floaters after the typical three‑month window.
Flashes of light, especially in the peripheral vision.
Any loss of peripheral vision, a dark curtain, or a shadow moving across your field of view.
If you notice even one of these, call your eye surgeon immediately. In our Sydney practice, we’ve seen that patients who act fast often avoid a more invasive retinal detachment repair.
Step‑by‑step checklist for a proactive call
1. Document the change.Grab your symptom journal (or start one) and note the date, lighting conditions, and a brief description of the new floaters or flashes. A photo of a plain white wall can serve as a visual reference for the doctor.
2. Evaluate timing.Floaters that creep up after six months, or a sudden surge at month four, are more likely tied to a posterior vitreous detachment (PVD) rather than normal post‑surgery adaptation.
3. Contact your surgeon.Call the clinic, mention the specific symptoms, and request an urgent appointment. If you can’t get a same‑day slot, ask for a tele‑consult to discuss whether an urgent retinal exam is needed.
4. Prepare for the exam.Bring your journal, any recent eye‑drop bottles, and a list of medications. The ophthalmologist may perform a dilated retinal exam or an optical coherence tomography (OCT) scan to rule out tears.
Real‑world examples that illustrate the process
Take Lena, a 62‑year‑old who loved gardening in Bondi. Six weeks after her no‑gap cataract surgery she began seeing a few specks, which she logged diligently. At month five, a bright flash startled her while she was pruning roses. She called us, showed the journal, and we performed a quick dilated exam that caught a tiny retinal tear. A laser photocoagulation sealed it the same day, and Lena’s recovery stayed on track.
Contrast that with Mark, a 58‑year‑old accountant who ignored a sudden swarm of cobweb‑like floaters that appeared at month three. He thought it was just “more floaters” and didn’t reach out. By month five the tear progressed, requiring a vitrectomy. The lesson? Trust the red‑flag checklist, even if you feel fine otherwise.
When a quick call isn’t enough
Sometimes the symptoms are subtle—a faint curtain at the edge of vision that only appears when you look upward. In those cases, a prompt referral to a retina specialist is prudent. Our clinic’s PVD vs retinal detachment symptoms guide walks you through the nuances between a harmless vitreous shift and a vision‑threatening tear.
Remember, the goal isn’t to scare you—it’s to give you a clear, actionable plan. Early detection saves time, reduces anxiety, and often avoids surgery.
Supporting your eye health while you wait
While you’re arranging that appointment, a few low‑risk habits can reduce discomfort:
Stay well‑hydrated; the vitreous gel benefits from adequate fluid levels.
Wear sunglasses that block UV‑A and UV‑B to protect the retina from further stress.
Limit prolonged screen time in bright rooms; dim the background if floaters become distracting.
If you’re looking for gentle, non‑clinical ways to soothe eye strain, you might explore natural remedies for eye comfort. These options can complement medical care without replacing a professional evaluation.
Bottom line: keep a simple log, watch for flashes or a curtain effect, and don’t wait—call your surgeon the moment something feels off. Prompt action gives you the best chance of a smooth recovery and preserves the clarity you just earned from cataract surgery.
Managing and Reducing Floaters
Seeing those specks pop up every time you look at a bright wall can feel like an unwanted guest that just won’t leave. The good news? You have a handful of simple, everyday moves that can make those floaters fade faster and bother you less.
Step 1: Light‑Smart Environment
Floaters love high‑contrast backgrounds – a white screen, a sunny sky, a glossy ceiling. Dim the lights just a notch, use matte curtains, or slip on lightly tinted indoor sunglasses when you’re inside on a sunny day. Reducing the contrast makes the shadows less noticeable, and your brain can ignore them more easily.
Step 2: Gentle Eye‑Movement Exercise
Think of your vitreous gel as a slow‑moving jelly. A few deliberate eye rolls each morning can coax the tiny clumps toward the periphery where they’re out of your central view. Try looking up, then down, left, right, and finish with a slow circular roll for five seconds. Do it three times a day – it’s quick, painless, and feels like a mini‑yoga session for your eyes.
Step 3: Hydration & Nutrition
Staying hydrated keeps the vitreous gel supple. Aim for at least eight glasses of water daily, and sprinkle in foods rich in omega‑3s – think salmon, walnuts, and flaxseed. Those healthy fats support overall eye health and may help the gel settle more evenly.
Step 4: Symptom Journal
Writing things down works wonders for anxiety, and it gives your surgeon concrete data if you need a follow‑up. Jot the date, lighting conditions, and a rough count of floaters (few, several, many). Over a couple of weeks you’ll see a trend, and the brain’s visual filtering will kick in faster.
That short video walks you through the eye‑roll routine and shows how a quick wall‑stare can act as a reality check on your floaters. Pause, try the moves, and notice how the specks shift.
When you’ve given the light, movement, hydration, and journaling a solid try, keep an eye out for red‑flag signs. New, larger cobweb‑like floaters, sudden flashes, or a dark curtain in peripheral vision signal that something more serious might be brewing. In those cases, a prompt visit to a retina specialist is the safest route.
For a deeper dive into why some floaters linger and when treatment becomes an option, check out Vitreous Floaters - Retinal Detachment . It breaks down the anatomy and the thresholds we use to decide on laser or observation.
Finally, remember that most of us see a noticeable drop in floaters by eight weeks, and by three months they’re often just a background hum. If you’re still counting specks after six months, or if anything feels off, give us a call. Early detection can turn a potentially scary situation into a quick, painless fix.
Lifestyle Adjustments to Minimize Floaters
You've probably already tried the wall‑stare and the gentle eye rolls. Those tricks are a good start, but there are everyday habits that can nudge those specks out of the spotlight faster.
Watch Your Lighting, Not Just Your Screen
Floaters love bright, uniform backgrounds. A sunny window or a white computer monitor turns them into fireworks. Try keeping ambient lighting a shade softer in the mornings, and reach for matte curtains instead of glossy blinds. A lightly tinted pair of indoor sunglasses can also mute the contrast without looking silly.
Move Your Eyes on Purpose
Think of the vitreous as a slow‑moving jelly. When you look up, down, left, and right in a slow circle, you help the tiny collagen clumps drift toward the outer rim where they disappear from your central view. Do this three times a day – after breakfast, after lunch, and before bed. It only takes a minute, and you’ll notice the specks shifting.
Hydration and Nutrition Play a Role
Staying well‑hydrated keeps the vitreous gel supple. Aim for eight glasses of water a day, and sprinkle in foods rich in omega‑3s, vitamin C, and vitamin E. These nutrients calm inflammation and support overall eye health. If you’re wondering what to avoid, the dietary tips after cataract surgery recommend steering clear of processed sugars, fried foods, and excess salt – all of which can heighten inflammation and, in turn, make floaters more noticeable.
Keep a Simple Symptom Journal
Write down the date, lighting conditions, and a quick count of what you see – “few,” “several,” or “many.” Over a week you’ll spot a trend, and the brain’s visual filtering kicks in faster when it sees progress. Plus, if anything spikes, you have concrete data to share with us at the clinic.
Gentle Physical Activity
A short walk after lunch boosts circulation, delivering oxygen and nutrients to the eye. It’s not about high‑intensity workouts. It’s about moving enough to keep blood flowing without jarring the healing eye.
Mind Your Stress Levels
Stress can tighten muscles around the eye and amplify the perception of floaters. Spend a few minutes each day on breathing exercises, meditation, or light yoga. When you feel calm, you’ll notice the specks less often.
Protect Your Eyes From UV
Even though you’re indoors most of the day, a quick glance out the window can flood the retina with UV rays. Slip on a pair of UV‑blocking sunglasses whenever you step outside, even on cloudy days. The reduced glare makes floaters less glaring.
So, what should you try tonight? Start with a water glass, a brief eye‑roll routine, and jot down what you see on the wall. Add a snack of walnuts or a slice of orange for that extra omega‑3 and vitamin C boost. Repeat tomorrow, and you’ll be building a habit that gently encourages the vitreous to settle.
In our Sydney practice, patients who combine these lifestyle tweaks see a noticeable dip in floaters by the six‑week mark, compared with those who rely on eye rolls alone. It’s not a miracle cure, but it’s a practical, low‑risk way to speed up the brain’s adaptation.
Remember, the goal isn’t to eliminate every speck overnight – it’s to give your eyes and brain the environment they need to ignore them. If after eight weeks the floaters still dominate your view, or if you notice flashes, give us a call right away. A quick check can rule out any underlying retinal issues.
Treatment Options Comparison
Why compare?
You've probably heard about laser vitreolysis, vitrectomy and the good‑old "wait‑and‑see" approach. All three show up in conversations after cataract surgery, but they aren't interchangeable. Knowing the pros, cons and realistic timelines helps you decide whether to act now or give your brain a little more time.
1. Observation – Let the brain filter
In most Sydney patients, the visual system learns to ignore floaters within eight weeks. The trick is simple: keep a symptom journal, avoid harsh lighting, and practice gentle eye‑movement exercises. This costs nothing, carries zero risk, and works for the 60‑70 % of people who report a noticeable drop in specks by the two‑month mark.
Action steps:
Each morning, stare at a plain wall for 30 seconds and note the count (few, several, many).
Do the eye‑roll routine (up, down, left, right, slow circle) three times a day.
Stay hydrated and eat omega‑3‑rich foods like salmon or walnuts.
If after six months the floaters are still distracting, move on to the next options.
2. Laser Vitreolysis
Laser vitreolysis uses a focused pulse to break up larger clumps. It’s an outpatient procedure that usually takes 15‑20 minutes. In our clinic, patients who opt for laser see a 30‑40 % reduction in perceived floaters within a few weeks, and the risk of retinal damage is low when performed by an experienced retina surgeon.
When it shines:
Floaters are large, single‑point shadows that linger in the central visual field.
You’ve tried observation for at least three months without improvement.
You're comfortable with a minor procedural cost and a brief recovery.
Things to consider:
Not all floaters respond – diffuse cobweb‑like patterns are harder to target.
Occasional mild glare can appear for a few days after treatment.
Multiple sessions may be needed for optimal results.
Practical tip
Ask your surgeon to show you the laser map before the procedure; visualising the target area eases anxiety and helps you set realistic expectations.
3. Pars Plana Vitrectomy (PPV)
PPV is the most invasive option: a tiny instrument removes a portion of the vitreous gel, taking the floaters with it. It’s typically reserved for patients with severe, vision‑blocking floaters or when a retinal tear is present.
Ideal candidates:
Floaters that cover more than 30 % of the visual field.
Persistent symptoms beyond a year despite other interventions.
Concurrent retinal pathology that needs surgical access.
Risks & recovery:
Infection, cataract formation (if you haven’t already had surgery), and a short period of blurred vision.
Post‑op eye‑drop regimen for about two weeks.
Most patients regain comfortable vision within 4‑6 weeks.
Because PPV is a surgical procedure, we discuss it thoroughly during a follow‑up appointment. The decision is never taken lightly.
Quick decision matrix
Feature | Observation | Laser Vitreolysis | Pars Plana Vitrectomy |
Invasiveness | None | Low (outpatient laser) | High (microsurgery) |
Typical cost (AUD) | $0 | $1,200‑$2,000 | $4,000‑$6,500 |
Recovery time | Immediate | 1‑2 days of mild glare | 4‑6 weeks for stable vision |
Success rate for noticeable improvement | 60‑70 % by 8 weeks (brain adaptation) | 30‑40 % reduction in 3‑4 weeks | 90‑95 % removal of target floaters |
So, what should you do next? Start with the low‑effort observation plan. Keep a daily log, protect your eyes from UV, and give the brain a chance to filter. If after three months the floaters still dominate your view, schedule a consult to discuss laser vitreolysis. Reserve vitrectomy for the rare cases where floaters truly block daily activities or are linked to retinal issues.
Remember, every eye is unique. Our Sydney practice tailors the approach to your lifestyle, visual demands and comfort level. A quick call lets us review your journal and map out the most sensible next step.
Conclusion
After reading through everything, you probably still wonder: "floaters after cataract surgery how long do they last?" The short answer is that most people see a noticeable drop within eight weeks, and by three months the specks are usually just background noise.
But if you’re still counting them at six months, that’s a signal to act. New or larger floaters, flashes, or any shadow‑like curtain should prompt an immediate call to your Sydney eye surgeon. Early detection can mean a quick laser seal instead of a more invasive procedure.
What we’ve seen in our practice is that a simple daily wall‑stare, gentle eye‑rolls, and staying well‑hydrated cut the recovery time for many patients. Keep a brief symptom journal – even “few vs many” notes give your doctor concrete evidence.
So, what’s the next step? Log your observations for the next two weeks, protect your eyes from harsh UV, and if the floaters haven’t faded or you notice red‑flag signs, pick up the phone. A quick consult can keep your vision clear and your recovery on track.
Remember, every eye heals at its own pace, but staying proactive gives you the best chance of a smooth outcome. We're here in Sydney to answer any questions and guide you through the next steps.
FAQ
How long do floaters after cataract surgery usually last?
Most patients notice a big drop in specks within eight weeks, and by the three‑month mark the majority are either barely aware of them or have learned to ignore them. In our Sydney practice about 60‑70 % report this improvement. If you’re still counting them after six months, that’s a signal to get checked – the timeline isn’t set in stone, but the brain usually filters them out by then.
Why do some people still see floaters after three months?
Every eye heals at its own pace. A larger clump of collagen or a mild posterior vitreous detachment can keep the shadows in view longer. Lifestyle factors like dehydration or excessive screen time can make the floaters pop out more. Also, the visual cortex needs time to learn what’s harmless; some folks simply need a bit more patience and consistent monitoring.
When should I call my surgeon about floaters?
Call right away if you notice any of these red‑flag signs: new, larger floaters that look like threads, sudden flashes of light, or a shadow/curtain effect in peripheral vision. Even if the specks are still present but have gotten noticeably worse after the typical three‑month window, it’s worth a quick phone call. Early evaluation can catch a retinal tear before it becomes serious.
Can I do anything at home to make floaters disappear faster?
Yes – a few low‑risk habits help. Do a gentle eye‑roll routine (up, down, left, right, then a slow circle) three times a day. Keep a simple symptom journal: note the date, lighting, and a rough count (few, several, many). Staying well‑hydrated and eating omega‑3‑rich foods can keep the vitreous gel supple. These steps won’t magically erase floaters, but they often speed up the brain’s filtering process.
Are there any risks if floaters persist beyond six months?
Persisting floaters aren’t dangerous by themselves, but they can be a clue that something else is happening – for example, a posterior vitreous detachment that’s progressing toward a retinal tear. That’s why we stress watching for flashes or a sudden increase in size. If those appear, the risk shifts from inconvenience to potential vision loss, and prompt laser or surgical intervention may be needed.
How does the brain help filter out floaters over time?
The brain’s visual cortex learns to ignore repetitive shadows, a process called neuro‑adaptation. After cataract surgery, it receives a flood of new visual information, and over weeks it starts classifying the specks as background noise. The more you expose yourself to uniform lighting (like a plain wall) while noting the floaters, the quicker the brain can label them “ignore me.” Consistency is the key.






Comments